Abstract
Contemporary battlefield trauma surgery in the Middle East Region has been characterised by aeromedical evacuation by rotatory wing (RWAME) with relative impunity. Therefore, future health planning needs to consider an environment whereby RWAME movement may be degraded or denied by a near-peer, peer or superior threat. To that end, an exploration of alternative approaches to surgical management of injured personnel is pertinent.
Life-saving surgical intervention may be delivered by deploying mobile surgical assets forward rather than relying on evacuation of casualty rearward. Shortly after the arrival of surgical resources to the point of injury, temporising damage control procedures may begin, removing the delay associated with casualty preparation, package and transfer. Essentially, the concept is to significantly augment Role 1 activities for a time-limited period to increase the evacuation window allowing patients to survive that would otherwise die on the battlefield if rapid evacuation capability was degraded or denied.
An exploration of the surgical procedures, anaesthetic considerations and transport logistics associated with these interventions is presented in this paper.
Limitations on the concept include tactical training requirement of forward deployed medical staff, definition and description of surgical intervention offered and prerequisite civilian skillset, attendant load list, and considerations of anaesthetic delivery and casualty hold elements.
Background
Contemporary treatment of traumatic military injuries in the Middle East Region (MER) has been facilitated with rapid evacuation of injured personnel to progressively higher levels of care. This has principally been achieved using dedicated rotary wing aeromedical evacuation (RWAME) platforms. Coalition air superiority has been assured throughout these most recent conflicts, and so RWAME has operated in a largely permissive air environment.
Future health planning needs to consider an environment whereby RWAME movement may be degraded or denied by a near-peer, peer or superior threat. To that end, an exploration of alternative approaches to the surgical management of injured personnel is pertinent.
The clinical outcomes that became a defining feature of recent operations in the MER were reliant on a mature medical system with a large and firm infrastructure footprint. A fully established medical system linked point of injury with higher echelons of care through to repatriation. These are not likely to be present in any of the following scenarios: the early phases of a heavily contested future military conflict; a conflict involving special warfare troops operating largely unsupported with a partner force; the early phases of a non-contested regional disaster mission; or in the initial phase of a peacekeeping operation.
In any operational scenario where movement is restricted, or in an environment with under- developed medical infrastructure, timely and optimal treatment of the injured soldier on the ground at or near the point of injury becomes an essential precondition for success.
An initial approach is to ensure on-scene integral medical technicians are capable (both in skillset and equipment) of performing life-saving procedural interventions to extend survivability on the battlefield prior to transfer to higher levels of care. Ultimately, evacuation is still required for the patient to reach surgical care quickly. However, this necessitates either outbound and inbound personnel and platforms—whether dedicated or opportunistic.
Alternatively, life-saving surgical treatment may be delivered with greater effect by deploying mobile surgical assets further forward. Shortly after the arrival of surgical resources to the point of injury, temporising damage control, life-saving surgical intervention may begin. This removes the inevitable delay associated with casualty preparation, package and transfer of an injured patient at both ends of the evacuation continuum.
Following temporising on-scene surgical intervention, evacuation to higher level echelons of care providing definitive interventional management remains essential, but death from exsanguination secondary to otherwise non-compressible truncal haemorrhage, in particular, may be avoided and more timely control of gross intraabdominal contamination may be achieved. This is relevant given that approximately 90% of combat-related deaths occur prior to the casualty reaching a medical treatment facility.1
In this discussion paper, we consider the spectrum of forward surgical and anaesthesia intervention necessary for improved survivability of the battle casualty, and associated transport and logistics.
The obvious liability of this paradigm is risk—both to highly specialised (and difficult to replace) medical assets and to the combat medical system more broadly if these assets are taken from larger facilities. Tactical training of forward surgical personnel is time consuming to teach, degradable and mastery is not easily achieved. However, a minimum standard of tactical proficiency is necessary and must be maintained by all far-forward staff. Some level of integrated force protection will still be required as medical assets will always remain non-combatants. This is relevant given the increasing proportion of injuries sustained during special warfare operations with coalition or host nation partners. Inserted or integral surgical assets cannot be allowed to represent a significant tactical liability to the receiving unit, nor can they necessarily consume excessive tactical assets for security from the unit they are supporting.
Considerations of the makeup and readiness requirements of forward surgical teams align with the current Army Capability Establishment Review (CER) terms of reference relating specifically to producing a versatile workforce that offers agile response options. The adaptability of a lightweight, highly specialised team allows use in many contexts (both permissive and non-permissive). Additionally, refining the selection of members into these teams will provide training efficiency and generate capability by leveraging existing civilian expertise in advanced trauma care applied to the austere, high- threat environment—rather than expecting a pool of generalist clinicians to apply clinical skills they have not mastered in an unforgiving and low-resource setting.
A Role 2 Light Manoeuvre element currently exists in the Order of Battle (ORBAT) of the 2nd General Health Battalion (2GHB), and this cell is replicated as a Role 2 (Forward) (R2[F]) in the forthcoming proposed Health CER 2nd Health Battalion (2HB) ORBAT due for implementation in 2022. The organisational and structural makeup of this is not yet confirmed. However, the utility in far-forward intervention is not the intention of this element, but rather the R2(F) is expected to fulfil a role of interim surgical capability while a more formal Role 2 (+/- Enhanced) structure is established. Therefore, in the future health capability of Army, a provision for far- forward surgical care is still lacking.
Historical considerations
Initially, during the early stages of Operation ENDURING FREEDOM, surgical support to ground troops was provided by US Army Forward Surgical Teams (FST). Very early into the operation, these teams were split into two, ten-man surgical teams capable of performing initial resuscitation, emergency trauma surgery, limited critical care and low dependency holding.
These ten-man teams ultimately became known as Split Forward Resuscitative Surgical Teams (Split FRST). As forces pushed further away from Forward Operating Bases (FOBs), the demand for lighter and more mobile surgical teams developed. These teams needed to stay within a tactical leap of their supported forces but still be able to provide the same level of initial care of the ten-man Split FRST’s.
Various acronyms emerged for these teams, including Special Operations Surgical Teams (SOST), Expeditionary Resuscitative Surgical Teams (ERST) and Golden Hour Offset Surgical Teams (GHOST). These teams consisted of between five to eight personnel and were designed to perform between one and three Damage Control Surgical (DCS) cases on casualties who were deemed too unstable to reach a fixed Role 2 facility collocated with a FST. Their equipment was light and scalable, able to be deployed in anything from large man packable kits with a total weight of 150 kg up to 4000 kg of medical stores for a more static operation.
Australia has utilised mobile tactical surgical teams in the past, notably with the Parachute Surgical Team (PST) that was raised in the 1990s to provide Role 2 resuscitation, surgery and holding for a Parachute Battalion Group (PBG) consisting of 1500 troops. The PST was on the same notice to move as the troops it supported and was staffed by a mixture of regular and reserve medical forces capable of parachuting themselves and their equipment to support a point of entry seizure.
The team exercised with the troops they would support on operations and hence developed Medical Standard Operating Procedures (MSOPs) designed to work within the constraints of a PBG. Given its high readiness, the PST was used for a number of short notice surgical deployments, including the military assistance mission to the Vanamo Tsunami in 1998, and in 1999 to Operation WARDEN where they provided the initial surgical support to peacemaking operations in East Timor.
Since that time, the forward surgical capability of the ADF has significantly degraded. There are now no integral, capable, forward deployable surgical teams with contemporary trauma or tactical expertise. ADF surgical teams deployed on operations since the early 2000s have been made up of medical personnel drawn from multiple different units (and in the case of reservists, with vastly different civilian practices) who may or may not have worked, trained or previously deployed together prior to the deployment. The actual civilian trauma experience of a significant proportion of reserve surgical specialists is unlikely to be equivalent to permanent work in a level 1 civilian trauma centre.
Surgical procedures on scene
Tactical combat casualty care (TCCC) elements of care under fire, tactical field care and casualty evacuation care have addressed the three main causes of preventable death on the battlefield (exsanguination from extremity haemorrhage primarily alleviated by the combat application tourniquet [CAT], tension pneumothorax and airway obstruction) and may be attended to by integral medics on scene, being within their current skillset (actually performed by all soldiers with initial training beginning at Kapooka). On the other hand, non-compressible truncal haemorrhage, which, by definition, is impossible to control with direct pressure, continues to account for almost half of otherwise potentially survivable deaths in recent MER conflicts.2 It is estimated from data held in the Joint Theatre Trauma System that as many as 25% of those who died in Iraq and Afghanistan 2001–2011 died of injuries that were potentially survivable if earlier access to surgical care had been achieved.3 The critical determinant of this potentiality is early access to surgical management. Rapid access of the injured to medical services remains a central tenet in trauma management.4
Thoraco-abdominal trauma
In terms of specific organ injury leading to non- compressible truncal haemorrhage, liver, spleen and small bowel mesentery account for most intraabdominal traumatic bleeding given their relative size, vascularity or predisposition to injury.5 Haemorrhage control for each of these organs in the first instance need not be overly complex nor time consuming. It has long been well established that complex resectional or restorative surgery is contraindicated in damage control surgery,6 and the life-saving manoeuvres associated with haemorrhage control and minimisation of gross intraabdominal contamination may be afforded with minimal equipment and time.
Abdominal packing immediately contains haemorrhage from many organs and is sufficient in the context of subsequent normalisation of physiology in a critical care environment to control up to two- thirds of otherwise exsanguinating haemorrhage from liver trauma, for example, at least in the blunt context seen in civilian trauma surgery.7 Adjunctive procedures may be necessary for those suffering penetrating injury. Nevertheless, temporisation can buy time for extraction and allow survival in patients who would otherwise bleed to death on the battlefield. Similarly, extraperitoneal packing following pelvic fractures may increase the likelihood of survival to higher-level care where external fixation or advanced procedures may be required.
Splenectomy for blunt or penetrating injury in trauma is usually expediently carried out within minutes with a single firing of a surgical stapler and may be performed with minimal lighting and exposure by surgeons experienced in the technique. Suture ligation is a cheaper but technically more challenging endeavour requiring better exposure and visibility. It would not be the preferred option in a genuinely austere and forward environment with potential close hostile activity. This intervention was only required once in the 15 years of after-action reports analysed by DuBose et al. (2020), among 87 procedures performed by a US Surgical Resuscitation Team (SRT).8
Suture ligation of mesenteric small bowel bleeding may be more easily afforded when necessary given its more accessible location in the abdominal cavity, but similar to liver trauma simple packing may be sufficient to allow extraction to higher-level care and more definitive haemorrhage control. Control of enteric contamination with stapled closure of small bowel defects is equally expedient requiring only one surgical instrument with the added advantage of being lightweight, disposable, prepackaged sterile and relatively cheap—that again being the ubiquitous surgical stapler (Figure 1). In the same series referred to in the previous paragraph, intestinal resection was undertaken in 8% of cases, representing a mid- range common emergency procedure performed by an SRT. If surgical staplers run low, enteric contamination can be controlled at the most basic level using umbilical tape to ligate injured bowel.

Figure 1: Disposable surgical stapler
In fact, abdominal packing, intestinal resection and splenectomy were the only abdominal procedures undertaken by a highly trained specialist SRT in the recent MER conflict validating the concept of abbreviated and simple-manoeuvre surgery that is possible far-forward.8
Life-saving intervention can therefore be afforded to many patients with non-compressible abdominal haemorrhage with only two surgical techniques— packing requiring only in the order of 10–30 disposable, lightweight, prepackaged sterile and extremely cheap surgical packs (Figure 2) and a surgical stapler with a variable number of staple reloads (recommended 10 as a minimum).

Figure 2: Abdominal packs
Temporary abdominal closure is the standard of care for damage control surgery even in fully equipped level 1 civilian trauma hospitals and is achieved using proprietary products such as the VAC system (KCI ™) but can be fashioned from surgical packs and drain tubes attached to suction canisters (Figure 3). Equipment required for formal VAC application includes a sheet of plastic, VAC foam, adhesive occlusive dressing and a VAC canister (Figure 4). This will allow transfer to higher-level care and ends the abbreviated laparotomy on scene.
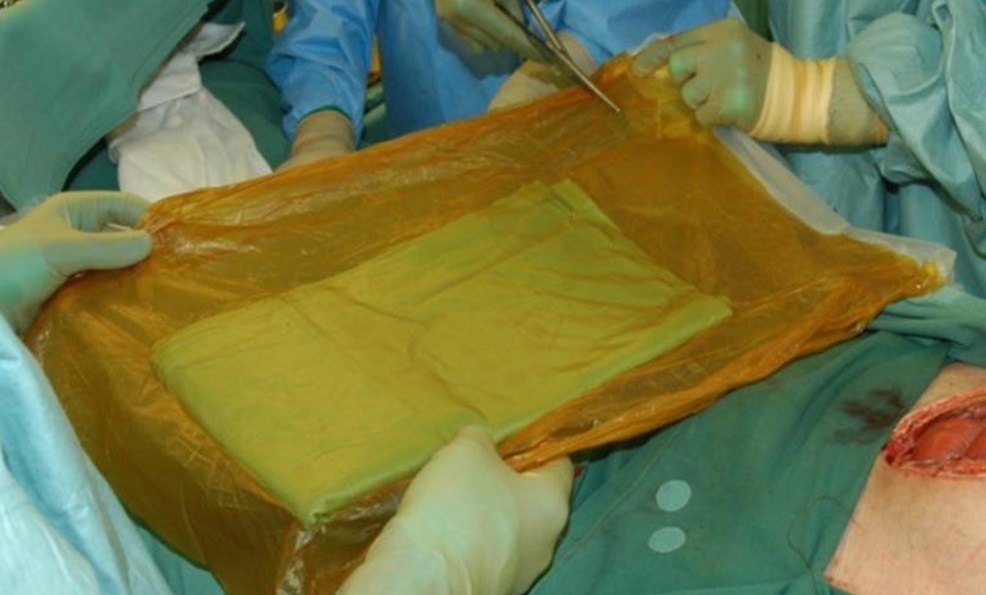
Figure 3: Make-shift ‘VAC equivalent’ for temporary abdominal closure (using ioban™ sandwiching a ‘huck’ towel)

Figure 4: Formal VAC system for temporary abdominal closure (Abthera™)
Other surgical equipment to allow these abdominal procedures on the field under the most hostile and constrained conditions include scalpel, disposable wound retractor (for example, the Alexis system that is disposable, lightweight, robust and effective— Figure 5), scissors, needle holder and suture material.

Figure 5: Alexis ™ wound retractor system
It would generally not be recommended that any thoracic procedures be attempted in the field. The only thoracic procedure that could be entertained is resuscitative thoracotomy (RT) with a pericardial window to relieve cardiac tamponade. However, cardiac repair in an austere environment would be considered extremely unlikely to be efficacious, although would no doubt be attempted in extremis. Thoracic aortic cross clamping is associated with minimal survival even in civilian trauma centres highly skilled in the application and utility with reported survival 9.7%.9 These procedures have been rarely reported in a military setting, and pericardial window at RT was only undertaken once in 15 years. Only seven RT were attempted (with overall mortality of 43%), reflecting the rarity with which this procedure would be considered.8 Theoretically, stapled lobectomy of bleeding lung is possible at thoracotomy and should not be contraindicated (especially as it requires no additional equipment other than the Finochetto retractor necessary for thoracic access).
Cross clamping the abdominal aorta at laparotomy is equally likely futile in the extreme forward environment. The procedure is not overly simple but ultimately only requires a single piece of equipment that can be carried prepackaged sterile as an aortic clamp (Figure 6). As a last-ditch attempt to save life, this would not be completely unreasonable, but it is foreseeable that most of these patients requiring this extreme level of intervention to save a life would likely succumb to injuries before arriving at a level of care capable of attending to that injury. An isolated major vascular injury to one of the great arterial vessels below the diaphragm (zone 2 or 3 aorta, common iliac, external/internal iliac or proximal femoral) by a single round may be the exceptional case that may survive, and so the inclusion of an aortic clamp with the carried set could be considered.

Figure 6: Aortic cross clamp
Wound infection is likely to be the least of these patients concerns, however, an attempt at sterility with some form of surgical prep (non-alcoholic to avoid flammability) and single window drape (with preformed central square cut-out, Figure 7) would at least minimise gross environmental soiling and trauma shears to rapidly cut through combat fatigues should also form part of the basic deployed kit. Lastly, individual surgeon headlights (with consideration of tactical green light filter) would be on the list of desirable equipment.

Figure 7: Disposable surgical square drape
Extremity trauma
Thankfully, given the widespread adoption of the CAT tourniquet, extremity trauma is rarely life- threatening in the field from the perspective of exsanguination. Damage control orthopaedics includes wound debridement and external fixation. However, it is unlikely this will ever need to be taken forward beyond its currently established function in the Role 2E facility, although debridement of gross contamination of limbs should be provided following blast injuries if evacuation time is prolonged (beyond 24 hours). Fasciotomy may equally be necessary if extraction is likely to be delayed. This can be performed by appropriately trained general surgeons with a knife and scissors and should be included in the prerequisite skillset of a forward trained surgeon. Equally, limb-saving is the ability to perform arterial shunting; however, the surgical complexity, exposure and training required to acceptably perform this type of procedure in the far-forward environment limits its applicability. Nevertheless, arterial shunting accounted for almost 14% of surgical interventions performed in the 2004–2019 cohort, although it is unclear under exactly how much austerity these procedures were undertaken.8 Attention to pelvic fracture with pelvic binder application supplemented with pelvic extraperitoneal packing on scene is preferred over external fixation that requires additional equipment and expertise.
Neurotrauma
While theoretically life-saving, craniotomy for military neurotrauma required in the field is rare and reported only once in the series by DuBose.8 This should not be seen as a priority skill given its rarity and unfamiliarity to most general trauma surgeons. The additional load required to effect this intervention coupled with its rarity also argue against including it as a key skill.
Capacity and load list
A small footprint surgical element capable of movement is essential to insertion and extraction inside the battlefield, which must intrinsically be able to move within very short time frames to deliver a meaningful health effect. Additionally, limiting surgical equipment to a load list that can allow transportation carried in backpacks is essential.
Dangelo et al. report their experience of an Expeditionary Resuscitation Surgical Team (ERST) comprising eight personnel (general surgeon, orthopaedic surgeon, critical care physician, emergency department [ED] physician, ED nurse, ICU nurse, surgical technologist, nurse anaesthetist). This team generally works more proximal than a far-forward team and carries supplies to perform
10 major surgical cases (thoracic, abdominal or neurological) with commensurate surgical sets including retractors, drills, vascular clamps, etc. to achieve those effects. The equipment is transported in hard cases; however, it is packageable to be carried forward with three soft bags per team member as necessary (two shoulder packs and a personal 36- hour bag).10
The far-forward surgical team proposed in this discussion paper would be envisaged to compromise half the number of personnel as the described full- scale ERST, being general surgeon, orthopaedic surgeon, anaesthetist, ED physician and nurse, and be equipped to provide a single major procedure to maximise efficiency, mobility and insertion capability. Prioritising only the highest value surgical procedures outlined above while minimising ancillary equipment should allow this small team to carry the required load while maintaining tactical manoeuvrability. The practicality afforded by two surgeons on either side of the operating table in terms of access and expert assistance and a depth of experience in the event of practitioner injury warrants this setup. Equally, two critical care specialists are of benefit in attending to the resuscitation effort concurrently.
In order for such a small team to perform the functions normally performed by a team of 20 to 30 requires individual and team skills and training. Each individual should be selected for predetermined attributes that allow them to function in a small group, and then the team should be trained in SOPs.
In fact, the surgical element of the ERST has a similar constitution comprising five members (general and orthopaedic surgeon, ED physician, nurse anaesthetist and either a second nurse or surgical assistant) and, when deployed forward, was shown to be able to reduce time to surgery by 6 hours. The ERST in this constitution could deliver one major surgical intervention and one minor surgical intervention with their deployed load.10 The four-member SRT described by DuBose, whose primary role was to provide damage control resuscitation (DCR) and surgery as close to the point of injury as tactically feasible and facilitate transfer to definitive care, comprised surgeon, ED physician, nurse anaesthetist and physician assistant and was equally streamlined.8
It appears between four and six staff achieves the optimal balance between capability and manoeuvrability. A structure of this nature aligns with the central elements of the JP2060 future health clinical care component of the next generation Deployable Health Capability for the Joint Force as it is modular, scalable and flexible and will strengthen the ADF trauma health response. Additionally, with sufficient all corps ‘good solider’ training in basic military manoeuvre, a surgical element of this nature could be constituted from the three services enhancing interoperability.
Anaesthetic considerations
The principal concerns of the anaesthesia provider in the forward, austere, remote or non-permissive environment are the safe conduct of limited DCR; the administration and maintenance of anaesthesia using minimal equipment and drugs; the preparation for early rearward evacuation, while simultaneously anticipating the need to perform extended field care when necessary. In many ways, the forward military anaesthetist has much more in common with colleagues in relief organisations such as Médecins Sans Frontieres (MSF) and the International Committee of the Red Cross (ICRC), than from military peers in a Role 3 or 4 facility.
The timely delivery of DCR in the austere environment relies on the expert adaptation of advanced skills obtained from regular, contemporary management of the severely injured in permissive, well- resourced trauma centres. The forward and austere environments are clinically unforgiving. To give the severely wounded or injured casualty the best chance of meaningful survival, initial resuscitation and administration of anaesthesia must set in place the preconditions for future success. No relative denial of upstream care can be mitigated downstream.
This requires advanced airway and major vascular access skills, experience in massive transfusion practices and contemporary experience in trauma anaesthesia. The key to success in the unsupported environment being discussed in this paper is the ability and comfort of the anaesthesia provider to adapt their expertise to the limited resources that are inevitable (indeed essential) to maintain a light footprint and forward mobility.
The reality is that the essentials of high-quality resuscitative anaesthesia can be performed using the basic equipment supplied with a resuscitation team. This includes a transport monitor, transport ventilator, transfusion equipment, fluid warmers and syringe drivers. The most common anaesthetic technique used by such teams over the past decade has been Total Intravenous Anaesthesia (TIVA) with ketamine as the dominant hypnotic agent, and usually in some combination with a benzodiazepine and opiate. Muscle relaxation and mechanical ventilation are, of course, ideal for surgery in major cavities and bring with them some reliance on supplemental oxygenation (or oxygen concentration). This has logistical as well as physiological benefits. Physiologically, of the TIVA techniques, ketamine based TIVA is the most haemodynamically stable— although ketamine remains a myocardial depressant in the shocked patient. Logistically TIVA equipment is lightweight (compared to anaesthesia machines) and ubiquitous in the military supply chain (as well as low-middle income countries where unconventional forces may operate). Unlike volatile anaesthesia, ketamine can be delivered in a closed space such as an aircraft or small unventilated room without the issues of off-gassing of anaesthetic agents.
While much can be achieved with simple equipment, some consideration must be given to the robustness and field utility of selected items. Ideally, all powered equipment should have a simple battery backup (that is, a readily available commercial battery, rather than a proprietary lithium rechargeable). Monitors and syringe drivers should be capable of functioning across a wide range of temperatures, and ventilators should ideally be turbine driven (so that they do not rely on pressurised gas supply to operate). Consideration may also need to be given to operating in low-light environments, or on the other hand, choosing equipment that is not clearly identifiable as military-spec if there is a requirement to support low-signature operations.
Ideally, the DCR team should be made up of a specialist anaesthetist, an emergency physician and up to two nursing or technical assistants with a background in emergency, critical care or prehospital practice. Such a team could comfortably and rapidly perform techniques to secure a casualty’s airway while simultaneously securing major intravenous access (such as via the subclavian vein to facilitate rapid flow rates) and then maintain anaesthesia, all while progressing ongoing haemostatic resuscitation.
Such a combination would allow the team to split into two to manage multiple casualties or perform forward or rearward extraction of casualties. Following successful haemorrhage control by surgical means, the anaesthetic focus would shift to critical care resuscitation until the casualty could be evacuated to a higher level of surgical care.
In addition to the usual litter horses used by a standard ADF resuscitation team, most small, austere surgical teams employ a surgical table that consists of a modular frame that a NATO litter can be strapped onto. The frame is designed so that it is structurally airworthy, with attachments for surgical lights, drip stands and shelves that a monitor can be strapped to. The frame has arm boards that allow the casualty to be positioned in the ‘crucifix position’ (the preferred position to resuscitate a severely injured person). This setup allows effective access to intravenous lines during damage control surgery and hard points that the team can strop themselves to continue to operate during flight. There are a number of companies that produce such a litter stand: The McVickers, the DOAK Mk 4 and the Charlie’s Horse SR901RT are all excellent off-the-shelf examples. All are ruggedised, lightweight, portable solutions that can be used either in an operating room as a surgical table or as the centrepiece of a resuscitation bay.
Post-operative patient evacuation
Given the introduction above regarding air superiority, ideally, any surgical team would be able to operate independently of any particular means of transport or platform (i.e. remain platform agnostic). With requisite training, having a broad range of options available would facilitate flexibility and interoperability. Utilising the ‘ruck, truck, house, plane’ approach to different modalities in prolonged field care, integration of surgical assets within this framework would allow planning for moving both the team forward and casualty rearward.
Depending on other assets already in the field and the tactical situation, there is an obvious benefit in basing the surgical team forward, even temporarily. Their augmentation in the provision of any tactical field care and preparation for evacuation care affords a greater level of support, especially if evacuation care were to be delayed as it often is.
However, if the surgical team were deployed on an on-call basis, arrangements could enable surgical treatment en route. It is worth noting that the British Medical Emergency Response Team (MERT) that operated in Afghanistan from a CH47 did not perform DCS, rather a highly advanced form of DCR in an air-superior environment with relatively short transportation timeframes.
If airframes are available within the risk profile of the mission, useful Australian Service helicopter options would include CH47 repurposed as a surgical platform (and which, once inserted, may stay on scene or move with medical intervention under way on board in flight). The use of the MI-8 or MI-17 or even the MRH 90 is also technically possible. Useful fixed-wing options include C27 or larger, fitted for surgical intervention.
Following surgery, the team would need to be able to hold a patient in place or evacuate rearward depending on tactical tempo. The usual expectation would be that any patient requiring DCS would not be woken from anaesthesia. Indeed they would require evacuation by critically care trained personnel to a more advanced level of care. En route, they would remain sedated, intubated and ventilated, provided ongoing resuscitation with blood products and attention to temperature control along with the usual aspects of critical care nursing and transport. Depending on the situation, this could be provided from within the team or handed off to another (e.g. RAAF CCATT).
Limitations
The major factor limiting the movement of surgical assets forward remains integral security, followed closely by recruiting, selecting, training and maintaining personnel with the genuine clinical expertise required for this type of work. If surgical teams are pushed forward, they are expected to act more like line units, requiring resources and tactical training. In addition, if the surgical team is busy performing surgical resuscitation, the members concentration and bandwidth will be consumed with the patient they are looking after, meaning that their situational awareness of what is occurring outside of the resuscitation will be compromised. This will require a tactical protection team of 4 personnel to provide close overwatch of the surgical team.
Inserting a surgical element cannot become a liability to the receiving unit. Although once an actual surgical procedure is commenced, there is no capacity for operating surgeons or anaesthetists to engage in tactical manoeuvres, up to and after that point, far-forward surgical teams must at least be able to engage in defensive movement for self-protection effectively. While remaining non-combatants, to afford a level of self-defence, the ability to fire and move safely in accordance with the current Combat Marksmanship Continuum would be considered essential. Limiting surgical intervention to rapid, easy to execute techniques facilitates this process. Casualty movement following operative intervention also needs to be taken into account, especially from an ongoing anaesthetic perspective. Surgical team members will require training in tactically moving, shooting and communicating in order to improve their survivability within a tactical environment.
Previous reports of deployed ERST members active in the MER confirm that while proficient with individual weapons, members could not provide their own security.10 Whereas Patel et al. notes there were numerous times the FST was responsible for its own protection without added security and recommended medical personnel attached to FST be further trained in combat skills, including management of prisoners of war.11
The requirement of basic Rifle Fire training completion is insufficient as a minimum to deploy as a far- forward surgical team. This is especially pertinent in the Australian context, where virtually the entire specialist medical capability provide reserve service, rather than regular Army employment. In the US context, the days when medical personnel were located in the rear are over,11 and to integrate with our coalition partners, it is recommended the ADF consider the readiness to again deploy a far-forward surgical team.
Instituting change
To institute meaningful change in healthcare delivery in the context of trauma, command interest from non-medical units is required. The introduction of TCCC is exemplary in this regard. Medical training was a highlighted area of command interest by the then commander of the 75th Ranger Regiment, Stanley McChrystal.1 Ultimately, this has resulted in the widespread adoption of the paradigm among armed forces and improvements in casualty care overall across militaries and nations. Engagement of senior commanders and tactical leaders is necessary to entrench medical outcomes as mission critical objectives. The delivery of effective forward surgical care mitigates not only adverse outcomes for the patient but also the mission more broadly. When a casualty occurs on a mission, the event is a tactical problem to be solved and not just an isolated medical issue.1
Summary
Once a patient arrives at a Role 2E facility in the MER, trauma care has been of exceptional quality. However, there will be only incremental gains if attention is focused on outcomes at this level. As approximately 90% of battlefield deaths occur prior to a casualty reaching a medical treatment facility, attention needs to switch to enhancing prehospital care to improve survival from combat injury.1 One method to achieve this is to take the surgical team to the patient, and this has been shown to reduce time to surgery by 6 hours.10
Damage control surgery is the gold standard civilian and military standard of care for severely injured victims of trauma. The central tenets of abbreviated laparotomy with temporary abdominal closure can be provided in an extreme abbreviated form, temporising injured soldiers at the scene with minimal surgical equipment and highly targeted manoeuvres aimed at stemming or controlling non- compressible truncal haemorrhage. In this ultra- abbreviated form, evacuation is still required, but it does buy time to allow casualties who would otherwise have died on the battlefield to reach higher-level care. In many ways, this represents the thoracoabdominal equivalent of the CAT tourniquet, which has revolutionised military medicine and fundamentally altered the causes of battlefield death. Surgical augmentation of Role 1 activities may again alter the distribution of battlefield deaths by minimising deaths from otherwise non-compressible truncal haemorrhage.
This requires an anaesthesia team capable and postured to provide rapid DCR within the resource constraints of the forward environment. These skills require the adaptation of expertise obtained through regular training and clinical experience in the management of the severely injured patient when not deployed. The forward trauma anaesthetist must be temperamentally suited to the austere environment. This is not a clinical environment flush with monitoring or specialised equipment, rather the survival of patients relies on the perfect application of paired-back clinical expertise and procedural skills.
Anticipating the movement of the equipped surgical team along with post-operative critical care patients will require careful consideration to be conducted safely and expeditiously. Ongoing development with trialling and exercising these elements will be essential in integrating this into mainstream practice.
A unique selection and training program must be developed to facilitate this process and equip existing trauma specialists with the necessary tactical skill set to provide effective care far forward in this austere environment. Leveraging existing civilian trauma- skilled medical staff should minimise the military trauma clinical upskill requirements.
Trauma care can be viewed as a niche capability in the broader context of health, but just as long- range reconnaissance or expeditionary offensive operations are only a fraction of Defence manoeuvre. Maintaining a highly specialised and well-trained group of a relatively small number of trauma specialists remains critical to support Army, Joint, combined or interagency operations more broadly. Noting the similarities in this regard with other special operations truths, it equally applies in health as it does in the special forces that quality is better than quantity; an effect cannot be mass produced, nor can it be created after an emergency has occurred; and finally, humans are more important than hardware. Investment in training highly skilled and agile operators postures Defence to rapidly adapt and evolve to future threats.
Development of a specific trauma-focused health capability to effect far-forward surgical care in this manner will be future-ready and independently deployable at short notice by leveraging the current extensive civilian trauma expertise present in various locations throughout the reserve forces. The training required to raise such an element requires tactical and operational upskilling more than clinical training if appropriate civilian trauma clinicians are identified and engaged. Defence must understand, appreciate and enhance the civilian skill set of its commissioned specialists in order to realise the full potential of those willing and able to serve and deliver a tailored combat health effect in the expert surgical management of trauma.
Corresponding Author: Charles H.C. Pilgrim, charlespilgrim@hotmail.com
Authors: C Pilgrim1,2, S Hendel3, N Eatough4, M Graves5
Author Affiliations:
1 The Alfred Hospital – Trauma Surgery Melbourne
2 Monash University – Department of Surgery, Central Clinical School
3 The Alfred Hospital – Department of Anaesthesiology and Perioperative Medicine
4 Royal North Shore Hospital – Emergency Department St Leonards
5 Wollongong Hospital – Anaesthesia Wollongong


