Introduction
THIS IS THE FIRST OF A TWO-PART ARTICLE on English naval medicine during the Tudor period, from the end
of the Wars of the Roses in 1485 until the death of Elizabeth I in 1603. Both parts follow an article on medieval naval medicine and have the same aim of making comparisons with contemporary ADF practice, in order to identify com mon issues.
Like the previous article, they are based on the first of a four-volume history of naval medicine, written by Surgeon Commander J.J. Keevil RN (Rtd) in the late 1950s.2 However, it has been possible to update Keevil’s work, following the salvage of the 600 ton Tudor warship Mary Rose. The Mary Rose sank off Portsmouth on 19 July 1545, after she flooded through her gun ports whilst in action against a French fleet. There were only about 35 survivors out of 700 men, compared to her normal complement of 400, suggesting the Mary Rose was overloaded when she sank. The wreck was rediscovered in 1971 and raised in 1982.
This part describes Tudor medicine from a naval viewpoint and Tudor ships from a medical viewpoint. The second part will discuss the medical aspects of Tudor naval operations.
BACKGROUND
Early 16th century England had about 2.5 million people, suggesting a small population increase for the first time since the 1345-1348 Black Death and the Wars of the Roses. Most were rural dwellers, with London having only about 60,000 people. As it is estimated that there were only about 5,000 English mariners at this time, the English lacked the need and the resources to make any special provision for the health care of seamen, apart from the Laws of Oleron!
After 1450, the sons of English noblemen began to join merchant-adventurer companies instead of religious orders. The ensuing fall in the number of novices, combined with the reduced endowments by those who were becoming more concerned with material rather than spiritual gain, led to the decline of the charitable ‘houses of pity’ that provided health care for the masses during the Middle Ages.
The end of the Middle Ages was a time of considerable economic disruption and unemployment, such that from 1493, begging licenses were issued to scholars, soldiers and seamen in order to control vagrancy. Municipalities and parishes were made responsible for dealing with the poor, while the drift to the cities was addressed firstly by the forced return to the parishes and later by punishing unlicensed beggars.
Although Henry VIII’s war with France and Scotland in 1512-13 temporarily solved the unemployment problem, it rebounded thereafter and was further exacerbated by his dissolution of the religious orders after 1537. In the 1530s, it was estimated that England had about 800 religious communities totalling about 10,000 people.3 Henry’s dissolution of these communities was based on political expediency, the lure of material gain, and abuses by the religious orders themselves. His takeover of their revenues led to the closure of nearly all the charitable institutions, including the seamen’s hospitals or ‘masyndews’. It is estimated this left England with only about 5,000 hospital beds for the entire population.3 Although his father, Henry VII, had left £6666 in his will for the
first English military hospital at the Savoy in London, it was not completed until 1517 and, in any case, only had 100 beds. After Edward VI appointed some of the Savoy Hospital’s revenue for other hospitals, it was always in financial difficulty and its dissolution in 1702 ended the religious medical outlook of the Middle Ages.
After the 1550s, the parishes began funding their own hospitals, with supplementation from lay benefactors, the privy purse, and levies, such as those on ships entering Bristol for the local mariner’s hospital. One benefactor was Sir John Hawkins, who received a licence in 1594 for England’s first naval hospital, a ten-bed facility at Chatham. However, it was only after a 1597 Act allowed benefactors such as Hawkins to make donations without royal approval, that English hospitals could provide even the basic medical care that was previously offered by the medieval religious orders.
The Tudor wars were therefore fought with minimal provision for medical care for anyone, let alone soldiers and sailors. One effect was to lay the whole English population open to epidemics of plague, typhus and intestinal infections.2 Evidence from human remains recovered from the Mary Rose certainly suggests that the standard of Tudor health care was poor. Excavating the wreck showed that her crew had been trapped at all levels throughout the ship but, not surprisingly, had tended to congregate near the companionways. Although they were completely mixed together, over 90 skeletons were partly reconstructed, by matching paired lower limb bones with pelves and spines and using forensic dentistry to match skulls with mandibles. It was estimated the remains represented between 100 and 300 individuals.
As might be expected, no women were identified and most of the crew were in their late teens and early twenties, although there was at least one child aged only ten. Their average height was about 171cm and they had similar facial characteristics to 21st-century males. Their dentition was fairly good, with modern patterns of tooth decay, but with better occlusion and less crowding. It was noted that many adult teeth had enamel hypoplasia suggestive of previous malnutrition, consistent with a severe famine during the English winter of 1527-1528. Other evidence of dietary deficiencies suggested childhood rickets and adult osteomalacia and possibly healed scurvy.
Evidence of trauma included several healed lower limb, nasal, rib and skull fractures. There were also several avulsion injuries, particularly of the tibial tubercle, and several fracture-dislocations of the hip. One case of Perth’s disease was found. Osteoarthritis was present in several spines and one set of elbows and appeared to be age-related. However, evidence of infectious disease was limited to possible TB, with no evidence of leprosy or syphilis.
A separate finding was a 12.5% incidence of osacromiale (non-union of the acromial epiphysis), mostly on the left side, compared with a modern incidence of only 3%. One possible reason for the higher incidence in the Mary Rose crew relates to the use of longbows from childhood by dedicated archers. Henry VIII enforced a 14th-century law that all fit males from seven to 60 had to practice with the longbow. Tests of longbows recovered from the Mary Rose indicate that they required a draw force of up to 75kg, compared to modern competition-bows which only require about 20kg. As longbows are drawn differently to competition-bows (for a right-handed man, by extending the left arm and shoulder instead of flexing the right), it may have been this technique, as well as the forces involved, that is responsible for the high incidence of osacromiale.
The overall conclusion was of a relatively fit population, but with a high incidence of childhood dietary deficiency, and several old lower limb injuries that could be consistent with unstable seagoing conditions.
TUDOR NAVAL AND MEDICAL DEVELOPMENTS
After several false starts, the Royal Navy was established by Henry VII, who built five ships and the first English dry dock (at Portsmouth). In so doing, his fleet developed from a mere armed transport service into a fighting force in its own right. Even so, Henry VII continued to hire his ships out in peace and to hire or impress merchantmen for war, a pattern that was followed into the next century. In the event, his ships were only used for anti-piracy patrols and they only fought one minor action, off Sluys in Holland, in 1492.
Henry VII also contracted with his noblemen to provide him with soldiers but left it to them to decide whether to take surgeons as well. Those who did either brought one with their retinue or had one indentured for the job by the London Barber-Surgeons Company. Although English surgeons first went to sea in this way, they were only taken to treat wounded soldiers, who ostensibly still did all the fighting. This meant no formal medical arrangements were made for Henry VII’s sailors.
Henry VIII ascended the throne in 1509 at a time of escalating tension with Scotland and France. Recognising the need for a strong navy, he initiated a maritime revolution when he commissioned the Mary Rose in 1511. Rather than carrying many small antipersonnel guns in the fore and aft castles and upper decks, she had 15 large ‘anti-ship’ guns below deck, firing through gun ports in the hull.6 These gun ports also led to carvel (edge-to-edge) replacing clinker (overlapping) hull construction. Three years later the Mary Rose was joined by the 1000 ton Henry Grace a Dieu, with a crew of 500 sailors and 500 soldiers.2 The Mary Rose was rebuilt at least twice before her loss in 1545.
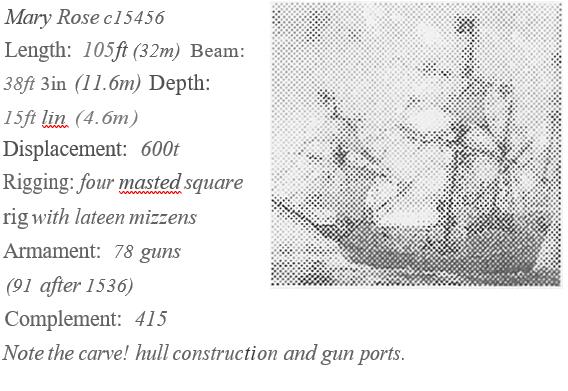
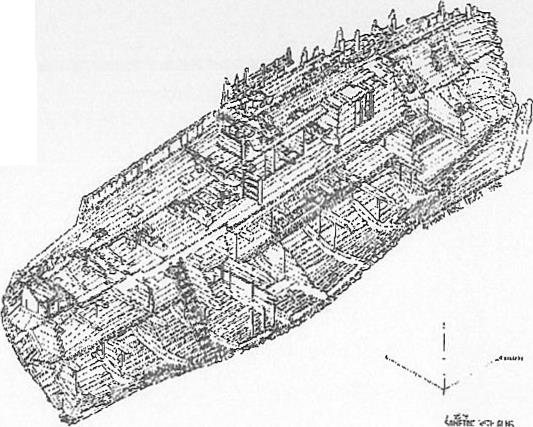
The surviving hull structure consists of a half section from bow to stern, with the whole port side missing. The lowermost level is the hold, containing ballast, stores and a brick galley. Two skeletons were found in the hold with remnants of straw nearby, suggesting they were sick or wounded. The level above the hold is the orlop, which contained more stores and equipment, as well as longbows and other hand weapons. Above the orlop is the main gun deck, with six large guns per side and four surviving cabins, including one for the surgeon. The upper deck had more guns and hand weapons, with archers shooting from behind protective blinds. It was also covered in anti-boarding netting, which meant that only those in the masthead fighting tops had a chance to escape when she sank.
Large below-deck guns eventually eliminated the need for soldiers at sea, by allowing ships to stand off and batter each other, instead of having to grapple and board to fight hand-to-hand. Fewer soldiers allowed more seamen to be carried, thereby enhancing ship handling efficiency. As a height advantage was no longer required for boarding, the fore and aft castles were reduced in height, while the ships’ length-to beam ratio was increased to improve seaworthiness. Henry VIII’s ‘high-charged’ carracks became Elizabeth I’s ‘race-built’ galleons, which in tum evolved into the line-of-battle sailing ships that dominated maritime power until the 1850s.8 These developments led to distinctly different warships and merchant men, and allowed the former to fight offensively rather than wait to be attacked7. Further improvements to the warfighting capability of English ships came when the 22 different types of gun in naval service under Henry VIII was reduced to five-under Elizabeth I.
Other technical improvements led to incidental health benefits. For example, better bilge pumps allowed for drier and hence healthier ships.2 In 1578, Sir William Wymer recommended replacing gravel ballast with large stone ballast to allow ship’s holds to be kept clean2 but this took time to be accepted, with the French continuing to bury their dead in the ballast until the 18th century.9 The French also suggested hammocks as early as the 1550s as they were easier to clean than lice-ridden straw beds, but their introduction aboard English ships after 1597 was driven by Sir Walter Raleigh’s dislike of cabins, as dens of sickness and fire and splinter hazards in action. In 1590, Sir John Hawkins followed Wynter’s suggestion to move the ‘cook room’ or galley from the hold (as in the Mary Rose) to the upper deck, thereby reducing contamination, improving ventilation, and allowing better stowage.
Sanitary arrangements, however, remained basic, with a ‘necessary seat’ in an exposed and sometimes dangerous location forward, while tubs of water were kept between decks for use as combined urinals and fire buckets. Meanwhile, the Laws of Oleron still did not permit sailors to undress at sea, resulting in hygiene problems.
As his sailors began to fight their ships themselves without soldiers, Henry VIII formalised his father’s ad hoc medical efforts by instituting the first English naval medical service. The Exchequer accounts for his 1513 expedition to France lists 19 ships with no less than 32 surgeons serving under four master surgeons, led by a chief surgeon named John Veyrier. As a major fleet unit, Mary Rose had Robert Sympson as one of the master surgeons and Henry Yonge as his ‘mate’ or assistant. These surgeons received the same non-combatant status that English military surgeons had had since 1491. The same organisation was probably also used for the war with France in 1545 and the Spanish Armada in 1588.
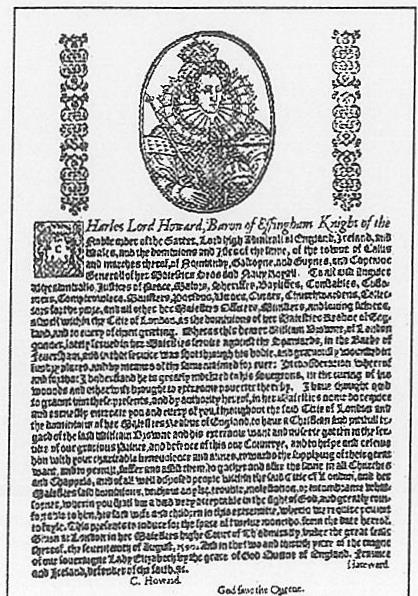
However, although a few disabled mariners received gratuities, the care of temporarily disabled seamen ashore still relied on the Laws of Oleron. A 1513 account had ‘Andrew Fysche, one of the gunners of the Mary Roose to heal him of his hurts, 13s.14d. In the absence of pensions, most permanently disabled seamen relied on begging licences or competed with the other sick and poor for what little charitable accommodation remained after the Dissolution until Lord Howard, Sir Francis Drake and Sir John Hawkins organised the Chatham Chest in 1590. This was an independent mutual benevolent fund, to which every seaman in the royal ships contributed sixpence a month. Despite abuses, the Chatham Chest lasted until 1829.
In 1546, Henry VIII replaced the office of Keeper of the King’s Ships that had existed since 1209 with a Naval Board of five officials, who were responsible for the building, maintenance, victualling and manning of his ships. Despite considerable nepotism and corruption, the Naval Board generally did a responsible job until the Admiralty was completely reorganised in 18325. However, the first shore-based naval medical commission was not established until 1653 and it was not until 1702 that the Royal Navy established a permanent medical department.
TUDOR BARBER-SURGEON TRAINING
Tudor period had four types of a medical practitioner. The most prestigious were physicians with university degrees, albeit in humoral medicine. These were followed by members of the Fellowship of Surgeons, who were also university trained, highly skilled and often qualified in both medicine and surgery. Next were the barber-surgeons, who qualified by apprenticeship to a master surgeon, followed by the apothecaries, who sold medicines from their shops with free advice and were regulated by the Grocer’s Company. These practitioners also competed with traditional non-qualified herbalists, quacks and astrologers.
Henry VIII’s 1511 Medical Act made the London bishops responsible for examining London’s barber surgeons and a similar act was passed for physicians in 1518. In 1540, Henry VIII made the Fellowship of Surgeons responsible for regulating the London Barber-Surgeons Company, and he also established a similar relationship between the physicians and the apothecaries.2 This exacerbated the divide between surgeons and physicians, with disastrous consequences for sea-surgeons because they had to practice both. The 1511 Act also tried to define the medical profession, thereby arousing opposition from the unqualified practitioners. This led to the 1542 ‘Quack’s Charter’, which also made them liable for sea service.
By 1563, apprentice surgeons had to be less than 21 years of age on entry. They had to serve a seven-year apprenticeship, during which their lives were closely regulated down to dress and hairstyle and they were not allowed to marry. Their apprenticeship was practically oriented, although their use as servants led to difficulties from those fathers who felt they were not getting value for their indenture money.
Although Barber-Surgeons were allowed to dissect four executed criminals per year after 1540, most of their anatomical and other training came from books. The leading authors included Thomas Vicary (d 1561), John Read, Thomas Gale (1507-1587) and William Clowes (1544-1604), all of whom wrote in English rather than Latin for the first time. Vicary produced a compilation of previous authors as A Profitable Treatise of the Anatomie of Man’s Bodie in 1548. Read translated passages from Franciscus Arceus and John Arderne into A most Excellent and Compedious Method of curing Woundes in the Head and in other Partes of the Body in 1588 and was noteworthy for attacking quackery. Although he never served at sea, Gale had considerable interest in young military surgeons and wrote An Excellent Treatise of Wounds made with Gunshot and An Enchiridon of Chirurgie in 1563.
However, the father of English naval medicine is William Clowes. He qualified at 19 years of age and served for several years at sea as well as ashore. In 1570 aboard the Queen’s ship Aid, he treated a boatswain who sustained two fractured ribs from a capstan bar, by incising the fracture site to remove a sliver of bone which was abrading the pleura. The wound was redressed on day five and had healed by day ten; a creditable effort aboard a 200 ton Elizabethan warship. On leaving the navy, Clowes worked at St Bartholomew’s in London, but returned to military service in the Netherlands in 1586-7, where he later stressed the importance of improvisation, using fingers as instruments and scabbards as splints. He was appointed to the fleet again in 1588 for the Armada but was soon released.
Like Gale, Clowes also tried to improve the status of military surgeons, vehemently attacking quacks despite their protection by the 1542 Act. In 1588, he wrote A Prooved Practice for all Young Chirugeons, which he updated in 1596 into A profitable and Necessarie Booke of Observations for all Those that are Burned with the Flame of Gun Powder, and also for Curing of Wounds made with Musket and Caliver shot, etc2. For amputations, Clowes had a strong operating table on which an assistant could sit astride the patient, holding both arms down. For below-knee amputations he had another assistant astride to hold down and steady the thigh and a third to hold the distal limb. He used a tourniquet for both haemorrhage control and analgesia. The amputation was performed circumferentially and, as the tourniquet was released, he found and stopped each bleeder. With the addition of four cross sutures to cover the stump, this technique was used at sea for the next three centuries.
Although recognising the need for naval surgeons to also practice medicine, Clowes cautiously stated that he used all honest and lawful measures to practice both medicine and surgery, if no physician was available. He recognised the primary and secondary stages of syphilis as the only time it could be treated by external application of mercury and gave a full account of scurvy, even associating it with the seamen’s diet.
Although the College of Physicians often tried to prevent lectures to the Barber-Surgeons on medical issues, Clowes did so until he handed over to John Banester (1540-1610) in 1600. Banester had served ashore Wilh Clowes in 1563 and 1586 and lost 45 patients (one-third of his crew) during a failed expedition to the East Indies in 1582, of whom only three were surgical cases.
After seven years of training, the apprentice was examined in anatomy, surgery, pathology (such as was known), the significance of certain signs and managing emergencies. He then received a restricted licence allowing him to receive wages while working as an assistant. To receive an unrestricted license, he waited another year and then either underwent further oral examinations or gave a lecture every six months until the Company was satisfied. He then paid £4 and was presented to the London bishops, after which he was licensed to set up his own practice as a Company freeman2. Country surgeons either made do with the local bishop (with resulting problems if he failed to consult the local barber-surgeon’s guild) or underwent a modified examination by the Company before being licensed by the London bishops.
John Banester lecturing at Barber-Surgeons Hall in 158F
However, as sea-surgeon apprentices were typically impressed from the country, they had not contributed previously to the Company and were therefore excused the period of restricted practice. This meant that they only had to pay seven guineas to the Company to be admitted as a freeman. Although apprentices could complete their training as mates to qualified sea-surgeons, a problem lay in the fact that ship’s captains could employ anyone in any job. This meant apprentices frequently bypassed the examination altogether if their mentors died, such that this almost became a normal naval promotion, without reference to the actual responsibilities or qualifications involved.
THE MARY ROSE MEDICINE CHEST
Clowes advised his students on what a military medicine chest should contain, using his own 1563 chest as a model. Given the alchemic approach to therapeutics at the time, apart from the usual purgatives, the drugs were often rare and costly but often did little more than sweeten the air or hide the taste of rotting food.
Clowes’ medical chest was probably similar to one retrieved from the Mary Rose in 1980. It was found in one of the cabins on the starboard side of the main gun deck. Almost empty of silt and undisturbed, it measured 1330 x 485 x 460mm 12 and was made of walnut with dovetailed joints on the corners, with a solid bar at each end pierced for rope handles. There were no internal partitions, except for a shallow lidded shelf on one side.
The 64 objects within included nine wooden containers with lids, eight containing ointments and one containing peppercorns. One ointment had a resinous substance which may have been frankincense, complete with scoop marks from the surgeon’s fingers. There were also five carefully corked ceramic jars from Siegburg in the Rhineland, with contents that may have included linseed oil, resins, henbane, quince or belladonna. Also found were several sausage-like rolls of unguents, made with a 2:1 ratio of fuller’s earth and frankincense, which may have been used as plasters.
Drawing of Mary Rose remains, showing the barber-surgeons cabin
The chest had one brass and one pewter syringe, their needles having small rounded nipples at the tips. Ambrose Pare (1510-90) referred to the use of the small syringe for urethral syringes for bladder stones and strictures from gonorrhoea and to the use of the glister or large syringe to treat the ‘flux’ (diarrhoea) and constipation.
Although the steel had corroded away, the chest also had had a collection of surgical instruments, with eight handles similar to 17th-century cauteries and a larger handle that may have been part of an amputation saw or large knife. There was a wooden mallet, eight cut-throat razors (indicating the surgeon was also the ship’s barber) and a whetstone. Other items included a large brass shaving bowl, a small pewter bleeding bowl with the initials ‘WE’ on one handle, a small brazier for warming a chafing dish, and a heavy mortar for grinding drugs.
 Bleeding bowl from the Maty Rosebarber-swzeonchestlj
Bleeding bowl from the Maty Rosebarber-swzeonchestlj
Urine bottle from the Mary Rose barber-surgeons Chest


Right: Barber-surgeons coif from Mary Rose, worn by a reluctant volunteer before restoration”
As one of Henry’s major fleet units, it seems likely that Mary Rose had a master surgeon and an assistant on board. It was odd that, despite the preparations for action, the chest was intact (but ready for use), yet the surgeon was not in his cabin when she sank. A further mystery was revealed when a set of apothecary’s scales was found on the after portion of the upper deck.’ A clue may be two letters from Henry’s commanders referring to an outbreak of the ‘bloody flux’, which prostrated entire ship’s crews. It is possible that, when the Mary Rose sank, her surgeon was treating patients in the hold, while his assistant was weighing out ingredients for medicines on the only part of the ship with enough light to see what he was doing. It is, therefore, possible that the Mary Rose sank, not through overloading or incompetent handling, but by a crew that was too ill to act in an emergency.


Although not directly related to medical issues at sea, the 81 combs recovered from the wreck may be indicative of shipboard hygiene standards. All except two were double-sided and made of boxwood1. Of note are the fine teeth of many combs, suggesting that they were used for delousing, rather than mere tonsorial elegance. In the likely absence of any other means of controlling fleas and the restrictions on removing clothing at sea, the number of combs found suggests that the standard of hygiene was less than ideal. The fact that the barber-surgeon had two combs (one found within the chest) suggests he was not immune from acquiring his own dermatological livestock.
SEA SURGEON’S CONDITIONS OF SERVICE
The first English sea-surgeons had significant problems with their status. Apart from the gentry, who acted as commanders in English ships until Francis Drake hanged one for mutiny, the most important seagoing officers were the gunner, the boatswain and the carpenter. Although a few master-surgeons served at sea with the gentry, most were ranked with the cook, smith, tailor, shoemaker, trumpeter and musician, which meant they lacked a meaningful place in the seagoing command hierarchy.
The fact that surgeons started their careers as apprentices also created ambiguity, especially while the Barber-Surgeons Company had more barbers than surgeons. Although barbers and surgeons were separated as far back as 1376, barbers were still permitted to per form ‘procedures’ such as trimming corns, while the Mary Rose chest confirmed that naval commanders used their surgeons as barbers. This meant apprentice sea surgeons had to acquire barber’s tools and learn how to use them before joining their first ship.
The impressment (compulsory service) of surgeons also contributed to their low status, especially as those liable ranged from fully qualified practitioners to mid wives, oculists, dentists and bonesetters, who often used ‘real’ surgeons to perform procedures that were outside their expertise. Often their deficiencies were not revealed until it was too late and it was the ensuing clinical disasters that gave all sea-surgeons a poor reputation. Martin Frobisher’s death through mismanagement, despite a slight wound in the thigh by a bullet at Brest in 1594, probably did little for their credibility.
Social barriers within the profession militated against sea-surgeons, as they were held in low esteem not only by the physicians but also by their land-based brethren. The lack of legal authority to give internal medicines meant that they were often put on trial by physicians on returning home. Yet at least some Tudor sea-surgeons must have given some confidence to their ship’s company, because sailors often refused to go to sea without one and when carried he was usually placed out of harm’s way in the hold during action.
As in the past, noblemen continued to make their own arrangements with either the Fellowship of Surgeons or the London Barber-Surgeons Company. William Gooderus, John Banester and William Clowes were all engaged on these terms, with Gooderus becoming serjeant surgeon of the Company, while Clowes and Banester passed on their military medical experience to young apprentices.2 However, because neither the physician’s nor the surgeon’s guilds had any specific responsibility for seamen’s health care, it was only via these indirect means that any naval health knowledge was passed on at all the lack of a shared pool of expertise in naval medicine, therefore, meant that the same mistakes were repeated again and again.
Furthermore, as neither the first Fleet Instructions dated 1530 or those of 1545 had any medical instructions, the royal ships at first failed to benefit from the medical lessons learned by the merchant adventurers during their overseas raids. It not until 1596 that the Instructions Issued to the Royal Navy included ‘you shall give orders that your ship may be kept clean daily and sometimes washed; what with God’s favour, shall preserve from sickness and avoid many inconveniences’2. Part of the problem lay in confusing ‘comfort’ for ‘hygiene’, with a ‘school of toughness’ deriding the health benefits of liberal diets, dry clothes, warmth, and bedsheets. Yet it was these informal contacts between the royal ships and privateers that led to the unwritten rules that became the foundations of naval hygiene.
Access to exotic overseas flora could have allowed sea-surgeons to import therapeutic drugs, including aloe, senna and ipecacuanha. However, as most surgeons lacked the authority and/or necessary training in internal medicine, it was often their captains who brought back reports of maladies and treatments2. One example was John Lock, who wrote the first description of trachoma, during a visit to Cyprus in 1553. In 1572, a merchant named Henry Hawks first linked illness to ‘musquitos’, but its loss meant that mosquito-borne disease continued to be ascribed to ‘night air’ for another 300 years.
A divided medical profession and their low status afloat meant living conditions aboard were largely controlled by ship’s captains. As health care ashore extended beyond the medical professionals, the captains’ involvement in treating ‘sea-diseases’ fell within this pattern. With the physicians trapped by their humoral theories of disease, the captains’ efforts often met with some success. This stemmed from their authority and practical experience, although they were just as prone as physicians to theorising as to why things worked, without any attempt at scientific validation2. From there, it was only a small step to captains taking over all non-surgical health issues, leaving the surgeons with only the actual hands-on application of their skills. London surgeon Thomas Roes wrote in 1519 that this included controlling haemorrhage, trephining, couching for cataract, removing sequestra, suturing wounds, lancing abscesses, reducing fractures and dislocations, dental extractions and bloodletting.
It is therefore not surprising that the first book on tropical diseases was actually written by a non-medical adventurer. In 1598, George Wateson’s The Cures of the Diseased in Remote Regions preventing Mortality Incident in Forraine Attempts by the English Nation presented a confused mix of typhus, yellow fever, dysentery, erysipelas and prickly heat. Wateson recorded some useful elements, although he avoided mentioning any conditions of which physicians at home were already aware while dressing up simple conditions with expansive Spanish names (such as ‘cameras de flux’ for the bloody flux) to make them seem more exotic.
The second part of this article will discuss the medical aspects of Tudor naval operations.






