Introductory Note on Sources
In the absence of access to original material (not to mention a lack of knowledge of Latin and Middle English), this article is based on information from the first volume (of four) of a history of British naval medicine, written by Dr John Joyce Keevil MD, BCh, MRCS, LRCP, DTM&H.1
Born in 1900, Keevil was educated at Cambridge and St Thomas’s Hospital. He joined the Royal Navy on 16 July 1927 after qualifying two years previously but did not take his university degree until 1931 and his MD until 1936. He was promoted to Surgeon Commander on 9 July 1937 and at the outbreak of WWII was posted to the New Zealand Squadron.1 Most of his wartime service was in aircraft carriers, including Illustrious, Indefatigable and in the Far East in Implacable. It was in Illustrious that he was awarded the DSO, after she was dive-bombed on 10 January 1941, leaving 125 men dead and over 150 wounded.2 He later worked in the Royal Naval Medical Department collecting material for the British official medical history of WWII, on comparable terms to the late A.S. Walker’s efforts for the Australian WWII official historian Gavin Long.
Keevil resigned in 1946 to pursue a literary career, writing two works of fiction and the first two volumes of his naval medical history before his death in 1958. The last two volumes were completed by Surgeon Captain J.L.S. Coulter, DSC, FRCS, RN and Mr C.C. Lloyd, MA, FRHistS.3 At that time, Jack Coulter was Medical Officer In Charge of the Royal Naval Medical School and had recently completed Keevil’s work on the WWll medical history. Christopher Lloyd was Assistant Professor of History and English at the Royal Naval College at Greenwich, and later wrote on the health of British seamen for the Naval Records Society.4
The aim of this article is to summarise Keevil’s history of naval medicine, during the medieval period from 1200 to 1500, in order to make comparisons with contemporary ADF practise and to identity common issues.
The Origins of English Medicine
European medicine during the Middle Ages was based on the teachings of Hippocrates and Galen, which, by 1200AD, had been established for over 1000 years.
Hippocrates (c460-c377BC), a native of the Greek island of Cos, is thought to have produced about 70 references on different medical subjects. Besides his well-known oath, Hippocrates was the first medical authority to repudiate the concept of illness as a divine punishment. He also created the concept of determining the prognosis of specific diseases bedside observation.5
Hippocrates
Galen (c129-c200AD) was born at Pergamum, near Smyrna in what is now modem Turkey. During a long career he worked in Greece, Egypt and Rome, writing over 400 medical works that dominated European medicine for the next 1500 years. He made significant surgical advances through his treatment of gladiators and athletes, although a ban on human dissection led to errors, in particular, a belief in ‘laudable pus’ (thick: yellow odourless pus, which was considered to be evidence of a healthy granulating wound).
Galen also developed Hippocrates’ theory of physiology, that the body had four ‘humours’ – phlegm, blood, bile or black bile – and asserted that illness reflected changes in their qualities.
Although this ‘humoral’ medicine never quite displaced common sense, folk remedies or reliance on the supernatural (any more or less perhaps than modem medicine has now), it was not completely discarded until well into the 19th century. In fact, it was not until 1543 that Andreas Vesalius started to correct Galen’s anatomical shortcomings, while doubts regarding his physiological theories began only after William Harvey discovered the circulation of the blood in 1628.
Galen (16th-century engravings)
Before 1150 the English generally relied on ancient Anglo-Saxon folk traditions of leeches, charms and medicinal herbs. 1 Modem English medicine began with Roger Bacon (1214-1294), a friar whose ideas on scientific experimentation formed the basis of later surgical developments. Subsequent advances in English medical knowledge also came from the efforts of monastic scribes. These were initially based on Italian developments, particularly the medical school at Salerno, which was established in about 900 AD and had issued the first medical degrees in 1140.
The best-known medieval English cleric surgeon was John of Ardeme (1307-c1377), whose Liber Receptarum mentions the use of wound dressings made of egg white and flour. It seems likely this was the first wound dressing to be used at sea. Ardeme also went against the Galenic belief in ‘laudable pus’, by cleaning wounds with wine rather than letting them fester. Cleric-physician John Mirfield (c1320-cl393) gave the average time for the
healing of various fractures in his Breviarum Bartholomei but retained his clerical bias by his use of prayer, as well as olive oil, to treat rheumatism.
European medieval medicine was therefore generally characterised by misinformation and a lack of progress. Medical practitioners were limited, not only by their poor understanding of physiology and anatomy but also by Galen’s reputation for infallibility. A further constraint was the belief in temporal suffering as part of the path to eternal salvation.
Early English Medieval Maritime Power
In contrast to the stagnation in medical knowledge, the Middle Ages was a time of steady maritime development. Before 1200, northern European ships were based on the Viking longships; small, single-masted, clinker-built ships with a square sail and oars. Their trading ships however tended to be rounder and shorter than the longships and were known as ‘knorrs’.
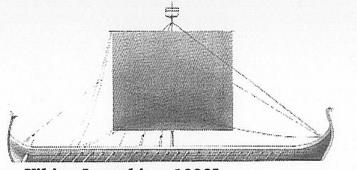
Viking Longship, c10007
Length: 120ft (26.6m)
Beam: 20ft (6.1m)
Depth: 3ft 6in (1.1m)
Complement: 50
The formation of the North German Hanseatic League in 1159 for trade led to the development of vessels known as ‘cogs’ after 1200. These were similar to the Viking knorrs, but tended to be larger and were the first ships to mount stem¬ mounted rudders instead of steering oars.
Increasing trade led to larger cogs and, as the Hanseatic League came into conflict with other northern powers, soldiers were soon placed aboard to protect them. However, it was not until about 1285 that cogs were given temporary towers or ‘castles’ fore and aft, to give the soldiers a height advantage in action. These temporary castles were permanently incorporated into the cog’s design in about 1350, resulting in the first permanent ship’s cabins for the crew and passengers.
Although all English ports hired their ships out for trade-in peacetime and had them ‘impressed’ (requisitioned) by the king in wartime, the key to English medieval maritime power were the Cinque Ports. Since the time of Edward the Confessor (c1003-1066) the ports of Dover, Hastings, Hythe, Romney and Sandwich (to which Rye and Winchelsea were added in the 1190s) were required to provide the king with 57 ships manned by 1140 men for 15 days per year, in exchange for certain tax privileges.1 In the early 13thcentury, these ships were essentially large open boats hardly exceeding 80 tons, which were only capable of short voyages during the summer months. In the period before permanent cabins, the only shelters were made of canvas and the wet conditions were exacerbated by the lack of efficient pumps to keep the bilges dry. The food was highly perishable, poor quality and boiled in a cauldron over a wood fire on deck.!
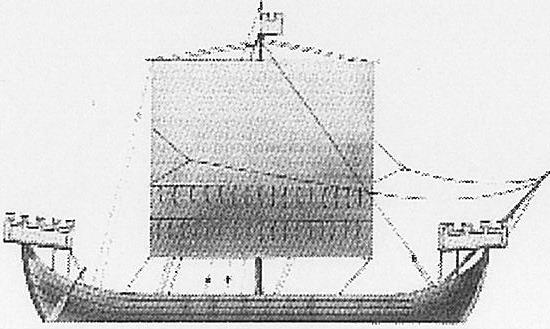
English Co c13007
Length: 42ft (12.8m)
Beam: 12ft (3.7m)
Depth: 7ft (2.1m)
Displacement: 180t
Armament: machines to project stones and arrows.
Complement: 6 seamen plus soldiers
It was in 1227, during a voyage to Palestine in one of these ships, that Gilbertus de Aquila (Anglicus) acquired the nautical knowledge for the first known written advice on naval medicine. His Compendium Medicinae advised seafarers to keep clean, protect their heads from the sun, eat a moderate diet with plenty of fruit (anticipating the prevention of scurvy) and to exercise if possible. Gilbertus also anticipated a 19th century Admiralty regulation for airing clothing and bedding to rid them of fleas and lice. He even stated that drinking water could be obtained from seawater by distillation.1 Had his advice been accepted earlier its effects on naval history, let alone naval medicine, would have been profound.
As ships were only used in war to transport armies over short distances, there were few naval engagements. Furthermore, sailors were only employed to move the ships to where the soldiers wanted to fight their battles. The latter used bows and lances during the approach to grapple and board. This was followed by hand-to-hand fighting with swords and axes, while the opposition threw rocks and lumps of metal from the masthead tops. Neither side gave a quarter and the losers went over the side whether they were wounded or not.
13th century Naval Action (Taken from a manuscript held by the Fitzwilliam Museum, Cambridge)
As they had no direct fighting role, the English did not expect sailors to be wounded as part of their duties. Furthermore, they believed surgeons were only of use for treating battle casualties who, by definition, were soldiers and not sailors. Given the perceived lack of a peacetime role, the lack of battles at sea, the short distances from shore when one was fought, the lack of treatment facilities afloat and the small numbers of surviving wounded, the need for English sea¬ surgeons did not exist until the early 1500s. Yet as early as 1317, a Venetian mission to England had included a ‘medical-surgeon’ appointed to the flagship, with Genoese ships following from 1337.
The Laws of Oleron and the Charitable Institutions
It was in this context that a fleet of 36 ships, owned by Eleanor. Duchess of Aquitaine left France in May 1153 to carry her second husband, Henry II, to the English throne. This fleet also brought to England its first maritime laws, including those providing for the medical care of English seamen.
Eleanor had accompanied her first husband on the Second Crusade and returned to Aquitaine with the Maritime Assizes of the Kingdom of Jerusalem. The Assizes had originated as the ancient Lex Rhodia, which had governed Mediterranean commerce for centuries prior to the Christian era. They were adopted by the seaman’s guild on the island of Oleron off La Rochelle, where Eleanor set up a maritime court to administer them as the Customs of Oleron. They covered numerous matters, including the responsibilities of masters with respect to hiring his crew, their discipline and welfare and their profit shares
The Lex Rhodia had two medical provisions, which were omitted from the Assizes. The first was:
“if sailors set to fighting, let it be with words and let no man strike another. If a man A strikes another man B and opens it or injuries him in another way, let A pay B his doctor’s fees and expenses, and his wages for the whole time he is away from work taking care of himself’
The second prescribed compensation and punishment in connection with causing a hernia or the loss of an eye.
However, the medical provisions of the Customs of Oleron differed significantly from the Lex Rhodia. It stated that if a seaman was injured through drunkenness or fighting, the master was not bound to provide for him and could turn him out of the ship. However, Article 7 also states:
“if it chaunce that any maryner be taken with sekenesse in the ship doyng service thereto be belogyng, the maister ought to set hym out of the shyp, and seke lodgyng for hym, And ought for to
fynde hym lyght, as talowe or candell, and to gyve hym a lad of the shyp for to take hede of hym or hyre a woman to kepe hym; and ought to purvey hym of suche meat as is used in the shyp, that is to wyte, as moche as he toke whan he was in helth, and no more, but yf the mayster wyll And yf he wyl have deyntyer meates, the mayster is not bounde to gete hym any, but to be at his castes. And yf the shyppe be redy to departe it ought not to tarry for hym, and yf he recover, to have his hyre in payinge and rebatynge that the mayster layde out for hym And if he dye his wyfe or next of kynne or frende oug hte to have it for hym The judgement is suche”.
This meant that if the injury occurred in the service of the ship, the owner was to pay for his treatment. However, this was only up to the cost of keeping the patient when he was healthy, with the patient paying for any extras. If the ship was due to sail, the patient (or next of kin if he died) was to be paid up to the time of departure. With modifications, these principles have generally continued to apply to the present day.
It was not until 1194 that Eleanor’s son, Richard I (‘the Lion Heart’) formally adopted the Customs of Oleron in England as the Laws of Oleron (later referred to as ‘Olrums’).1However, although ‘Olrums’ gave ship’s masters the obligation to pay for accommodating their sick. A key omission for the next 450 years was the lack of accommodation for them in the first place. A further problem was a prohibition on undressing at sea, with severe punishments for breaking this regulation.
Article 7 of the Laws of Oleron, from The Black Book of the Admiralty.
Once ashore, the care of wounded seamen was complicated by the lack of distinction between royal and merchant ships, because both were used for peaceful as well as warlike purposes. Although this meant the Laws of Oleron could not be restricted to merchant sailors, mariners who were wounded in the King’s service were often treated as soldiers and were frequently abandoned by their lord on their return home.1 Even seamen from the Cinque Ports could only expect temporary accommodation if they were sick or wounded unless they could enter a charitable institution.The first modem hospital in Western Europe was the Hotel Dieu, which was established in about 542AD at Lyon in France, with the English not following suit until St Batholomew’s Hospital was established in London in 1123. In 1198 Pope Innocent III (c1160-1216) encouraged the religious orders to build more ‘houses of pity’. He also encouraged the nobility to provide charity for their retainers and servants, as part of their path to salvation.
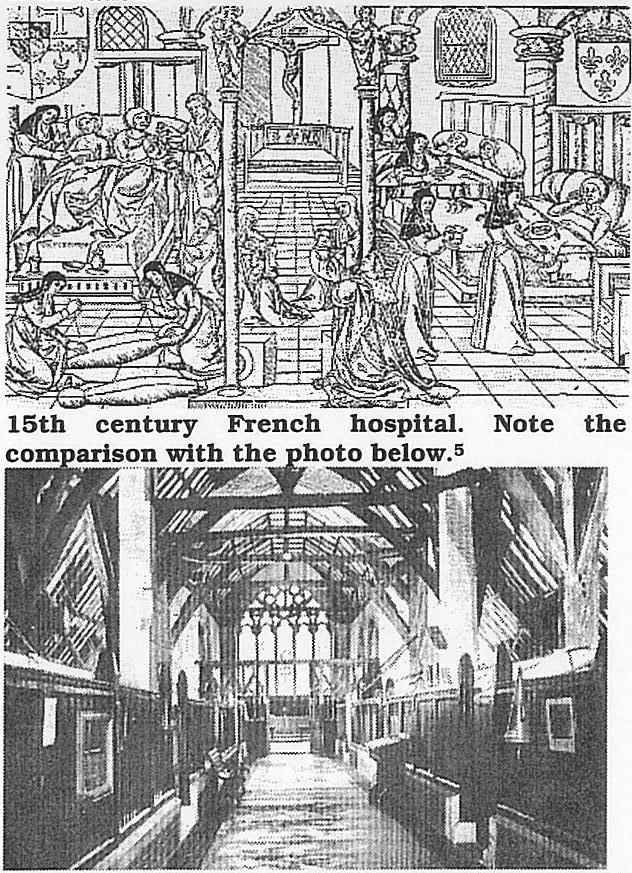
Hospital of St Mary, Chichester UK, a small surviving medieval ‘House of Pity’, c1950s. I
The permanently disabled typically gained admission to these places by surrendering all their possessions in exchange for a small allowance, which was forfeited if they failed to do what work they were able to do. This led to many tiny communities with each individual doing what he could, aided by cooks, brewers, smiths, carters and boatmen. Their sources of income included alms from the king, churches, the ownership of manors, tolls and tithes, and sponsored appeals aided by the advent of a wealthy merchant class. Richard’s successor John also provided for disabled soldiers and sailors by allowing hospitals to hold fairs in exchange for admission rights when required.
This pattern of care for naval casualties began after a battle off Dover in 1217, when the few surviving wounded were accommodated at several places ashore, including the Maison Dieu Hospital, an almshouse located on the Dover quay. Later, as the number of permanently disabled sailors increased, they began to establish their own ‘houses of pity’ via their craft guilds, with the first European hospital for seamen being founded in Venice in 1318, by a sea-surgeon named Gaulterius. However, the first English seamen’s guild was not founded until 1369, and it was only in 1457 that a seamen’s almshouse or ‘masyndew’ (named after the Dover hospital), was built at Kingston-on-Hull. The Cinque Ports thereafter developed their own ‘masyndews’ and other English ports along the south coast soon followed. These ‘masyndews’ often had less than ten beds and the standard of care varied considerably. Other seamen’s guilds either continued to rely on private citizens or contributed to other charities in exchange for access for their members.
Barbers, Surgeons, Physicians and Apothecaries
The care of sick sailors ashore initially lay with the master of the charity or ‘masyndew’ who, if he were a priest, may have dressed their wounds as well as hear their confessions. However, after 1139, the clergy were progressively discouraged from teaching or practising medicine outside their monasteries. Despite encouraging ‘houses of pity’, in 1215 Innocent III prohibited priests from performing any surgery involving cautery or incision, and this ruling was repeated by Pope Gregory IX in several decretals in 1230-34. In 1216, Henry III prohibited the English clergy from practising any medicine at all.
As a result, the clergy began to train the barbers who were originally employed to shave their tonsures. This led to the founding of provincial barber-surgeon’s guilds, including the London Barber-Surgeons Company in 1308. A 1370 Act of Parliament required all guilds to have a seven-year apprenticeship and in 1376 the London Barber-Surgeons separated into barbers and surgeons within the same guild.1 The surgeons soon dropped the barber prefix, although even in the 17th century the navy still expected them to cut hair. The London Barber¬ Surgeons were incorporated by a 1462 Royal Charter, which required them to supply surgeons not only for London but the army (and later the navy) as well. Many barber-surgeons began their careers at the charitable institutions and it was these young itinerants who first treated wounded seamen ashore, that were eventually hired or pressed to treat them at sea.
After Parliament required every man to belong to a guild, a Fellowship of Surgeons was founded in London in 1363 to provide a small number of university-trained surgeons for the nobility and to supervise the barber-surgeons guilds. The Fellowship of Surgeons established regulations for the examination of all London barber-surgeons in 1435, but an agreement with the London Barber¬ Surgeons was only reached in 1493 and formal linkage did not occur until 1540.
None of these developments affected the medical care of sailors in the short term, except that their ‘masyndews’ placed them somewhat closer to the sources of medical knowledge than their landsman counterparts. The latter relied on the local herbalist or drug-seller, who eventually became known as apothecaries, whose practical experience and skill mostly displaced the folk remedies of the village matrons. Instead of Galen’s humoral model, the apothecaries’ theories of treatment were generally based on opposites (hot conditions being cooled and vice versa), while their diagnostic capabilities were given a scientific veneer by urine inspections and checking the pulse.
The apothecaries and physicians soon developed a relationship on parallel lines to the barber-surgeons and surgeons, with a small select university-trained group to care for the nobility and to supervise those who treated the masses. This was compatible with the prevailing view of suffering as part of God ‘s will and, as seamen numbers were still relatively small and naval engagements few (the latter requiring surgeons to only treat wounded soldiers in any case) this had little effect on their care.
However, in 1421 an attempt was made to combine the physicians and surgeons into one college, but this failed three years later. This split in the English medical profession lasted 400 years and had two crucial effects on naval medicine. Firstly, physicians typically belonged to the higher strata of society and were therefore above mere service at sea. Secondly, for centuries, surgeons were only wanted to treat the wounded and even if they had medical cases (typically outnumbering the surgical cases). They lacked the legal authority and the expertise to treat them. Despite the limitations of humoral medicine, it seems likely that much of the mortality from epidemics at sea could have been averted if sea-surgeons had training in internal medicine.
Later Medieval Ships and the First Sea¬ Surgeons
Richard’s crusader nobles found that the Middle Eastern powers had highly organised medical organisations, in the traditions of the old Roman Empire. These consisted of ambulance corps with surgeons and assistants attached to each unit.1 Although the nobles brought their own physicians from England, the Middle Eastern physicians proved more efficient and many were used on their Mediterranean voyages. However, as they were only there to treat the nobility as part of their retinues, the soldiers and sailors generally did without.
Although the Crusades had little influence on English medicine, they led Richard ‘s successor, John, to establish the first regular English navy in 1209. When he appointed a Keeper of the King’s Ships and built a naval base at Portsmouth. However, John ‘s successor, Henry III, relied on the Cinque Ports, initiating a series of swings in naval capabilities which continued throughout the world to the present day. Although Henry took two surgeons to Gascony in 1253 (Master Thomas de Weseham and Thomas the Barber), they went only as part of his personal retinue.
In the early 14th century, Edward II had ten or 11 ships of up to 250 tons, each with crews of up to 120 men, for summertime anti-piracy patrols, although in wartime he still pressed merchant ships into his service. By 1350, English ships had permanent ‘castles’ forward and aft, with an enclosed space forward for the crew and another aft for the officers. However, there were still no bilge pumps and they were unable to operate in the northern winter months.
English Cog c13707
Length: 75ft (22.9m)
Beam: 22ft (6.7m)
Depth: 6ft 6in (2.0m)
Displacement: 120t
Armament: machines to project stones and arrows
Complement: 6-12 seamen plus soldiers
The Hundred Years War from 1338 was noteworthy for the naval battles at Sluys in 1340 and at Les Espagnols-Sur-Mer in 1350, where high casualties from the latter were landed at Winchelsea in accordance with the Laws of Oloron. In addition, Lord Arundel’s expedition to Siuys in 1387 failed because of fever (possibly malaria). Although surgeons accompanied the nobility on these campaigns. No specific arrangements were made for treating soldiers or sailors.
It was not until 1415 that Henry V made any arrangements for soldiers, when he indentured his personal surgeon and his physician to serve in France for 12 months during the Agincourt campaign. Although both were required to provide archers for the campaign, the surgeon also had to find 12 junior colleagues via the London Barber-Surgeons. They were paid the same rate as archers and their listing with ‘soldiers. shoemakers, tailors and washerwomen’ indicated Henry’s sense of priorities. It seems likely these 14 medical practitioners made little difference to an army of 30,000 men. Furthermore, no specific medical arrangements were made for the sailors who got them across the Channel and back again.
By 1400, some of the larger cogs had developed a second mast and were known as ‘carracks’. The first English ship to carry guns at sea was the Christopher of the Tower!, which carried three iron guns and a handgun. These were mounted on the raised ‘castles’ at either end of the ship and were intended as anti-personnel rather than anti-ship weapons.
Christopher of the Tower, c14067
Displacement: 300t
Rigging: two masts; square sail on the foremast and small lateen mizzen.
Armament: small deck guns
It was not until after 1410 that Henry IV began mounting large numbers of guns aboard his ships, thereby initiating a decline in the need for soldiers for fighting at sea. Although the guns were not yet carried below decks, his son, Henry V, built larger and stronger ships with multi¬ storied castles and more tumblehome to accommodate them. His largest ship was the Grace Dieu, the world’s first three-masted carrack, which was built in 1416. Although Henry’s ships were still clinker-built, their increased size led to bilge pumps and below deck cabins and ‘cookrooms’ or galleys. However, after Henry’s death in 1422, his ships were sold and for the next century, England again relied on merchant ships for naval defence. By 1450, three¬ masted carracks were commonplace, were capable of long voyages in most weathers and traded as far afield as Lisbon, Morocco and Iceland.
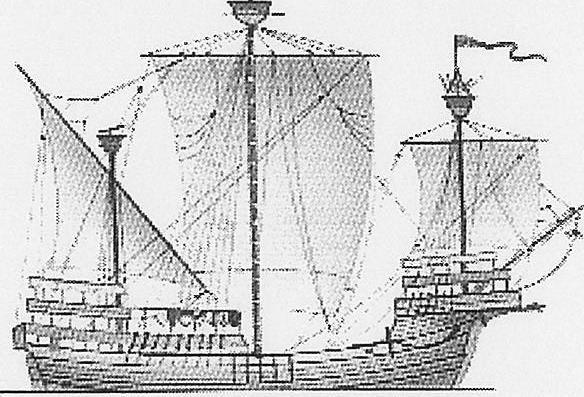
Carrack, c14707
Length: 112ft (34.1m)
Beam: 33ft (10.0m)
Depth: 17ft (5.2m)
Displacement: 180t
Armament: small castle-mounted deck guns
Complement: 20 seaman plus soldiers
By 1500, the Cinque Ports were declining in naval importance, as they were too small for carracks and King Henry VII had begun building his own ships. Although increased size and associated technical advances had established the need for specialist craftsmen to build, maintain and sail these ships, the number even of army surgeons was very small, hence there was still no perceived need for sea-surgeons. This meant that the first sea-surgeons joined a relatively long¬ established nautical hierarchy, which often disregarded their presence and undermined their authority and value. As late arrivals to this environment, sea-surgeons were awkwardly and uneasily included. c
Conclusion
The primitive standard of care ashore during the Middle Ages reflected the lack of medical progress over the previous thousand years, but also came from contemporary ideas of Christian suffering as a part of life. The absence of personalised medical care for anyone other than the nobility and the view that surgeons (when available) were only useful for treating wounded soldiers.
No provision was made for sick and injured English seamen until Eleanor recognised the need in both peace and war. Although she began the legislative provisions for sailors, the provision of health care for anyone ashore, let alone afloat, only began in England after the Church began to withdraw from its medieval role as the repository of medical knowledge.
None of this mattered much when voyages were short, naval engagements few and casualties rare. As a result, it was not until the early 1500s that English seamen began to receive any professional medical care at sea. Furthermore, it would be another 150 years before their medical care ashore would progress beyond the limitations of the Laws of Oleron.
Meanwhile, attitudinal limitations and the split in the English medical profession led to a series of medical disasters over the next three centuries from 1500, in which more campaigns and expeditions failed through illness than through battle losses. Yet, as early as 1227, Gilbertus identified hygiene and other preventive health measures which, had they been adopted, would have had made their success more likely.
Comparison with the provision of ADF medical support in the 21st century suggests at least three common issues all reflecting the requirement to conserve scarce personnel resources.
Although medieval sailors probably expected little and received less in terms of their standard of care, the Laws of Oleron meant they were probably better off than non-sailors. Comparing the health care standard required to ensure the deployment fitness of 21st century Australian sailors with the civilian standard suggests that, in this respect (apart from the extravagant expectations of at least some members) little has changed.
Secondly, it is suggested that the provision of non-operational health support was as much an issue in medieval England, as it remains in 21st century Australia. Medieval medical force preparation though the Laws of Oleron was focused on paying for sailors health care, rather than ensuring the health care itself was actually available. As there were no internal health care providers, this was only available from the medieval equivalent of external providers.
Although this worked well by the standards of the time while naval casualties were few, after 1500 this rudimentary health care system was soon overwhelmed by the sheer number of disabled seamen. It was not until the 1690s, when the Navy began to set up its own hospitals, that a health care system was developed that could manage large casualty numbers, many with exotic conditions not normally seen in Europe. Even at a time when life was cheap, the primary consideration driving this requirement was the need to conserve manpower. It is suggested that the need for an appropriate level of military involvement in non-operational health support, in order to conserve personnel, remains a key consideration in the 21st-century health force preparation process.
Finally, the need for deployed health assets to treat more than just battle casualties, in order to conserve manpower, remains an issue for some ADF operational planners. This, in turn, has ongoing implications for the level of training, status and remuneration of ADF medical officers. Although (unlike their medieval forebears), ADF medical officers can practice both medicine and surgery, in many respects their professional preparation for deployment, whatever their specialty, is still less than ideal. Certainly, in terms of status, there remains a body of opinion within the ADF that Henry V’s listing of surgeons with ‘soldiers, shoemakers, tailors and washerwomen’ is still appropriate!






