Abstract
Australian military malariology has a long but discontinuous history extending back to the Boer War and possibly earlier. Its origins could possibly have been in the Sudan campaign (1885) and more certainly in the
second Boer War (1899–1902) in the years before the establishment of the Australian Army. The discipline has continued, increasingly purposefully during the past half-century, to the present. The continuing struggle of
the Australian Defence Force against malaria is now led by the Australian Army Malaria Institute (AAMI), the forerunner of which, the 1st Malaria Research Laboratory (1MRL), was founded in June 1966.
The Army’s anti-malaria effort has typically been led by officers of the Royal Australian Army Medical Corps;however, particular distinguished civilian malariologists have also influenced the directions taken by Australian
military malariology.
This article is the first in a proposed series that will trace the careers of about 20 Australian malariologists who have made significant, pioneering contributions to the development of their discipline. As the AAMI will be able
to celebrate the 50th anniversary of the formal establishment of the 1MRL on 14 June 2016, such a series is timely. Later articles in the series will demonstrate how the AAMI has grown from humble, even inauspicious
origins as the 1MRL to become a leading malariological research agency.
Introduction
Malariology was a late developing discipline in Australia. Although much of tropical Australia was still malarious after Federation, with localised seasonal outbreaks of malaria, the first professionally trained malariologist did not begin work in Australia until 1909. The late development of the discipline probably reflected demographics. Northern Australia was sparsely settled; the population centres there were small and widely dispersed; and the great bulk of the national population lived in the non-malarious south, where other infectious diseases demanded the attention of medical scientists.
Australia’s early military involvements, especially in particular theatres during World War I, provided impetus for the development of Australian malariology. The Army experienced its first epidemics of malaria in 1914–1915 in New Guinea and in 1918 in Syria. Many of the Army’s medical officers treated their first cases of malaria during those campaigns. Some went on to specialise in malariology. Others, specialists in other branches of medicine, nevertheless took continuing interest in the disease after treating it during overseas military service.
The Army’s experience of malaria was consequently the background from which Australian malariology emerged.
One way of conceptualising the development of Australian malariology is to view it through a ‘biographical prism’, that is to trace the growth of the discipline through the experience of the Army officers who treated malaria cases during the happenstance of military service.
This article takes that approach by recounting the careers of five Australian Army officers and one civilian who were confronted by the realities of malarial outbreaks among soldiers in the field. In broadly chronological order they were Sir William D.C. Williams, Dr Anton Breinl, Colonel Cecil L. Strangman, Major-General Rupert M. Downs, Lieutenant George G. Grant and Sir Raphael W. Cilento. The article now profiles them in that order, showing how they each contributed to an expanding corpus of Australian knowledge about malaria during the period 1900–1924.
Sir William Duncan Campbell Williams (1856–1919)
William Duncan Campbell Williams, the son of an English-born medical practitioner, was born in Sydney on 30 July 1856. After completing his schooling at Sydney Grammar School, he studied medicine at University College, London. On graduating he undertook a one-year internship at the college hospital before returning to Sydney, where he practised in Darlinghurst1.

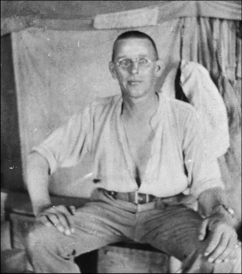
Surgeon-Major W.D.C. Williams, Principal Medical Officer
of the Sudan Contingent of 1885, seen here 11 years later
in 1896, three years before he served as Principal Medical
Officer of the New South Wales force sent to the Boer War.
(Australian War Memorial [AWM] picture no. H13980.)
Williams became a captain the New South Wales Artillery in 1883 and was soon promoted to major. He led the medical units accompanying the New South Wales Sudan Contingent in 1885.
Williams was not a malariologist as such, but as the udan Contingent’s Principal Medical Officer (PMO), he was probably the first Australian military medical officer to become responsible for treating cases of malaria among Australian troops in the field — 13 years before the causes of malaria and its mosquitoborne transmission were understood. At that time the Australian medical profession still thought that ‘malaria bacteria’ infested swampy areas, where they were readily picked up by humans. In the Sudan the Australians suffered from a malaria-like relapsing fever, which Williams treated effectively with quinine.
Back home in Sydney, Williams was appointed PMO of the NSW army forces. During the period 1888–91 he reorganised the army medical services, introducing a well-trained permanent Medical Staff Corps. The Corps was equipped with improved light ambulance wagons of Williams’s own design, lightweight stretchers, mounted stretcher bearers and an intensive training program for Corps members.
At the outbreak of the second Boer War in 1899 Williams mobilised two contingents of the NSW Army Medical Corps. He accompanied them as a colonel. Williams’s highly mobile medical units, which could keep up with the forward troops, provided an excellent service. They became the model from which the Australian Army’s field ambulance system of World Wars I and II developed.
In 1900 Williams was appointed PMO of the Australian and New Zealand forces in South Africa. His work in South Africa earned him promotion to surgeon general and the award of the CB (Companion of the Most Honourable Order of the Bath).
By this time the causes of malaria had been determined. In the period 1897–1899 Ronald Ross’s research in India and Giovanni Battista Grassi’s experiments in Italy, building on the 1880 studies of Charles Louis Alphonse Laveran in Algeria, had demonstrated that malaria was caused by various species of Plasmodium, a blood parasite transmitted by female mosquitoes of the Anopheles genus.
Surgeon-General W.D.C. Williams at Heliopolis, Cairo,
Egypt, February 1915 (Australian War Memorial
photograph no. P11235.030).
The infectious diseases most commonly suffered by Australian troops during the second Boer War were typhoid and dysentery; however, among the 286 Australian deaths from disease during the war, malaria was a factor. Where it was diagnosed, it was treated with quinine.
In 1902 Williams was an obvious choice for appointment as the Australian Army’s inaugural Director General of Medical Services (DGMS). His early achievements in the position included the drawing together of the disparate former colonial military medical services into the Australian Army Medical Service and the establishment of the Australian Army Nursing Service in 1903.
At the opening of hostilities in World War I in August 1914, Williams, who was widely known by the nickname ‘Mo’, sought and was granted appointment as the Director of Medical Services (DMS) of the Australian Imperial Force (AIF) to be dispatched overseas. His commanding officer, Major-General Sir William Bridges soon came to regret the appointment however. Aged 58, greatly overweight and physically unfit, Williams was in poor shape for the rigours of the campaigns ahead. He impressed Bridges poorly by regarding the voyage to Egypt as a holiday cruise.
Bridges increasingly relied instead on Williams’s staff officer, the dynamic Lieutenant-Colonel Neville Howse VC.
Instead of remaining in Egypt with the AIF, Williams travelled on to London, where he did useful work procuring motor ambulances, medical equipment and pharmaceutical supplies for the AIF’s medical units. Returning to Egypt in February 1915, he was greatly embarrassed to find there was no command position he could fill or worthwhile work to do. In addition, he was reduced to Deputy DMS (DDMS) status while his former protégé, Howse, was being advanced upwards through the Australian Army Medical Corps (AAMC) hierarchy. (Later in 1915 Howse was promoted to major-general and moved into the DMS position.)
Isolated, on 25 April 1915 — the day of the Gallipoli landings —Williams returned to London to arrange the shipment back to Australia of AIF convalescents and invalids. At Malta on his way back to Egypt he received a telegram saying that his services were no longer required in Cairo. He was ordered back to London, where he was attached to the Australian High Commission but with few responsibilities or duties to perform.
After Howse transferred his base as DMS of the AIF from Cairo to London in April 1916, Williams returned home in failing health and greatly resentful of his treatment. He was knighted in June 1916 soon after his return. He retired from the Army in early 1917. He had less than 2½ years left to enjoy his retirement and the honour and prestige of his KCMG. He died of heart disease in May 1919 in Melbourne, where he was buried with full military honours.
Despite the frustrations of his World War I career, Williams had been a great innovator and a superb administrator of military medical services in both peace and in the three wars in which he had served. His great achievement had been to create the Australian Army Medical Services and then to mobilise them for war in 1914. Another achievement, of course, had been to institute effective treatment regimens for the Army’s early malaria victims in the wars in the Sudan and South Africa.
Dr Anton Breinl (1880–1944)
Anton Breinl was born in Vienna , Austria. His family was from Pilsen, at that time in the German-speaking province of Bohemia of the Austro-Hungarian Empire but nowadays in the Czech Republic and called Plzen. After schooling in Komotau (present-day Chomutov), he studied medicine at the University of Prague, graduating in 19042.
Dr Anton Breinl, 1910, State Library of Queensland.
Soon after his graduation, Breinl moved to England to study at the Liverpool School of Tropical Medicine. He became an ‘International Fellow’ in bacteriology at the school, working under Sir Ronald Ross, discoverer
of the causal link between malarial infection and the bite of a Plasmodium-loaded mosquito. In 1905 Breinl accompanied the school’s Yellow Fever Expedition to Brazil, where he contracted the frequently fatal disease but survived. After returning to England he continued his research at the Runcorn Research Laboratory, of which he was appointed director in 1907.
In 1909 Breinl migrated to Queensland to become the inaugural director of the Australian Institute of Tropical Medicine (AITM) at Townsville. He spent the next 11 years at the AITM, building it up into a wellrespected
research organisation. During his time there, he undertook extensive research expeditions in Queensland, the Northern Territory and Papua. In that time the AITM demonstrated its effectiveness by publishing 22 pioneering scientific research papers. Personally, Breinl established a deserved reputation as Australia’s first great malariologist.
Breinl also applied his expertise in tropical diseases by treating their victims in the Townsville General Hospital. It was there that he treated the troops of the Australian Naval and Military Expeditionary Force who had fallen victim to malaria during their capture of New Guinea in 1914–15 and had been repatriated to Australia. He described their treatment regimen in a long and authoritative article in the Medical Journal of Australia in January 1916. Co-authored with an AITM colleague, Dr (later Professor) Henry Priestley, this was titled simply ‘Malaria contracted in New Guinea by members of the Expeditionary Force and its treatment’3.
Breinl had become a naturalised Australian in 1914 before the outbreak of World War I; and in 1919 he married an Australian nurse. (Two of their three sons became Australian medical practitioners.) He tried unsuccessfully on three occasions to enlist for war service as an Australian Army Medical Corps (AAMC) officer but was rejected each time. While continuing his own AITM research throughout the war, he also served as the non-salaried superintendent of the Townsville General Hospital when the former salaried incumbent departed after enlisting in the AIF.
Despite his outstanding service to the citizens of his adopted country, Breinl suffered social ostracism throughout the war because of his Austrian background and his self-evidently German surname. Because of xenophobic anti-German-Austrian vilification that many German-speaking Australians had to endure during the war, people like Breinl became the victims of hurtful speculation about their loyalties to Australia.
Breinl eventually quit the AITM in 1920 to retreat into successful private medical practice. He was probably pressured into resigning from his position because of his Austrian origins. His colleague Henry Priestley, who later held the chair in biochemistry at the University of Sydney, described Breinl’s departure from the AITM as ‘a great tragedy’ because it deprived Australian medical research of his vast knowledge of tropical diseases.
The Australian Institute of Tropical Medicine, Townsville,
1910, the year after Dr Anton Breinl, became its inaugural
director. (Photograph from the Queensland Historical
Atlas website www.qhatlas.com.au/.)
Breinl lived in Australia for the rest of his life. He died in Sydney of renal failure in June 1944, eleven months before World War II ended in Europe. His contribution to the development of tropical medicine in Australia was belatedly commemorated in the naming of the Anton Breinl Centre for Public Health and Tropical Medicine of the James Cook University in Townsville.
The Anton Breinl Centre was established in 1987 in the original AITM building. It adopted Breinl’s name in 1990. The next year it became the base for a new professional organisation, the Australasian College of Tropical Medicine. At the time this profile was written, the Anton Breinl Centre was one of only eight internationally recognised centres of excellence in tropical medicine.
Colonel Cecil Lucius Strangman (1867–1942)
Major Cecil Lucius Strangman (1867–1942) was an Irish-born and trained AAMC surgeon from Adelaide who had migrated to South Australia in 18904. He was the fourth of nine children. As well as he a brother and two sisters became medical practitioners. In 1907 he moved to Darwin as the Government Medical Officer and Protector of Aborigines5.
Strangman served in Darwin for six years 1907–1913 and proved a popular appointment among the town’s racially diverse residents. The Acting Administrator of the Northern Territory regarded him as ‘a most capable officer’6. Elsewhere, the Acting Administrator wrote that Strangman’s presence in Darwin had been an ‘incalculable advantage to the Territory’ as he was ‘so skilled…in tropical medicine’. Further, ‘many lives [had] been saved by reason of [his] education in tropical diseases’7.
Twice during his time in Darwin, in 1908 and 1912, Strangman spent six-month periods studying at the London School of Tropical Medicine under Sir Patrick Manson, one of the great pioneers of parasitology8. Strangman’s qualifications included Fellowships in the Royal College of Physicians of Edinburgh and the Royal College of Surgeons of Edinburgh and a Diploma in Tropical Medicine and Health from Cambridge University awarded in 19129.
After leaving Darwin, Strangman returned to Adelaide, where he enlisted as a captain in the AAMC in September 1914. He had previous militaryexperience in militia units, as a surgeon with the South Australian Mounted Rifles, the 17th Light Horse and the 4th Field Ambulance10. In October 1914 he was promoted to major and three weeks later was assigned to the 3rd Battalion of ‘Tropical Force’11. Commanded by Brigadier (later Sir) Samuel
Pethebridge, this formation was sent to New Guinea aboard the ship Eastern at the end of October 1914. Its task was to support and relieve the Australian Naval and Military Expeditionary Force (ANMEF), which had occupied the German possessions there during September–October 1914. Strangman became the Tropical Force PMO12.
In Rabaul Strangman took over from the previous PMO of ANMEF, Arthur Maguire (a later DGMS), in early January 191513. This was midway through the first malaria epidemic ever suffered by Australian military forces. The epidemic had begun in December 1914, with the onset of the wet monsoon season. Maguire dosed the troops with quinine but the two hospitals, at Rabaul and nearby Herbertshöhe, ‘filled rapidly’ according to the official war historian, S.S. Mackenzie, who described the epidemic in his volume The Australians at Rabaul14.
In one week in January 1915, 36 troops of the Rabaul garrison were admitted to hospital suffering from ‘benign tertian’ or vivax malaria, with another 238 troops being treated as out-patients15. Two of the malaria victims died. Both had what the previous PMO described as ‘meningeal symptoms’, i.e. cerebral malaria. Two more victims died after being repatriated to Australia in February 1915. They had contracted what was then known as ‘malignant tertian’ malaria, now commonly called falciparum malaria16. Troops sent to outposts such as Madang, Kavieng, Angoram and Kieta also suffered malaria and some died. One victim died of the falciparum malaria complication, blackwater fever, and was buried at Kieta on the east coast of Bougainville17.
Mackenzie wrote that as Strangman took over from Maguire he faced ‘an ugly menace and the next three months were anxious ones18.’ In treating the malaria victims, Strangman administered quinine in four hourly dosages for ten days and thereafter three times weekly. The quinine was taken in a solution of hydrochloric acid — a nauseating concoction loathed by those receiving it. To make it more palatable, each dose was followed by a tot of rum. Somewhat perversely, Strangman refused to administer the quinine in tablet form, which he believed was ineffective for people not acclimatised to the tropics.
Strangman took it upon himself to conduct a ‘crusade’ against malaria, especially in Rabaul and Madang, towns which the medical officers regarded as ‘hotbeds’ of the disease19. According to Mackenzie, ‘during those anxious months, when the lives of the whole garrison were in his hands’, Strangman saw his patients daily and spent the rest of his time at the microscope examining their blood slides. ‘His brusque, kindly manner and his trick of plain speaking’ inspired confidence and endeared him to them20.
Brigadier Sir Samuel Pethebridge, his staff officers and heads of ANMEF administrative departments, Rabaul, 1917. Pethebridge is fifth from the left in the front row; him PMO, Strangman ( inset), is next to him, fourth from the left. ( AWM photo no. H15071.
Under Strangman’s management, the epidemic was brought under control by mid-February 1915 and subsided with the end of the wet season in March. In the meantime, Strangman had instituted a vigorous mosquito control program. He discovered that rainwater accumulating in the hollows between the trunks and branches of the decorative poinciana trees planted along Rabaul’s avenues were prime mosquito breeding sites, so he had them filled with concrete. Any outside receptacles in which rainwater could accumulate were destroyed. He also had layers of kerosene poured on top of the water in all the domestic rainwater tanks around the town to suffocate the mosquito larvae; he then had the water microscopically examined every fortnight to ensure that the tanks were not becoming breeding grounds21.
With the malaria epidemic under control and vigorous mosquito eradication measures in place, Strangman was promoted to lieutenant-colonel in March 1915 and then to colonel in July 1916. He remained in Rabaul as the PMO until June 1917. He had held the position for 2½ years, the longest period of any who ever held it. As PMO he was also the head of the Medical Department in Pethebridge’s military administration of the former German
colony. During Pethebridge’s absences from Rabaul while visiting outstations, Strangman twice served as Acting Administrator22.
Strangman’s war took an unexpected turn in early August 1917 as he was sailing back to Rabaul from Sydney after seven weeks’ furlough. He was due to succeed Pethebridge as ANMEF commander. (Pethebridge had been repatriated ill to Melbourne. He died there of malaria in January 1918.) Strangman, however, never returned to Rabaul. His ship, the Matunga, apparently vanished without trace during the voyage, At first the vessel was thought to have sunk with all aboard, but then the military authorities in Australia learned that the German raider Wolf had captured the Matunga and taken those aboard prisoner. In early February 1918 Army headquarters (HQ) in Melbourne advised Strangman’s wife in Adelaide that he was now a prisoner of war (POW)23.
The Wolf had intercepted the Matunga only 12 hours’ sailing time from Rabaul on 6 August. The raider then escorted the Matunga to Netherlands New Guinea. The Germans took the Matunga’s crew and passengers aboard, then sank the ship with shellfire, torpedoes and bombs. After that the Wolf made its way across the Indian Ocean and north up the Atlantic to Kiel, its home port in Germany, laying mines and sinking ships en route24.
Colonel Cecil L. Strangman (left) and other ‘top deck’
prisoners of the German raider Wolf. (From Richard
Giulliatt and Peter Hohnen, The Wolf: How One German
Raider Terrorized Australia and the Southern Oceans in
the First World War, William Heineman Australia, 2009.)
After reaching Germany, the ex-Matunga personnel were mostly sent to POW camps, where they spent the rest of the war. That was not to be Strangman’s destiny, however, because in early March Army HQ in Melbourne received word from London that he had been sent to Denmark and from there to England. He spent three months in hospital and convalescence in London. After his discharge from hospital he was temporarily attached to an orthopaedic hospital and then spent a brief period on active service in France. He eventually departed England for Adelaide in October 1918. His appointment was terminated there in February 1919. After returning to civilian life he seems to have lived and practised in Lower Mitcham, a southern Adelaide suburb25.
Little is actually known of Strangman’s life, apart from what might be gleaned from several files on him in the National Archives of Australia and the references to him in the official war histories. These, however, are sufficient to demonstrate that that he was the first formally trained and qualified malariologist to serve in the Australian Army.
Without his enterprising malariological work in New Guinea 1914–1917, the number of deaths from malaria among ANMEF troops could well have been much higher than the official tally of five.
Major-General Rupert M. Downes (1885–1945)
Rupert Major Downes was born in Adelaide, where his parents had settled in 1877. His father, Colonel Francis Major Downes, a former Royal Artillery officer with Crimean War experience, had come to Adelaide when appointed commandant of the South Australian defence force. In 1885 Downes Snr. moved to Melbourne as commandant of the Victorian defence force. He later presided over the transfer of the defence force to Commonwealth control at Federation in 1901. He retired as a major-general in 190226.
Rupert Downes received most of his schooling at Haileybury College, Brighton, a Melbourne suburb, where he was Head Boy. He joined the militia as a trumpeter while still at school and was one of the trumpeters who played the fanfare at the opening of the federal parliament in Melbourne on 9 May 1901. The next year he began medical training at the University of Melbourne. After graduating he was commissioned as a captain in the Australian Army Medical Corps (AAMC) in 1908. In the years that followed he specialised in surgery and completed a Doctor of Medicine (MD) degree.
Downes enlisted in the AIF at the outbreak of World War I in 1914 and was immediately promoted to lieutenant-colonel and given command of the 3rd Light Horse Field Ambulance, a unit he raised, trained and then led at Gallipoli. He subsequently served as Assistant Director of Medical Services of the Anzac Mounted Division 1916–17 and then as Deputy Director of Medical Services (DDMS) of Lieutenant-General Sir Harry Chauvel’s Desert
Mounted Corps 1917–1918.
In the latter position Downes instigated and oversaw a vast and intensive mosquito control program in the lower Jordan valley in the period May–September 1918. This work was necessary to protect the Desert Mounted Corps from malaria after the Corps camped near Jericho for the summer of 1918. At the time, the low-lying, swampy valley was among the world’s most malarious regions. The program entailed largescale engineering works to drain the swamps, clear away the tangled thickets of vegetation sheltering mosquito breeding sites, remove the algal growths harbouring mosquito larvae, dig a network of drainage channels and straighten the courses of the numerous meandering wadis to speed up the stream flow entering the Jordan. Meanwhile, any troops succumbing to malaria were immediately evacuated to the military hospitals in Gaza and Egypt, where they could be treated without risk of passing the disease on to their comrades27.
Colonel Rupert Downes as Deputy Director of Medical
Services of the Desert Mounted Corps 1917–18. As DDMS
he had to manage a catastrophic malaria epidemic in
Syria in October 2018. (AWM photograph no. A02728.)
These measures succeeded in keeping malaria infection rates among Desert Mounted Corps personnel at relatively low levels during the summer the Corps was obliged to spend in the Jordan valley. The average weekly malaria evacuation rate across the 19 weeks the Corps spent in the valley May– September 1918 was only 0.84 percent of Corps strength; and in no week did it exceed 1.4 per cent.
Canalisation of the Wadi el Auja by Sikh pioneers
(engineering support troops), lower Jordan valley, 1918.
The working party is straightening the stream course
and lining the banks with rock. (AWM photograph no.
A00328.)
Unfortunately, however, as soon as the Corps quit the valley in September 1918 to spearhead the Allies’ rapid advance into Syria in September 1918, the troops entered malarious regions where no control work had been carried out. A catastrophic epidemic of falciparum malaria erupted soon after the Corps occupied Damascus on 1 October, striking both the Allied forces and their Ottoman (Turkish) foes simultaneously. Complicating and exacerbating the epidemic was the arrival of the worldwide pandemic of pneumonic or ‘Spanish’ influenza of 1918–1919. Many soldiers on both sides suffered falciparum malaria and pneumonic influenza simultaneously. The tsunami of disease effectively halted the war. An armistice between the combatants ended the war in the Middle East on 31 October, but by then the war in Syria had almost ground to a stand-still.
The scale of the emergency was obvious in the campaign statistics. The Desert Mounted Corps suffered relatively light battle casualties of 149 killed, 49 missing and 438 wounded during the six-week advance from the lower Jordan to Damascus and then north to Aleppo; but during the same period the Corps’ medical units treated 11,300 sick or 41 per cent of Corps strength28. All available hospitals were soon overflowing with the sick. In Damascus, for instance, the medical units took over the missionrun ‘French’ and ‘English’ hospitals, which together had 247 beds; but within a few days they were accommodating 625 patients29.
When the actual malaria figures for the Allies’ final seven-week offensive were eventually compiled, they provided an astonishing view of the hazards that malaria had presented. For the Desert Mounted Corps the total number of malaria cases confirmed by blood slide testing was 6347 or 22 per cent of average Corps strength of 28,850 men30. As for the mortality that malaria had inflicted, for the whole Allied force the total was 865 deaths or one in 370 for the entire force. For AIF soldiers the rate was almost twice as bad: 101 AIF members died from the disease, a rate of one death from malaria for every 174 soldiers31. Malaria had proved almost as lethal as the fighting for the Australians.
As the Corps DDMS, Rupert Downes was responsible for managing this disaster, even though he, too, suffered a debilitating attack of malaria himself — as did many of his medical colleagues as well. Before the war Downes probably had little experience of malaria. A surgeon, he was above all else a superlative military-medical administrator. It was his systematic approach to the malaria problem combined with his organisational skills and his close working relationship with his commanding officer, Chauvel, which enabled him to tackle effectively the huge challenge that malaria posed for the Desert Mounted Corps.
Post-war, Downes became a leading paediatric surgeon in Melbourne but he also continued his AAMC service part-time as DDMS of the 3rd Military District (Victoria). He returned to full-time military service when appointed DGMS and promoted to major-general in 1934. His great achievements as DGMS included mobilising the Army medical services for war in 1939 and instituting and presiding over the construction of the great military base hospitals in Australia’s mainland capital cities — Heidelberg (in Melbourne), Concord (Sydney), Greenslopes (Brisbane), Daw Park (Adelaide) and Hollywood (Perth).
After retiring from the Army in 1944, Downes was appointed as Australia’s official medical historian for World War II. His main qualification for this position was the book-length account of the campaigns in Sinai, Palestine and Syria he had contributed to the first volume of A.G. Butler’s official medical history of World War I, The Australian Army Medical Services in the War of 1914–191832. Downes was unable to complete his proposed World War II history because he died in a plane crash several months after beginning the project. On 6 March 1945 he was flying to New Guinea with Major-General George Vasey, Commander of the 6th Division 2nd AIF, when their Lockheed Hudson aircraft plummeted into the sea off Cairns, north Queensland, killing all eleven servicemen aboard.
Major-General Rupert Downes as Director General
of Medical Services of the Australian Army, 1939: his
passport photograph. (From Ian Howie-Willis, Surgeon
and General: A Life of Major-General Rupert Downes
1885–1945, Australian Military History Publications,
2008.)
Cecil Strangman, a malariologist, had effectively managed the Army’s first malaria epidemic, in 1914–1915. Rupert Downes, a non-malariologist, managed the next, four years later. As the statistics above indicate, the epidemic confronting Downes was on a calamitous scale. The 101 deaths from malaria over a seven-week period represented the highest mortality from the disease ever suffered by the Australian Army in its entire history. Without Downes in situ to manage the disaster, the mortality might have been much higher. His success in reining in the epidemic earned him a well-deserved place on Australia’s malariological ‘honour roll’.
Lieutenant George Gordon Grant (1873–1918)
In combatting the malaria epidemic in Damascus in October 1918, Colonel Downes was fortunate in having ready access to a remarkable scientific testing service. This was the Anzac Field Laboratory, a mobile unit established in Egypt in August 1916 to assist in the desert campaigns being fought by British-led forces against the Ottoman armies in Sinai and Palestine. The Laboratory’s function was to conduct pathological tests to determine what infectious diseases the troops were suffering. Staffedby various Australian, New Zealand and British medical officers and laboratory technicians, by 1918 it had a staff of 11, two of whom actually died from malaria33.
The Laboratory performed an essential service for the Allied forces during the 2½ years of its existence. It conducted no fewer than 32,390 separate tests. Among these were 17,431 blood slide examinations for malaria, of which 4312 yielded positive results. During the Desert Mounted Corps long summer in the Jordan valley in 1918, the laboratory moved to Jericho. While there, it undertook mosquito surveys and microscopically identified mosquito species as well as doing blood slide analysis. In addition to that work, it performed a critical role during a malaria and influenza epidemic in Amman in Jordan in September-October 1918, which coincided with the disastrous epidemic in Damascus. The Laboratory later moved to Syria and was based in Aleppo.
One of the Laboratory’s malaria victims was Lieutenant George Gordon Grant (1873–1918), its head. Grant had been born in Hadlow, Kent, England, but had migrated to Australia. A civil servant, he had enlisted in the AIF in May 1915 at the age of 42, which was old for a recruit. He was appointed staff sergeant and posted to the 3rd Australian General Hospital (3AGH) at Mudros on Lemnos Island during the Gallipoli campaign34.
After falling ill with jaundice, in December 1915 Grant was sent to England for treatment. He spent two months in hospital in Woolwich then in March 1916 he was sent back to the 3AGH, which had relocated to Abbassia near Cairo. He remained with the 3AGH until posted to the Anzac Field Laboratory when it formed in August 1916. Initially appointed as the Laboratory’s quartermaster, he continued working with the unit until his death two years later.
In October 1917 Grant was promoted to lieutenant and given command of the Laboratory. He was mentioned in despatches in June 1918 for ‘devotion to duty’. At that time he was with the laboratory in Jericho, where he fell ill with malaria in August 1918, a month before the thrust north into Syria. He was evacuated to a hospital in Gaza on 26 August but by 30 August he was reported as being ‘dangerously ill’ with malignant tertian (falciparum) malaria. He died the next day and was buried in the war cemetery at Gaza.
George Grant did not live to see the crucial part his Anzac Field Laboratory would play during the great malaria epidemic in Damascus in October 1918. The tests conducted by the Laboratory during that crisis enabled the medical officers of Desert Mounted Corps to determine which troops were suffering from malaria, from influenza or from both diseases. That in turn enabled them to plan the prophylactic regimens, treatment methods and evacuation strategies put in place to combat the epidemic.
Lieutenant George Gordon Grant, one of the original staff
of the Anzac Field Laboratory on its formation in August
1916. He became Officer-in Charge of the unit in October
1917. He died in Palestine from falciparum malaria in
August 1918. (AWM photograph no. B02851.)
Grant was neither malariologist nor medical officer but an administrator. The pathological testing and mosquito identification routines of the Anzac Field Laboratory that he helped implement nevertheless enabled Rupert Downes and his fellow medical officers to tackle malaria effectively. For that achievement Grant earned his ‘honourable mention’ in the history of Australian military malariology.
Sir Raphael West Cilento (1893–1985)
Raphael West Cilento was born in Jamestown, South Australia, on 2 December 1893. Known in his childhood as ‘Ray’, he was the son of a railway stationmaster whose father had been an Italian immigrant. After primary schooling in Jamestown, Ray became a pupil teacher and taught in Port Pirie before completing his secondary education at Prince Alfred College. He then entered medical training at the University of Adelaide, from which he graduated in November 191835.
On graduating, Cilento enlisted in the AAMC as a captain and was immediately posted to Rabaul, the capital of German New Guinea. He served there as a medical officer with ANMEF, the Australian occupying force. He spent only ten months in New Guinea, but his experiences there aroused his interest in tropical medicine. He later contributed the final chapter to the first volume of A.G. Butler’s official history, The Australian Army Medical Services in the War of 1914– 191836. This dealt with ‘Tropical Force’, which had supported ANMEF, the military agency which had occupied New Guinea and was then responsible for civil administration in the former German colony37.
Returning to Adelaide, in March 1920 Cilento married Dr Phyllis McGlew (1894–1987), who had been in his graduating class at university. They had six children, four of whom became medical practitioners, but Phyllis continued practising medicine independently for the rest of her long life. Interested in paediatrics, obstetrics and nutrition, she became an authority on mothercraft, on which subject she published a series of books. As a newspaper columnist, writing under the nom de plume ‘Medical Mother’, she became one of Australia’s most widely read medical practitioners38.
After their marriage, the Cilentos took up positions as medical officers in the Perak sultanate in northern Malaya. They returned to Australia in 1921 after Ray had been offered a position at the Australian Institute of Tropical Medicine (AITM) in Townsville. The appointment required him to complete a Diploma in Tropical Medicine and Hygiene at the London School of Tropical Medicine. After completing this qualification and also graduating as a Doctor of Medicine (MD) at the University of Adelaide, in 1922 Cilento was appointed as director of the AITM. As such, he became one of Australia’s few authoritieson tropical diseases. In 1924 he published the first book on malaria by an Australian — Malaria, with Especial Reference to Australia and its Dependencies — and he also published a series of articles on the disease in the Medical Journal of Australia39.
In 1924 Cilento returned to Rabaul on secondment as the director of public health for the Australian controlled League of Nations Mandated Territory of New Guinea. He spent four years in the position before taking up a Commonwealth government position as Director of Tropical Hygiene and Chief Quarantine Officer for north-east Australia, based in Brisbane. In 1934 he transferred to Canberra but after a year there he returned to Brisbane as the first State Director-General of Public Health and Medical Services. As the job required the preparation of legislation, he studied law and was admitted to the Bar in 1939. He retained his director-general’s position until 1945. His achievements as directorgeneral had earned him a knighthood in 1935.
Dr Raphael (‘Ray’) Cilento in 1923, the year after he
became the director of the Australian Institute of Tropical
Medicine at Townsville. (Picture Queensland Connections
photograph no. #197735.)
During the 1930s Cilento was also a leading advocate for the establishment of a medical school at the University of Queensland. When it opened in 1936 he was appointed as its inaugural Professor of Social and Tropical Medicine. This appointment was one of the first in the world using the title ‘Social Medicine’. He held the position for ten years.
During World War II Cilento was prevented from serving with the AAMC or otherwise contributing to the military effort because the Commonwealth security services were suspicious of his Italian heritage and his alleged sympathies for the Fascist regime in Italy. In May 1945, however, he began working for the new United Nations Relief and Rehabilitation Administration (UNRAA) on malaria control in the Balkans. He was then appointed UNRAA director in the British zone of occupied Germany. In 1947 he moved to New York as the foundation Director of the UN’s Social Activities Division, an agency which developed UN social policy. In 1948 he served as the UN’s director of disaster relief in Palestine.
After resigning from the UN in 1950 Cilento returned to Queensland but was unable to secure either a government or an academic appointment in keeping with his distinguished career in tropical medicine and public health. Instead he entered part-time private medical practice, which he combined with various public activities. These included long-term commitments to the Royal Historical Society of Queensland and the National Trust of Queensland, in each of which he served as president. In addition he stood twice a candidate for election to the federal parliament but was unsuccessful both times.
Sir Raphael Cilento, 1945, John Oxley Library, State
Library of Queensland.
With the journalist Clem Jack in 1959 Cilento published Triumph in the Tropics, an ‘historical sketch’ of Queensland which became a best-seller. Unfortunately the book contained disparaging references to Aboriginal society that reflected the patronising views of an earlier era. A firm supporter of the ‘White Australia’ policy, Cilento deplored the presence in Australia of immigrant communities from Australia’s near neighbours in the Pacific Islands, whom he believed were of ‘inferior’ racial stock. In later life he controversially aligned himself with the extreme right of Australian politics, as represented by the Australian League of Rights.
Despite the controversies that Cilento’s political and racial views aroused, with Anton Breinl he remains one of the two ‘founding fathers’ of Australian malariology. His work in the epidemiology of malaria in Australia was the first of its kind and it prompted both State and Commonwealth government public health authorities to act decisively in containing the disease. As one observer later remarked, Cilento was not only both brilliant and eccentric but he helped rid northern Australia of malaria.
Conclusion
The above biographical profiles— of Williams, Breinl, Strangman, Downes, Grant and Cilento — provide a window on the early development of Australian malariology. That development was stimulated by the Australian Army’s involvement in the overseas military campaigns of the early twentieth century, especially in South Africa, New Guinea and the Middle East.
Particularly during World War I, the AAMC medical officers who supported the campaigns in New Guinea, Egypt, Palestine and Syria learnt much about malaria, its treatment and its prevention through both chemical prophylaxis and mosquito control measures. Few of them could be described as malariologists. Most, however, had realised the military significance of high malaria infection rates among Australian soldiers. That understanding would underpin the Australian Army’s anti-malaria effort in the next major conflict, World War II.