Introduction
A previous series of papers have analysed the following functions and roles of military health services necessary to conduct their three elemental and distinct yet intrinsically interlinked missions: providing treatment services, enabling operational capability and facilitating civilian re-integration:1
- ‘Military health support’, pending a better term indicating that, whether deployed or not, all ADF commanders have missions to perform that require targeted health service support2
- Casualty evacuation3
- Humanitarian aid/disaster relief4
- Military medicine capabilities in support of the ADF’s aviation, diving and submarine operations, as well as chemical, biological, radiological and nuclear defence5,6
- Assessing health-related suitability for military employment and deployment7,8,9
- Occupational and environmental health10
- Health promotion11
- Treatment12
It should be noted that these functions and roles are listed in priority order: as one heads up the list, the level of military expertise required to conduct them increases.
These papers have explained why excessive workplace illness and injury rates confirm the need to improve the management of hazards associated with ADF workplaces, with better emphasis on prevention. To this end, a submission by the Royal Australasian College of Physicians to the 2019 Productivity Commission inquiry into veteran’s heath advocated that this would best be achieved by premising the ADF’s health services on a systems- based occupational health strategic model.13 Implementing such a model would entail reassessing the following Fundamental Inputs to (in this case ADF health) Capability or FICs per the Defence Capability Development Handbook:14
- Organisation
- Personnel
- Collective training
- Facilities
- Supplies
- Major systems
- Support
- Industry
- Command and management
This paper was originally the second of a new series that will analyse the ADF’s health FICs that enable operational capability via its health services missions, functions and roles: in this instance the ‘organisation’ FIC (Figure 1). The paper originally intended to be first (to be published in due course) provides an overview to this new series.
Readers should also note that this new series is extensively based on the previous ‘functions and roles’ papers.
The Capability Development Handbook
The Capability Development Handbook describes the ‘organisation’ FIC as employing the—in this case, health—capability within flexible and functional groupings, which have the right balance of competencies, structures, and command and control to do what the capability needs to do.15 To this end, the first issue for consideration is that the ADF’s resources are finite: having the right number of the right people with the right skill sets in the right places at the right time will fail without a structure to guide and direct what they should be doing and how to go about it; on the other hand, having a structure that provides perfect guidance will likewise fail without people to implement it. Therefore, the ADF health services need to be organised in a manner that reflects the limited resources available while maximising effectiveness in conducting their missions. This entails applying a risk management approach regarding health organisational structures that may be less-than-ideal but reflect the resources available. This may have implications for some health professionals (in particular reservists) who choose to participate in organisations like the ADF, whose primary reason to exist does not entail providing health care.
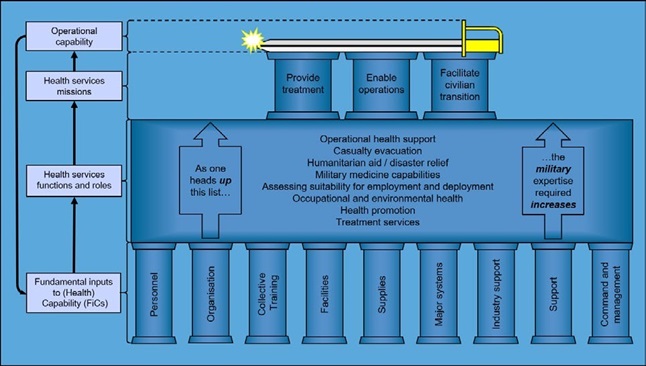
Figure 1: Operational capability and its relationship to military health services missions, functions and roles, and FICs.
Separated versus integrated mission health structure?
To this end, there are two options for how the ADF’s health services can be organised: one comprising three separate components (one for each mission) or one with multiple components (however many), each of which contributes to conducting all three missions. However, although they are separate, the extent to which these missions are inextricably linked demands the latter.
Although their emphasis will vary depending on what, how and when they contribute to providing health services for who and what their missions are, the mission statements for each component within the ADF health services should refer to how they each contribute to all three missions. This could perhaps be achieved per the following template:
‘The mission of [name of ADF health component] is to:
- [directly or indirectly provide/enable/support] ADF treatment services for [ADF target population(s)], by [nature of contribution(s)]
- [directly or indirectly provide/enable/support] the [ADF target population(s) missions], by [nature of contribution(s)]; and
- [directly or indirectly provide/enable/support] the civilian re-integration of the [ADF target population(s)], by [nature of contribution(s)].’
It seems reasonable to assert that this approach will facilitate ascertaining the appropriate health service organisational structures to conduct these missions.
Health service structural development: Top- down versus bottom-up?
The next two options for creating a military health service organisational structure entail starting at the top or ‘strategic’ level and working down to the bottom or ‘tactical’ level (such as individual clinics and other ADF health capability enablers) or vice versa. This paper asserts that a ‘top-down’ approach is more likely to impose one-size-fits-all solutions to accommodate the lowest common denominator, thereby leaving some clinics under-resourced for solving problems they do have and others over- resourced for solving problems they do not have. Furthermore, this approach is more likely to result in top-heavy structures that do not reflect the health services’ size or skill set composition.
On the other hand, a ‘bottom-up’ approach, based on factors such as each clinic’s location (within Australia, at sea or overseas), their target population demographics and the operations they perform, would better enable the higher ADF health organisation to direct the functions and roles required by each clinic to conduct their missions. This would mean the former only have to manage how each of its clinics adapt to changes in their target population(s) and operation(s) over time.
Base health services: Geographic versus functional structure?
The next issue pertains to the ‘operational level’ organisational structure between the ‘tactical level’ clinics (and other ADF health service providers and enablers) in the base setting, and the higher ‘strategic level’ ADF health agency. Analysing the current structure requires some historical background.
All three services—Navy and Army since Federation and Air Force after WWI—initially organised their bases geographically. This made sense when interstate communications were limited to telegraphs and what would now be called ‘snail mail’, moved via ship or train. As communications improved, by the late 1970s the Air Force and Navy health services had become functionally-based organisations, whereby each base health facility reported to a Command Medical Officer at the relevant single-service Support Command. This reflected the high mobility of Navy and Air Force ships and aircraft from their bases and, particularly, Navy’s posting pattern (see below).16,17
On the other hand, the Army health services remained geographically organised as part of the broader Army ‘Military District’ structure into the 1990s. This reflected its initial composition as a regionally-based part-time militia, which was legally barred from deploying overseas until the current Australian Regular Army (ARA) was established in 1947. However, even then, Army maintained this organisational health structure, firstly because the ARA still typically remained in or near their home bases in peacetime, and secondly because of the need to support Army’s non-deployable reserve elements.1
Hence, with the formation of the Defence Health Service in 1997 as part of the Defence Efficiency Review (DER), the geographical health organisation Army had had since 1903 underwent only minor changes before its application to the Navy and Air Force health services Australia-wide. This may have made sense if:
- Their remit only entailed providing treatment services without considering their other two missions: indeed, that was the assumption when these changes were made. However, this would have undermined the DER program’s primary aim of making economies19 in the context whereby health services had long been considered an obvious exemplar of something Defence could easily unify or contract out.20,21,22,23
- All ADF bases have the same However, the extent to which (for example) Stirling mostly supports ships and submarines while Swanbourne exclusively supports special forces personnel and Pearce mostly supports flying training renders this premise at best arguable.
- All ADF members have the same likelihood of being posted to any ADF However, despite the increasingly joint nature of the ADF’s bases, something like 80 per cent of personnel remain likely to be posted to a mostly Navy, Army or Air Force base for the foreseeable future.
- All ADF members had the same posting patterns between However, unlike Army and Air Force, whose non-deployable personnel can remain posted to their unit unless it actually deploys, Navy’s minimum crewing policy for Fleet units means that its non-deployable seagoing members must be landed ashore. The ensuing unplanned postings for compassionate, disciplinary, medical and other purposes mean that Navy’s posting processes are far more dynamic.24
- How Army deploys overseas (i.e. large numbers on an occasional or periodic basis, generally requiring several days or even weeks notice) also applies to Navy and Air 25,56,57 However, not only does Navy have up to 1600 personnel at sea at any one time, but can adapt its operational tempo at far less notice, as shown by its response to Cyclone Tracy in 1974,28 the first Operation DAMASK deployment prior to the 1991 Gulf War,29 and the 2001 evacuation from Honiara in the Solomons (Operation PLUMBOB).30
Hence, despite a succession of reorganisations since 1997, the ADF’s geographically-based military health organisational structure remains unfit for purpose. In particular:
- Continuity of patient care for non-Army members has been fragmented by the extent to which they are posted anywhere within Australia (or, in Navy’s case, ships that routinely deploy overseas). Using the previous example, this paper asserts that it is far more important to ensure continuity of care between Stirling, Kuttabul and Coonawarra (and the ships they support) than between Stirling, Swanbourne and Pearce.
- It should be noted that ADF members only have to be medically suitable to perform the intrinsic requirements of their employed Hence, unless all ADF members have the same job requirements, using the ADF Military Employment Classification (MEC) system to apply a single medical standard (as opposed to the standards themselves) does not comply with the Disability Discrimination Act 1992.31,32
- The misuse of the MEC system as a patient rather than personnel management tool has led to the Chiefs of Air Force and Navy losing control of the health aspects of their personnel ‘raise/train/sustain’ 33 This assertion is based on the increasing proportion of Navy members deemed not fully employable and deployable,34 and the assumption that MOs with comparable workplace experiences as their clientele will provide better-quality medical employability advice than those without. The latter primarily refers to not just preventing those from deploying who should not, but also ensuring that those who can deploy are able to do so. Besides ensuring compliance with the Disability Discrimination Act 1992, this attribute would have maintained credibility with the personnel managers by enabling their clientele’s employability and deployability (hence operational capability) without unnecessarily impinging on their health. It also would have maintained credibility with their clientele by not needlessly hindering their promotions, courses and/or career progression.35
- It has failed to enable the service chief’s workplace health (as opposed to safety) obligations per the Work Health and Safety (WHS) Act 2011.36 This began sometime around 2001 when responsibility for the ADF’s occupational health services was moved from the Defence Health Services to the current Defence WHS Branch, with the following consequences:- Attempting to provide WHS policy support and advice across all of Defence has failed to address the generally higher levels of health risks faced by uniformed personnel, as indicated by their excessive compensatable illness and injury 37,38 This has been compounded by the WHS issues for Defence civilians being more familiar and, in that sense, ‘easier’ to manage. Hence, the single services have had to fill the ensuing gaps with their own WHS services, which lack the resources to put the ‘H’ in ‘WHS’.- The services’ inability to put their ‘H’ in ‘WHS’ is compounded by Joint Health Command (JHC) considering occupational health a WHS branch responsibility and a distraction from providing treatment At the same time, the WHS branch remains unable to fulfil its occupational health responsibilities without developing a parallel health service to JHC. This has been demonstrated by the Occupational Medicine/Occupational Hygiene (OMOH) project between JHC and the WHS Branch, which was instituted in 2010 in response to a succession of fairly egregious occupational health failures39,40 but has made no progress since.41,42,43
Deployed health service structure
From a health perspective, many (not all) deployed health units come under the J07 (Director Health) at Headquarters Joint Operations Command (HQJOC). While accepting this situation is unlikely to change in the foreseeable future, the following issues should be noted for consideration:
- The terms ‘deployed’ and ‘non-deployed’ have been used more or less synonymously with ‘operational’ and ‘non-operational’ since the 1990s: this reflected Army’s succession of Middle East deployments from 2003 to 2021 and Air Force’s OKRA deployments from 2014 to
- However, with the end of these deployments, more ADF operations for the foreseeable future will not entail physically basing anyone overseas: although Air Force will continue to routinely cycle aircraft to Butterworth, most of its operational taskings will be flown from Learmonth, Tindall, Darwin, Scherger, Amberley, Williamtown, Edinburgh and/or Pearce, while Navy and Army will provide Amphibious Task Groups that operate overseas but remain based in Sydney and Townsville. Hence, although the health clinics at these bases clearly do not deploy, they just as clearly will be providing health support for these operational units, thereby blurring their current characterisation as health services without an operational role.
- As previously indicated, not all ADF deployments are force-assigned to HQJOC: both Air Force and Navy routinely deploy aircraft and ships independently, many of which still need health This means Air Force for example, could have two units doing similar things in the face of similar health threats but with different health support arrangements, simply because one is force-assigned to JOC and one is not. This reflects the extent to which HQJOC has had a top-down ’one-size-fits-all‘ approach to health support that is intrinsically inefficient and potentially hazardous.44 This issue confirms the need for greater accountability by at least some J07s at HQJOC and other joint headquarters with respect to applying an informed risk management approach to managing the environmental operational and non-operational health threats confronted by their force-assigned units.
The way forward
There are three components—mostly longer-term— to facilitating the ADF health services’ ‘operational capability’ and ‘civilian transition’ missions in addition to their ‘treatment service’ mission: the first entails changing JHC’s current geographic organisational structure for its base health services into a functional one; the second involves moving the ADF MEC functions to the single-service health directorates, and the third is to return the ADF’s occupational health functions to JHC.
A new functional organisation. In lieu of multiple regional health services, this would entail putting the JHC clinics with mostly Air Force clientele under an O6 Director Air Force Health Services (DAFHS); those with mostly Navy clientele under an O6 Director Navy Health Services (DNHS); and those with mostly Army clientele under an O6 Director Army Health Services (DAHS). These O6s would have two reporting chains: one to a JHC one-star Director Defence Health Services, the other to their single- service chiefs through the latter’s existing O6 health directors.
This functionally-based structure would have the following benefits:
- It gives the clinics the means to conduct all three missions rather than just The fact that 80% of the ADF members at most bases still being expected to be single service explains the O6 Directors’ Canberra presence under a JHC DDHS: while they would each focus on managing how their clinics support their single- service populations, they clearly need to liaise with each other regarding the remaining 20% from the other services.
- It makes the clinics more accountable to the Service chiefs regarding the latter’s ‘raise/train/ sustain’ role and their health-related Person(s) Conducting a Business Unit (PCBU) obligations per the WHS Act.
- Noting the extent to which the ADF relies on the military capabilities provided by aircrew, divers and submariners, who not only comprise 5% of all ADF members but also make up 15–20% of all Air Force and Navy members (compared to only about 5% for Army),45 it makes sense that the health services that support them should be functionally organised.
- Given how they deploy and their far larger proportion of reservists, this structure would still allow Army to maintain its geographic-based structure under a However, centralising the Navy and Air Force health command and management functions will reduce their personnel duplication among multiple ‘garrison’ headquarters, improving their utilisation.
A new MEC process. In lieu of a single JHC agency being responsible for providing medical employment advice, moving this function to the single-service health directorates would:
- improve accountability to the Service chiefs with respect to applying the ADF MEC system as a personnel rather than patient management system
- improve the quality of the advice being provided to the single-service personnel management agencies, both through personal experience of the clientele’s working environment and by improved supervision of MEC Review treating MOs and confirming authorities
- extend the current processes for the ADF’s SPEC personnel to its single-service
A new occupational health structure. In lieu of the Defence WHS Branch maintaining its current responsibilities across Defence, moving its occupational health functions to JHC would acknowledge the extent to which the ADF population is first and foremost a workforce that requires a range of health services related to preventing avoidable workplace-related illness and injury. This will extend their current ‘ambulance down in the valley’ role to enable operational capability and facilitate their clientele’s eventual transition to the civilian community.46 Doing so will also fulfil the intent of the failed OMOH project by enabling the processes by which the clinics can fulfil their responsibilities to the Service chiefs regarding the latter’s ‘raise/train/ sustain’ role and health-related PCBU obligations per the WHS Act.
Conclusion
There has been a longstanding misperception within Defence (including elements within its health services) that, as they only exist to provide treatment services, its health services are an obvious exemplar of something that can be easily unified or contracted out. However, this fails to recognise the other two missions of health services that support military workforces rather than civilian populations: enabling operational capability and facilitating their eventual transition to the civilian community.
Previous papers have explained why excessive workplace illness and injury rates confirm the need to improve the management of hazards associated with ADF workplaces, with better emphasis on prevention. Figure 1 summarises these papers by showing the relationships between ADF operational capability, the three health service missions necessary to enable that capability, the eight health service functions and roles enabling those missions, and the nine FICs they need to conduct them. It also demonstrates how occupational health is intrinsic to all the components of a holistic military healthcare system.
This paper explains why the health ‘organisation’ FIC is not fit-for-purpose in its current form: in particular, the misapplication of a geographically- based organisational structure that does not enable operational capability beyond one of the services in general and Navy in particular. This had been compounded by the misuse of the ADF MEC System as a patient rather than a personnel management tool, and JHC’s non-accountability for enabling the service chief’s health-related PCBU obligations.
The proposed organisational changes per this paper will allow JHC to manage the ‘what’ regarding the functions and roles that the ADF’s clinics need to perform for them to conduct all three missions via its one-star Director Defence Health (not just ‘Clinical’) Services, whose subordinate single-service O6 health directors manage the ‘how’ while also supporting the single-service chiefs’ ‘raise/train/sustain’ role and PCBU obligations via the latter’s health directorates.
As applied to the ADF health services, Figure 1 remains consistent with the meaning of the word ‘joint’, as defined by the then CDF in 2017:
‘I look at where we’ve come to now from back then [1999] and we are well ahead, with a far better understanding that joint isn’t doing everything the same. Joint is about bringing the best of the three services and the public service together to get the best combination you can for that particular operation.’ [underlining added].47
Disclaimer
The views expressed in this article are the author’s and do not necessarily reflect those of the RAN or any other organisations mentioned.
Corresponding Author: Neil Westphalen, neil.westphalen@bigpond.com
Authors: N Westphalen11,2
Author Affiliations:
1 Royal Australian Navy – Directorate of Navy Health CP4-7-150
2 University of New South Wales Canberra at ADFA






