Introduction:
Can you hope to save me one Division in the next advance and keep my men on their legs? GEN. Edmund Allenby, Jerusalem 19181
Military plans often do not survive intact when first contact occurs with the enemy, whether the enemy is human or a micro-organism. One tries to anticipate threats and the required organization to meet them, but modifications are always needed to adapt to actual circumstances. Epidemic outbreaks of infectious disease are the most obvious medical threats to military operations and are common in the Middle East. At the end of the First World War an entire British Army was forced to stop military operations just as they managed to defeat the opposing Turkish forces in Palestine.2, 3 Simultaneous outbreaks of epidemic falciparum malaria and pandemic influenza made tens of thousands sick and killed more than 1,700 (166 Australians from a total uniformed strength approximately 17,000 in the AIF).4, 5 Royal Australian Army Medical Corps personnel formed new medical units to address infectious disease problems they encountered during Middle Eastern operations in 1916-19. Addressing the actual question posed by Army Commander General Edmund Allenby to CAPT. Philip Manson-Bahr (shown above) required flexible, innovative thinking and rapid reorganization of existing medical units.1 It is likely that such evolutionary behaviour will be required during future operations in developing countries, especially those disrupted by war or natural disaster.
ANZAC Field Laboratory:
Among the new medical units which were evolved to meet the unforeseen requirements of the war, none in the history of the Australian Medical Services is more worthy of note. COL. R. W. Downes, Canberra 19382
Figure 1: ANZAC Field Laboratory at Bir El Abd, Sinai, Egypt 1916; Australian War Memorial photo B02849
In August 1916 there was a cholera outbreak among troops in transit camps in the Sinai desert. Due to the potential for severe disease and mortality from cholera (the 1896 epidemic in Egypt killed more than 100,000 civilians), the commander of the Military Bacteriological Laboratory in Alexandria and formerly of the Lister Institute, LT.COL. C. J. Martin, set up a medical unit to conduct local investigations to support the anticipated need for ‘diarrhoea camps’.6 This temporary laboratory’s mission was to stop cholera from crossing the Suez Canal and reaching the civilian population on the Nile. It subsequently evolved into the ANZAC Field Laboratory shown in the Egyptian desert in Figure 1.6 Initially located at kilometer 47 along the Kantara Railway, the lab consisted of one medical officer and three other ranks, eventually growing to seven personnel drawn from the Australian Imperial Force (AIF). Fortunately the cholera threat passed and the ANZAC Field Laboratory was assigned other duties to supplement the two fixed-facility Military Bacteriological Laboratories in Egypt. Assigned to the Desert Mounted Corps, the ANZAC Field Laboratory’s light establishment was designed to closely follow the mounted forces. It was usually attached to a field ambulance on orders to be able to move in less than 8 hours.7 In its first year of operations, the ANZAC Field Laboratory moved nine times covering 230 km moving across the Sinai and then north into Palestine.7 Movement could be by train, motor vehicle (shown in Figure 2) or camel (the lab consisted of 19 camel loads).

Figure 2: ANZAC Field Laboratory loaded on wagons in Gaza, Egypt prior to movement in 1916; Australian War Memorial photo B02805
Besides diarrhoeal diseases (cholera and bacillary dysentery) the laboratory could also test for diphtheria, meningitis, sexually transmitted diseases, parasites (malaria, schistosomiasis, leishmaniasis and trypanosomiasis), tuberculosis, gas gangrene (anaerobic bacteria), enteric fever (typhoid) and typhus.6 Separate investigations detected human diphtheria carriers, relapsing fever (a type of bacterial sepsis) and anthrax infections in horses. Dysentery had been a major medical cause of casualties at Gallipoli and most of the diarrhoea-related work of the ANZAC Field Laboratory was to detect shigellosis (bacillary dysentery). Vaccines and sera were kept by laboratories and one of the ANZAC Field Laboratory’s function was to give preventive injections of horse anti-tetanus toxin to wounded troops.8 Further reorganization occurred in 1917 while attached to the 1st Light Horse Field Ambulance. The lab was split into mobile and fixed sections (three men each). Turkish prisoners of war were examined for cholera as a means of stopping introduction into British forces. Chemical analyses were done to check drinking water supplies for bacterial contamination and residual chlorine.
The arduous task of maintaining a military force in the Jordan Valley in 1918 was assigned to Chaytor’s Force, which included the ANZAC Mounted Division.2 The Jordan Valley was generally felt to be uninhabitable during the hot, dusty summer. Once attached to the ANZAC Mounted Division in June 1918, malaria became the primary focus of the ANZAC Field Laboratory. Initially this was to support prevention measures such as mass quinine administration and engineering works to drain mosquito breeding areas. A large number of the infantry previously infected with malaria in Salonika (modern Greece) had been moved to Palestine where they became a source of infection.9 To give a sense of the scale of these antimalarial operations, in 1918 more than 111,000 malaria slides were read by three laboratories (ANZAC laboratory in Jordan Valley, #2 Military Laboratory in Ludd and #3 Military Laboratory in Jaffa), of which about 1 in 5 were positive.2 From 19 Sep 1918 a coordinated offensive rapidly moved more than 300,000 soldiers north, the cavalry covered up to 100 km per day. The ANZAC Field Laboratory was only partially mobile so while most of the unit stayed in Jericho, two men and two microscopes were moved forward to Amman, Jordan during the malaria epidemic of October 1918 in the 1st Australian Light Horse Brigade. The ANZAC Field Laboratory was subsequently assigned to the 5th Cavalry Division. They finished their war service attached to the Divisional Hospital which was set up on the grounds of a Turkish school; the farthest AIF unit north was in Aleppo, Syria. The epidemiology of the simultaneous malaria and influenza epidemics, and the subsequent impairment of military operations, has already been described both by MAJ. Eustace Ferguson, the Laboratory Officer in Charge, and in a later historical review.4, 7, 10
During its greater than 2 year existence, 15 men served in the ANZAC Field Laboratory. Most were from the Royal Australian Army Medical Corps (RAAMC), but there was one Royal Army Medical Corps (RAMC) medical officer and two New Zealand Army Medical Corps (NZAMC) other ranks. The unit’s casualty list demonstrates how high a price our military medical predecessors paid to accomplish their historical mission. Two men died of falciparum malaria and three were evacuated with either malaria and/or influenza in late 1918. Four men had previously been sent to hospital for several weeks treatment and convalescence for dysentery.7 The laboratory was under nighttime aerial bombardment while at El Arish, but suffered no combat injuries.
5th Malaria Diagnosis Station:
The clinical type was a very severe one, and there were many fatal cases. The diagnosis stations attached to the cavalry divisions were able to accompany them to Damascus. CAPT. Philip Manson-Bahr, London 1920.11
During the summer of 1918 it became apparent that although malaria could be controlled to a manageable level while on fixed lines, if and when the troops moved north into Turkish controlled territories they would be exposed to high levels of malaria transmission. In order to prepare for this eventuality, CAPT. Philip Manson-Bahr (RAMC), approached the Commanding General and requested authority to form six small mobile malaria diagnosis stations with the intention of providing rapid diagnosis and treatment to all febrile soldiers regardless of how rapidly the cavalry advanced into enemy territory. General Allenby responded with “Can you hope to save me one Division in the next advance and keep my men on their legs?”; upon receiving a positive answer he further stated to his quartermaster “Give this young officer everything he asks for”. One should hope for such a decision from a senior line officer, as only when combatant officers take disease prevention seriously in order to maintain their forces in the field, will diseases such as malaria be controlled.

Figure 3: Staff of 5th Malaria Diagnosis Station attached to 5th Cavalry Division at Homs, Syria in Jan 1919; front row PTE. A. J. Hardy, CAPT. C. C. Chesterman, PTE. Jeffery; back row unidentified batman and RASC driver.
Australian War Memorial photo B01051
A Malaria Diagnosis Station originally consisted of one medical officer and two other ranks who had each received a month’s special instruction on how to stain and search microscopic blood smears for malaria parasites.11 In Figure 3 the 5th Malaria Diagnosis Station is shown with one medical officer (CAPT. Clement C. Chesterman RAMC) and four other ranks. By April 1918 these small diagnostic teams were deployed (two per Army Corps), in anticipation of a military offensive later in the year. Their equipment consisted of one wagon, two microscopes, three tables and four horses. This very light establishment was intended to allow the stations to move rapidly behind the cavalry, across a desert with few roads or railroads.11 Besides providing current epidemiological information for public health purposes, the goal of fast and accurate diagnosis was the rapid provision of the only effective medication, quinine, usually by intramuscular injections. The alkaline nature of quinine solutions caused tremendous pain on intramuscular injection, leading some medical officers to favour intravenous quinine administration.12
The last great cavalry battle ever started on 19 September 1918 when British infantry broke the Turkish line, followed by three cavalry divisions (largely Indian and Australian units) moving as rapidly as possible up the coast to cut off three Turkish Armies retreating north through the Jordan Valley. The 5th Malaria Diagnosis Station was attached to the Australian Mounted Division and 6th Malaria Diagnosis Station was attached to 5th Cavalry Division.3, 11 Within a single incubation period (10-14 days), leading cavalry units had moved into Damascus and a major malaria epidemic had started. During the second week of October, more than 1,800 new malaria infections were diagnosed and pandemic influenza had broken out.13 Military operations largely ceased as over-extended units tried to evacuate their sick (who out-numbered the battle wounded by a factor of 37) hundreds of kilometers back to military hospitals.2, 4 The 4th Cavalry Division was the only cavalry division unsupported by a Malaria Diagnosis Station. The 4th Cavalry Division was unable to regain momentum following the twin infectious disease epidemics, and at one point it barely had men well enough to feed their horses and was unable to join the 5th Cavalry Division in their eventual movement to Homs and Aleppo, Syria.

Figure 4: 5th Malaria Diagnosis Station when attached to 5th Light Horse Casualty Clearing Station in Damascus, Syria Oct 1918; PTE. Hardy, PTE. Jeffery, CAPT. Chesterman (standing); Australian War Memorial photo B01070
Fortunately for the British Army the Turks had already been defeated in the first two weeks of the campaign and were suffering even greater disease casualties than the Allies. The 5th Malaria Diagnosis Station laboratory set up in Damascus is shown in Figure 4; it was the first Allied laboratory unit in Damascus in October 1918 when nearly all medical arrangements collapsed due to the large number of Turkish POW casualties. CAPT. Chesterman later noted “Thousands died of the combined influenza and malaria, but we got there just in time to diagnose many hundreds of cases just at the end of the pre-patent or incubation period. Our little laboratory worked in shifts for 16 hours each day, and I went round to all the hospitals collecting blood smears. But there was a holocaust, and mass graves were filled daily.”14 The Australian 5th Malaria Diagnosis Station ended its war service in Homs, Syria. By that stage, the unit was largely working with sick prisoners of war and civilians.
Although it is arguable whether General Allenby’s question had been answered correctly, rapid diagnosis and treatment did avert a medical disaster from being even greater. The six Malaria Diagnosis Stations made over 40,000 blood examinations during their short existence, of which 11,557 contained malaria parasites. Although little could be done for soldiers with pandemic influenza, by detecting the men that were co-infected with malaria, quinine could be given in a rational, life-saving manner.13, 15 For as yet unclear reasons, pandemic influenza appears to be synergistically lethal when it occurs in soldiers with falciparum malaria, an observation made by MAJ. N. Hamilton Fairley, who later became the Australian Army’s chief malariologist during the Second World War as well as the Director of Land Headquarters Medical Research Unit, a forerunner of the Army Malaria Institute.16, 17
7th Mobile Sanitary Section:
A new feature in health control was developed in the provision of mobile sanitary sections attached to cavalry divisions. MAJ. Harvey Sutton, Brisbane 1919.18
Sanitary Sections were vital to maintaining troops in the field, despite their unglamorous tasks of dealing with food, water, excreta and insect infestations. The challenge facing the Sanitary Sections in Palestine in 1918 was the same as the other medical units: how to become sufficiently mobile in order to accomplish their functions within a cavalry division. The Mobile Sanitary Sections had to be formed by special order of the AIF commander in June 1916 as no such unit had ever been an organic part of a mounted formation. The 7th Mobile Sanitary Section was originally attached to the Australian New Zealand Army Corps (ANZAC) Mounted Division, whereas the 8th Mobile Sanitary Section was attached to the Australian Mounted Division. That it took a year for the 7th Mobile Sanitary Section to become truly mobile when it received its own horses, gives some indication of the lack of importance usually given to these vital administrative functions. Figure 5 shows the 8th Mobile Sanitary Section mounted as it was constituted in 1917. Although establishments varied, most Sanitary Sections consisted of about 20 men.
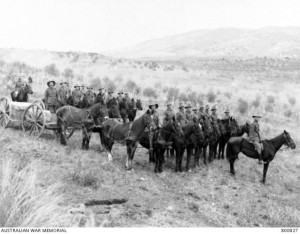
Figure 5: 8th Mobile Sanitary Section attached to Australian Mounted Division circa 1917; Australian War Memorial photo B00827
The hostile desert produced many practical difficulties for maintaining the health of human and animal populations in hot, dry, dusty areas. Cavalry units produced enormous amounts of horse manure which had to be disposed of in addition to human faeces. In 1918 Egypt and Palestine presented particular problems due to the difficulties of communication and transport, which greatly complicated all preventive medicine functions. In the SinaiDesert camels were one of the few transportation options. Latrines (5 seats in a single bench box) were devised such that they could be transported by camel.
Water was a supremely valuable resource in the desert and the entire military campaign was planned around the need to capture water sources for both men and animals. The main water source for the Desert Mounted Corps was the canal in Kantara which was fed from the NileRiver. As the water in Kantara resembled dilute sewage, it was first strained, clarified by alum and followed by sand filtration under pressure. The need to chlorinate water prior to its use for drinking was also an important sanitation function, often disliked by the soldiers due to the taste of chlorine. Water was then moved via pipeline along the coast advancing with the soldiers.2 Water delivery to the units in the field often depended on camels using specially designed rectangular metal cans holding 10-12 gallons. Mobile Sanitary Sections in the AIF became the primary construction force for water containers, latrines, incinerators and food storage facilities for the mounted divisions in the absence of sufficient engineers.2
Where there was adequate humidity, as in the Jordan Valley, insect pests such as flies and the Anopheline vectors of malaria were particularly problematic.19 Flies were a constant issue in desert warfare; dysentery had been a major problem on Gallipoli and great efforts were made to avoid a repeat of the situation in Egypt. Latrines and refuse pits were covered with oil-soaked sacking to discourage fly breeding. Drying of horse manure prior to its use as road material limited some fly breeding. Temperatures often rose above 43°C which was useful for eliminating fly breeding. This all occurred prior to the synthesis of any useful chemical insecticides; formalin and arsenic were tried by the Sanitary Sections with limited success. Expert entomological advice regarding the nature and habits of insect vectors of disease was available from MAJ. Edward Austen (RAMC) who was the entomology curator at the British Museum. Using engineer and labour troops, streams were canalised and swamps drained to prevent malaria as shown in Figure 6.3, 20 As previously stated this engineering effort was successful until offensive operations moved the battlefield north into new areas.

Figure 6: Sanitary Section eliminating mosquito habitat by draining areas in the Jordan Valley circa 1918; Australian War Memorial photo B00228
Masses of dead animals were the inevitable product of large cavalry units and disposing of animal carcasses, preferably by fire, was a constant effort for Mobile Sanitary Sections.18 Fuel and building supplies remained a challenge in the near treeless desert. Delousing stations were important to prevent typhus despite the difficulties of providing washing facilities; a railroad based high-pressure steam disinfector was devised and used for entire brigades with 1,000-2,000 men accommodated over 1-2 days.2
Discussion:
The Middle East has been torn by warfare for centuries. This was true for the AIF during the First World War and is also true currently with the civil war in Syria, only the largest and bloodiest of many armed conflicts in the region. It is ironic to realize that although the battle against malaria in the Middle East was won with parasite eradication occurring more than a generation ago, human conflict continues in the same towns where the AIF medical units were stationed during 1918. The ANZAC Field Laboratory redeployed to Australia from Aleppo in January 1919 and the 5th Malaria Diagnosis Station was disbanded in Homs, Syria. Australian forces may well face similar preventive medicine issues in the Middle East in the future.
Each war presents its own health problems which are often exacerbated when the conflict involves developing nations without medical or industrial infrastructure. Although our scientific predecessors did not have much to offer infectious diseases patients in the pre-antibiotic era, it is not inconceivable that a similar situation may evolve with the rapid spread of multiply drug-resistant micro-organisms. The medical officers of the Australian Imperial Force found many unfamiliar challenges when they arrived in Egypt. Over the four years of the war, RAAMC personnel evolved the best answers they could to their problems, often with little other than their ability to think. Key to their largely successful response in the face of the massive casualties created by simultaneous malaria and influenza epidemics in 1918, was their ability to form new and flexible medical units specially adapted to the local situation. It is highly likely that such adaptations will be required during future armed conflicts.






