INTRODUCTION
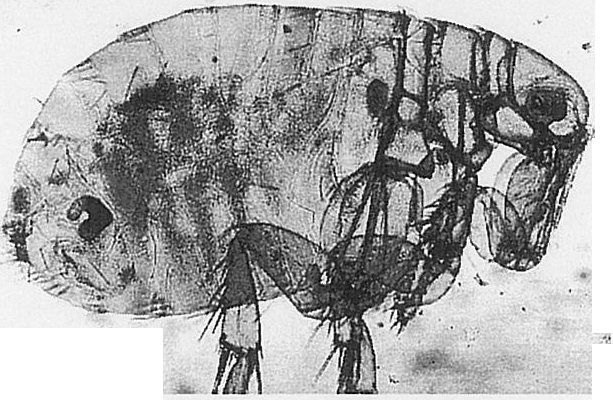
THE PLAGUE, RECOGNISED BY MOST FROM its description as the Black Death, is alive and well today. It is an enzootic disease of peridomestic and wild rodents caused by the bacillus Yersinia pestis. It is spread by the bite of the oriental rat flea Xenopsylla cheopsis. When the rodent population is reduced through death brought about by epizootic proportions of the disease, the flea finds other hosts. If there is contact between human and rodent populations, such as existed early this millennium, and that occurs due to population movements as a result of disaster or wars, then outbreaks of the plague in humans can occur.
The plague is subject to quarantine and reporting by International agreement through the World Health Organisation (WHO). Its relevance to Travel Medicine is in its history of global spread over the centuries and the effect of disasters, wars and possibility of development of antibiotic resistance on its possible resurgence.
HISTORY OF THE PLAGUE
Plague has been with us throughout recorded history. It is a disease associated with the movement of human populations and trade.
Biblical Times
It is mentioned in the Book of Samuel in the Old Testament of the Bible.’
Justinian Epidemic (AD 543)
This epidemic, starting at the time when Justinian I was Emperor of Rome, lasted some two centuries. It is believed to have spread from India or Central Africa by rats on board seagoing vessels, initially into Egypt and thence into the coastal areas surrounding the Mediterranean, into Western Europe and possibly as far as the British Isles. The death toll is thought to have been as high as 10 million people throughout Europe. At the same time that Europe was being devastated by the plague, ships trading between India and China were also carrying the disease.’
The Dark Ages
The result of the massive reduction in the population of Europe caused by the Justinian Epidemic was the breakdown of administration and civilisation in what became known as the Dark Ages. Little is known about the plague during this time. What literature is available makes scant mention of the existence of plague and one wonders whether it had ceased to be a problem.’
The Twelfth Century
During the Twelfth Century, increased communication between Asia and Europe occurred because of the overland caravan and the conquering Mongol armies of Genghis Kahn. This situation, along with the use of the Silk Road between China and Syria, increased the contact of the burrowing rodents of the Steppe with human and animal carriers of the plague from areas of India, China and the Himalayan foothills. This movement of human carriers into areas previously clear of the plague set the stage for the Black Death.
The Black Death (AD 1347)
From 1348 to 1350, the plague devastated much of Europe. It was called the morsater, which translated means terrible or black death. It was believed to have originated in Caffa in the Crimea around 1347. Caffa was under siege by a Mongol prince. Plague broke out amongst the besiegers.
Historical reports claim that the besiegers catapulted the bodies of plague victims over the walls of the besieged city. This is an early example of the use of biological warfare. It is suggested that some of the inhabitants of Caffa, fleeing the siege by Genoese ships, carried the plague with them to ports such as Venice, Messina and Genoa. From there it spread across Europe. It is estimated that throughout Europe approximately 25 million people died as a result of the Black Death

Oberammergau and the Passion Play
The impact of the plague was so dramatic on many areas of Europe that even today its influence can be seen in some social traditions. One of the most interesting examples I have found is that of the story of the Passion Play enacted every ten years in the little town of Oberammergau in the Bavarian Alps since It is reputed to have been started after the people of the town vowed that if they were spared from an epidemic of the plague, they would celebrate with a Passion Play.
The Great Plague of London (AD 1665)
The Great Plague killed an estimated 70,000 out of a total population of around 460,000 people in London. Changes had occurred in building materials utilised since the Black Death. More houses were built out of stone rather than wood and tiles were used in place of thatch. This and the use of quarantine meant that this epidemic, by comparison with earlier episodes, was relatively short-lived. The Great Fire of London in 1666 further reduced the number of wooden and thatch structures. The reconstruction that followed reinforced the trend towards living conditions that reduced the impact of rodents on the human population.
China (AD 1894)
In 1894, outbreaks in Hong Kong and Canton left some 80,000 to 100,000 dead from the plague. A further 10 million deaths worldwide were attributed to the plague over the next twenty years after its spread from the southern Chinese ports.
Twentieth Century
Small outbreaks of the plague have occurred through out this century. Between 1900 and 1906, Western Australia had 80 cases. Cases of the plague continue to occur in areas of Asia, Africa, North and South America, with the most recent being an outbreak in Namibia.
” Plague continues to be enzootic in wild rodent populations over large areas of the Americas, Africa and Asia, with occasional outbreaks among commensal rodents in villages and small towns. Wild rodent plague poses a real, though the limited, risk to humans. When the infection spreads to rats in urban or populated areas, humans are at markedly increased risk of exposure. In the past several decades, however, urban outbreaks have been rare and limited in size. Wild rodent plague exists in the western third of the United States, in widely scattered areas of South America, in north-central, eastern, and southern Africa, Madagascar, Iranian Kurdistan, along the frontier between Yemen and Saudi Arabia, Central and Southeast Asia (China, India, Indonesia, Kazakhstan, Mongolia, Myanmar [Burma], Vietnam), and portions of the Russian Federation. In recent years, human plague has been reported from the African region from Angola, Botswana, Democratic Republic of Congo (Zaire), Kenya, Libya, Madagascar, Malawi, Mozambique, South Africa, Tanzania, Uganda, Zambia and Zimbabwe; in Asia from China, India, Kazakhstan, Laos, Mongolia, Myanmar (Bunna), and Vietnam; and in the Americas from Bolivia, Brazil, Ecuador, Peru and the United States. Risk to travellers in any of these areas is small.”‘
The incidence of plague worldwide continues to rise. The average number of cases reported to the WHO in the 1980s was 861 cases per year. By the 1990s it had risen to 2025 per year.”
The plague is reportable to the World Health Organisation under the International agreement. Isolation of cases of the plague are responsible for reducing its spread despite the speed of travel.
“For international travellers, international regulations require that prior to their departure on an international voyage from an area where there is an epidemic of pulmonary plague, those suspected of significant exposure shall be placed in isolation for 6 days after last exposure. On arrival of an infested or suspected infested ship, or an infested aircraft travellers may be disinsected and kept under surveillance for a period of not more than 6 days from the date of arrival. Immunization against plague cannot be required as a condition of admission to a territory.”

THE DISEASE
The plague is a disease of rodents. It is transmitted from rodent to rodent, other mammals and man by the bite of the oriental rat flea, Xenopsylla cheopsis. For humans to become part of the transmission cycle of the disease, certain factors need to exist. The rodent population must be infected with the bacillus Yersinia pestis. At some point, the disease reduces the rodent population and the flea seeks new hosts. There needs to be sufficient contact between rodents and humans allowing for humans to become the alternate hosts for the flea.
“Initial signs and symptoms may be nonspecific with fever; chills, malaise, myalgia, nausea, prostration, sore throat and headache. Commonly lymphadenitis develops in those lymph nodes receiving drainage from the site of the flea bite, where there may be an initial lesion. This is bubonic plague, and it occurs more often in lymph nodes in the inguinal area (90%) and less commonly in those in the axillary and cervical areas. The involved nodes become swollen, inflamed and tender and may suppurate. Fever is usually present. All forms, including instances in which lymphadenopathy is not apparent, may progress to septicemic plague with bloodstream dissemination to diverse parts of the body, including the meninges. Endotoxic shock and disseminated intravascular coagulation (DIC) may occur without localizing signs of infection. Secondary involvement of the lungs results in pneumonia; mediastinitis or pleural effusion may develop. Secondary pneumonic plague is of special significance, since respiratory droplets may serve as the source of person-to person transfer resulting in primary pneumonic or pharyngeal plague; this can result in localized outbreaks or in devasting epidemics.”
THE VACCINE
The plague vaccine available in New Zealand is produced by CSL, Australia. It is an inactivated vaccine made using agar-grown, heat-killed organisms of Y. Pestis in saline containing 0.5 per cent w/v phenol as an antiseptic.
Plague vaccine is not required as a condition of entry into any territory. Use of the vaccine is believed to confer some protection on the individual, increasing the chances of recovery from the bubonic form of the plague. Its protection to the pneumonic form of the plague or aerosol exposure is presumed to be ineffective.
The vaccine is given subcutaneously. It is given as two doses between one and four weeks apart in those over 12 years and three doses for children under 12 years. Dosage is age-related (as outlined in package insert). Booster doses are given every six months for those persons living in areas where plague is prevalent.
The dosage regime for the plague vaccine licensed for use in the US differs from that used in NZ. The primary series consists of an initial dose followed by two smaller doses at 1-3 months later and then 5-6 months after the second dose. Three booster doses then follow at 6-month intervals after the third dose of the primary series.
TREATMENT
The plague is readily treatable with antibiotics. Persons suspected having the plague should be placed in strict isolation.
“Streptomycin is the drug of choice, gentamycin can be used when streptomycin is not readily available; tetracyclines and chloramphenicol are alternative choices. All are highly effective if used early (within 8-24 hours after onset of pneumonic plague).”
Streptomycin is given at 30mg/kg/day (IM) in two divided doses for ten days, however, it can be difficult to obtain in some parts of the world. Intravenous doxycycline 200mg initially, followed by 100mg every 12 hours for 10-14 days is also effective.
Contacts should be given a course of antibiotic, either oral tetracycline or co-trimoxazole. For contact with patients with pneumonic plague, doxycycline is the drug of choice, given 100mg orally twice a day for seven days or for the duration of risk of exposure.
SOURCES of INFORMATION
Travel medicine specialists need to be aware of the worldwide incidence of plague and of any current outbreaks of the disease. There are many sources of this information. The World Health Organisation provides information about areas of plague in its publication, International Travel and Health: Vaccination Requirement s and Health Advice. This book is published yearly and should be part of the library of a travel medicine clinic. It is available electronically at http://www.who.org/ith/english/ind ex.htm.
VVHO has a site on the Internet, www.who.int/wer, which contains the World Epidemiological Record (WER). This can also be subscribed to via email PROMED, another Internet source of up to date information is available as an email digest. It can be accessed at www.healthnet.org/programs/promed. html.
RELEVANCE TO THE MODERN TRAVELLER
Plague risk to travellers today is small. There are still areas of risk and these must be pointed out to the intending traveller. Those that will be staying in areas of plague foci for periods in excess of thirty days, such as missionary and aid workers, members of the military and those who are adventurous travellers are most at risk.
The traveller’s itinerary must be ascertained as this will throw some light on the advice to be given. For instance, a traveller to Namibia, going for a year as an aid worker and staying in accommodation of unknown standard in rural areas close to the latest known outbreak of the plague is at risk. On the other hand, a visitor to South Africa, who has friends living in the capital of Namibia, and intends to go see his friends for a couple of days is unlikely to be at risk.
” Immunisation of visitors to epidemic localities and of laboratory and field workers handling plague bacilli or infected animal s is justifiable but should not be relied upon as the sole preventive measure.”
Plague vaccine is available, but its use is limited. It is essentially only useful in preventing bubonic plague.” It is not considered effective against the pneumonic form. Where travellers are considered to be at risk, consideration should be given to the use of short term antibiotic chemoprophylaxis using doxycycline or tetracycline during periods of risk7. It is important that those at risk are educated about the disease and how it is spread, the strategies that can be employed to reduce risk of exposure and what to do if the plague is contracted.
It should be stressed that the first line of defence is the use of good preventive medicine practices. This includes choice of living arrangements, care with rubbish disposal, awareness of presence of rodents in the area and use of personal protective measures. Care must be taken if reduction of any rodent population is contemplated that the first action is the use of insecticides to reduce any fleas in the area. Killing of the rodents without care for fleas may result in the fleas looking for new hosts, one of the causes of plague spread.
Secondly, use of insect repellents on exposed skin and use of permethrin for impregnation of clothing and bednets may reduce the risk of contact with fleas. This is good advice for any traveller to areas of insect-borne disease.
Perhaps some comment on the possibility of spread via household pets in areas of risk should also be mentioned. For instance, it is known that cats can develop pharyngeal plague and that this can be passed to humans causing pneumonic plague.
” Seventeen cases of primary plague pneumonia were acquired from pet cats with plague pneumonia in the interval 1977-1994.”
THE RETURNING TRAVELLER
It is important to be aware of the plague as a possible infection among travellers despite the small risk.
” Medical personnel should be aware of areas where the disease is endemic and early entertain the diagnosis of plague; unfortunately, plague is often misdiagnosed, especially in travellers who develop illness after returning from an endemic area.”
CONCLUSION
Historically the plague is a disease of contact between humans and populations of infected rodents and their fleas. It has been spread as a result of travel, either by carriage of the disease on infected persons or movement of rodents or fleas in the baggage and transport of humans.
It still occurs in areas around the world, but the epidemic proportions of the Black Death are now part of history. Its control is due largely to International Regulations, isolation of cases of the plague and the bacteria’s susceptibility to the use of antibiotics.
This does not, however, mean we should be complacent. Factors exist today for an epidemic of huge proportions to occur should only a few factors change. Firstly, the number of wars around the globe threatens its control in many areas. Secondly, the speed of travel and the potential for movement of infected people and rodents and their fleas. And finally, the ability of bacteria to become resistant to antibiotics. A change in any one of these factors could be all the trigger the plague needs to once again become “the Black Death”.






