Abstract
Aims: In this study, we aimed to investigate the effect of depression on education regarding sexually transmitted diseases and reproductive and sexual health.
Methods: The study was conducted in 98 healthy private soldiers. Sociodemographic characteristics were recorded. The participants filled out the ‘reproductive health knowledge evaluation form’ (RHKEF) and Beck Depression Inventory (BDI) before the two-hour reproductive and sexual health education intervention. The RHKEF was repeated four weeks after the intervention. Higher than the median increase in the RHKEF score was accepted as a meaningful improvement. The effects of study variables and depression status on the RHKEF score change after the intervention was evaluated by using univariate and multivariate analyses.
Results: Among the study population, 35 soldiers (35.7%) were at risk of depression. The rate of depression was higher in soldiers who were living in urban areas compared with those living in rural areas. The mean RHKEF score increased from 16.9±3 at the baseline visit to 18.7±2.2 after the education. There was no association between the change in RHKEF score and depression or sociodemographic characteristics. There was a negative correlation between the age and change in the RHKEF score (r=-0.208, p=0.04) in univariate analysis. In the multivariate analysis, only the absence of depression had a positive effect on RHKEF score improvement. The OR was 2.08 (95% CI: 1.78-3.5, p=0.042).
Conclusions: The rate of depression risk is relatively high in healthy private soldiers. An education intervention for reproductive and sexual health seems to be beneficial in this population. Depression seems to influence the effects of education on reproductive and sexual health adversely.
Keywords: depression, education, military, sexually transmitted disease.
Introduction
Sexually transmitted diseases (STDs), generally acquired by sexual contact, have preventable causes and severe complications. Chlamydia trachomatis and Neisseria gonorrhoeae are the most common bacterial STDs in Turkey and worldwide.1, 2 Young adults are at higher risk of STDs.3 The risk is even higher in the presence of certain factors such as unprotected sexual contact, multiple sexual partners, illicit drug use, being uncircumcised and overseas travel. Abstinence from unsafe sexual contact, encouragement of condom use, delaying the age of the first sexual contact, facilitation of treatment, education of people at risk, treatment of partners along with patients when needed and implementation of routine check-ups are essential in the prevention and reduction of STDs.4
Among young adults, military recruits are in an age group with high levels of sexual activity. The peak age of STD transmission is between 20 and 24 years. In Turkey, military service is mandatory for every 20-year-old male Turkish citizen, and the duration may be one, six or 12 months according to education and health status.5,6 Besides being away from their family, social and workplace environments, the soldiers need to get used to a new place and being on duty both physically and psychologically. Furthermore, they face many challenges, such as a restricted personal life, lack of sexual relationships, living in a crowded environment, poor hygiene and harsh weather conditions.7 Such conditions may lead to psychological problems in soldiers with several studies indicating that psychological problems are associated with military attrition among soldiers.8,9
Depression may influence information processing, reduce the motivation for behaviour change and undermine sustained change.10,11 Depressive symptoms commonly develop along with the onset of STDs. Depression is also associated with low condom use rates, casual relationships, multiple sexual partners, sexual intercourse with sex workers and sexual intercourse while under the influence of illicit drugs.12-14 Several studies suggest that depression may diminish the benefits and efficacy of treatment of STDs.15-17 Untreated depression may also hinder interventions that aim to reduce high-risk sexual activity.
Because soldiers may encounter conditions that have a high risk for STDs, raising awareness of this issue is essential. Condom use is a cheap and effective measure to prevent STDs. As well as the social benefits, lecturing on this subject to military populations would be beneficial not only for the military service period but also for the rest of their lives.18 The beneficial effects of reproductive and sexual health education on the knowledge level of soldiers was shown previously.19
In the present study, we aimed to investigate the effect of depression scores on the success of education about reproductive and sexual health, and STDs in soldiers.
Methods
The present semi-experimental study was carried out in a military troop between October 2018 and November 2018, after obtaining the required permission from Erzurum Garrison Command. The study population consisted of 98 healthy private Turkish soldiers between the ages of 21 and 26.Military officers (12 soldiers) and those who did not want to participate (14 soldiers) were excluded from the study. The participants had to attend all education sessions to be included in the study. All soldiers who consented to participate in the study filled out the ‘reproductive health knowledge evaluation form (RHKEF)’ and ‘Beck Depression Inventory (BDI)’ before the education intervention. Subsequently, the reproductive and sexual health education, which lasted around two hours, was provided by two physicians (one of whom is a public health specialist) and a nurse (doctorate in public health).The RHKEF was repeated four weeks after the education.
The questionnaires in the present study were as follows; six-item ‘participant demographic information form’, a 25 item RHKEF and a 21 item BDI.
Reproductive health knowledge evaluation form: The authors prepared a 25 item ‘true or false’ questionnaire according to the literature in order to assess the knowledge level of the participants regarding reproductive and sexual health.
Beck Depression Inventory: The self-administered questionnaire and the Turkish validity and reliability study of the test was performed by Hisli et al.20 Each response to the 21 questions is scored between 0–3 points to determine the level of depression. A total score of 1–10, 11–16, 17–20, 21–30, 31–40 and 41–63 indicate regular ups and downs, mild mood disturbance, borderline clinical depression, moderate depression, severe depression and extreme depression, respectively.
Ethical aspects: The required ethical committee approval (date: 21 May 2018; approval number: 37732058-514.10) and permission from the relevant institutions were obtained.
Statistical analysis: Analysis of the data was performed using SPSS version 15.0 (SPSS Inc., Chicago, IL, USA).Histogram graphics and Shapiro Wilk test evaluated the normal distribution of the data. Categorical variables were compared by using Pearson chi-square and Fisher’s exact tests. Mann- Whitney U and Kruskal Wallis tests compared the nonparametric data. The correlation between continuous variables was assessed using Spearman correlation tests. The median split method was used to determine the median change in the RHKEF score after the education. A meaningful change was defined as a higher increase than the median value in the RHKEF score. Multivariate binary logistic regression analysis was used to determine the factors that are independently associated with an increase in the RHKEF score. A two-sided p-value of <0.05 was used to define statistical significance.
Results
The study population consisted of 98 healthy private soldiers between the ages of 21 and 26. Among the participants, 72.4% lived in urban areas, 92.9% were single, 55.1% were high school graduates, 83.7% had a private room before the military service and 74.5% had a history of sexual activity. According to the BDI, 35 soldiers were at risk of depression. The rate of depression was significantly higher in soldiers living in urban areas compared with those living in rural areas (42.3% vs 18.5%, respectively; see Table 1).
Table1. The comparison of subjects with and without depression
| Depression | p | |||||
| Absent | Present | |||||
| n | (%) | n | (%) | |||
| Age(median-IQR) | 22 | (21-26) | 22 | (21-24) | 0.671a | |
| Living area | Urban | 41 | (57.7) | 30 | (42.3) | 0.028 b |
| Rural | 22 | (81.5) | 5 | (18.5) | ||
| Marital status | Single | 59 | (64.8) | 32 | (35.2) | 0.698 c |
| Married | 4 | (57.1) | 3 | (42.9) | ||
| Education status | Left primary school | 1 | (50) | 1 | (50) | 0.545 c |
| Primary school graduate | 15 | (68.2) | 7 | (31.8) | ||
| High school graduate | 32 | (59.3) | 22 | (40.7) | ||
| College/university graduate | 15 | (75) | 5 | (25) | ||
| Private room | Present | 55 | (67.1) | 27 | (32.9) | 0.192 b |
| Absent | 8 | (50) | 8 | (50) | ||
| History of sexual activity | Present | 48 | (65.8) | 25 | (34.2) | 0.604 b |
| Absent | 15 | (60) | 10 | (40) | ||
aMann Whitney U test, b Chi-square test, c Fisher’s exact test. Significant p values are presented with bold text
Table2. The univariate analyses for the association between the change in the RHKEF score and the socio-demographic characteristics
| The change in RHKEF score | p | ||||
| Median | IQR | ||||
| Living area | Urban | 1 | 0-3 | 0.171a | |
| Rural | 2 | 1-4 | |||
| Marital status | Single | 1 | 1-4 | 0.077 a | |
| Married | 0 | (-1)-2 | |||
| Education status | Left primary school | 0.5 | (-1)-2 | 0.150 b | |
| Primary school graduate | 2.5 | 1-4 | |||
| High school graduate | 1 | 0-4 | |||
| College/university graduate | 1 | 0-2.5 | |||
| Private room | Present | 1 | 1-3 | 0.409 a | |
| Absent | 15 | (-1)-3 | |||
| History of sexual activity | Present | 1 | 0-3 | 0.360 a | |
| Absent | 2 | 1-4 | |||
| Presence of depression | No | 2 | 1-4 | 0.146a | |
| Yes | 1 | (-1)-3 | |||
| Severity of depression | Moderate depression | 1.5 | (-0.5)-3 | 0.937 a | |
| Severe depression | 1 | (-1)-2.5 | |||
RHKEF: reproductive health knowledge evaluation form aMann Whitney U test, b Kruskal Wallistest. Significant p values are presented with bold text
Among the 35 soldiers who were at risk of depression, 16 had severe risk.There was no significant association between the severity of depression and the sociodemographic characteristics.
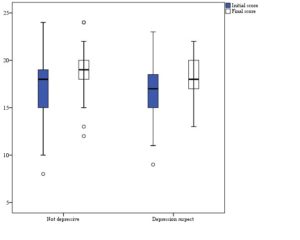
While the mean RHKEF score was 16.9±3 (median 17) at the baseline visit, it increased to 18.7±2.2 (median 19) after the education intervention.There was no association between the change in the RHKEF score and the presence of depression or sociodemographic characteristics.(see Table 2 and Figure 1).
The age of the soldiers had a moderate and positive correlation with the initial RHKEF score (r=0.345, p=0.001), a weak and positive correlation with the final RHKEF score (r=0.254, p=0.012), and a weak and negative correlation with the change in RHKEF score (r=-0.208, p=0.04; Figure 2).
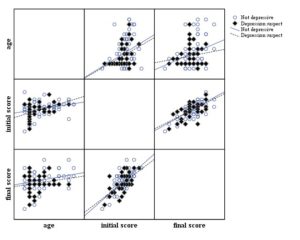
Figure 2. The correlation between the soldiers’ ages and their initial and final RHKEF scoresThe median change in the RHKEF score was 1 point.Among the study variables, only depression was independently associated with a meaningful change in the RHKEF score.According to the multivariate logistic regression analysis, the absence of depression increased the likelihood of an increase in the RHKEF score greater than 1 point by a factor of 2.08 (95% CI: 1.78–3.5, p=0.042; Table 3).
Table3. The multivariate analysis for the association of a meaningful change in the RHKEF score and the study variables
| p | OR | 95% CI | ||
| Lower | Upper | |||
| Age | 0.299 | 0.976 | 0.932 | 1.022 |
| Not depressive | 0.042 | 2.084 | 1.789 | 3.500 |
| Living in rural areas | 0.437 | 1.584 | 0.497 | 5.056 |
| Single | 0.16 | 3.116 | 0.431 | 22.548 |
| Does not have a private room | 0.539 | 1.464 | 0.434 | 4.936 |
| No history of sexual activity | 0.368 | 1.597 | 0.577 | 4.424 |
RHKEF: reproductive health knowledge evaluation form
Significant p values are presented with bold text.
Discussion
Nearly 40% of people seeking care at STD clinics experienced psychological problems immediately before or at the time of their visit.21,22 One of these studies reported that 14% of women and 23% of men experienced a major depressive disorder,22 which is a substantially higher rate than general practice patients and the US population.23,24 Several studies indicated that depression is an important risk factor for various diseases, including STDs.25–28 Depression may also adversely influence essential life functions, such as eating, drinking and learning.29, 30
Factors such as staying away from family, change of habits or change in the environment may accelerate depression.In the present study, among the variables, only the population density significantly affected depression.The rate of depression was higher in soldiers living in urban areas than those living in rural areas (42.3% vs 18.5%, respectively).This finding is consistent with previous studies.Urbanisation is not only a risk factor for cardiovascular disease and metabolic disorders such as diabetes mellitus but also mental diseases such as depression.31–33 In Turkey, a migration wave from rural to urban areas began in the second half of the 20th century.34 However, in our country, urban areas have become a risk factor in various aspects because of rapid urbanisation, inadequate infrastructure and adaptation problems.35 In the present study, we evaluated the association of depression with relevant factors (age, marital status, education status, etc.) reported in the literature, but there was no significant relationship found.
In contrast to previous studies,36,37 married soldiers had a higher risk of depression compared to single ones.However, previous studies focused mostly on the association between depression and marital status in women.38,39 Concerning age, Kessler et al.40 reported that while depression affected all age groups, the middle-aged individuals were at the highest risk level.The present study consisted of middle-aged individuals, but it did not include other age groups so we could not adequately assess the relationship between age and depression.
Although the increase in the RHKEF score was higher in the soldiers without depression than those with depression, the difference was not statistically significant (median value was 2 vs 1, respectively).In the multivariate regression analysis, depression was independently associated with the increase in the RHKEF score, and soldiers without depression were 2.08 times (95% CI: 1.78–3.5, p=0.042) more likely to benefit from reproductive and sexual health education. As mentioned in previous studies, depression may reduce the motivation to change behaviour, interfere with information processing or undermine sustained change.10,11 Furthermore, several studies suggest that depression may negate the benefits of intervention and inhibits efficacy.16,41 Holden et al.17 investigated the influence of depression on sexual risk reduction and STD infection with a cognitive/behavioural intervention (SAFE trial). Although the depressed women had a higher behavioural risk at baseline, the intervention was similarly successful in reducing reinfection and high-risk behaviour among depressed and non-depressed subjects.
A few limitations of the present study must be noted. First, the study utilised only subjective measures of depression at the individual level. In this context, further clinical evaluation is needed for an accurate diagnosis of depression. Another limitation is that such education interventions may not be sufficient enough when they are provided for subjects in a compulsory environment, as in the present study. Therefore, this may be reflected in the quiet small change in median RHKEF scores pre and post-intervention.
Conclusions
The lack of determination of the correct target group for reproductive and sexual health education may fail to obtain expected results from such interventions. The difficulty of succeeding in reproductive and sexual health education programs has been reported, but the studies were conducted on female populations alone.42–44 In this context, basic military training is a unique opportunity to perform such programs. However, depression may reduce the efficacy of this educational intervention.
Providing coordinated care can reduce the prevalence of STDs among soldiers with depression and be a crucial step in reducing the morbidity associated with poor mental health. The present study indicates an independent and adverse effect of depression on reproductive and sexual health education programs. Therefore, enhanced and coordinated health care for better mental health in primary care is vital for family planning and to prevent STDs.
Acknowledgments
Authorship contributions: Concept: M.Ö., R.Ö., A.B.; Design: M.Ö., H.Y.B.; Supervision: M.Ö., H.Y.B.; Resources: R.Ö., A.B.; Materials: R.Ö., A.B., H.Y.B.; Data collection and/or processing: M.Ö., H.Y.B.; Analysis and/or interpretation: M.Ö., H.Y.B.; Literature Search: M.Ö., R.Ö.İ H.Y.B., A.B.Writing: M.Ö., H.Y.B., A.B.; Critical review: H.Y.B.
Conflict of Interest
The authors declared they do not have anything to disclose regarding conflict of interest concerning this manuscript.
Corresponding Author: Özdemir Mikail, mika367@gmail.com
Authors: Özdemir Mikail1,2, YALÇINÖZ BAYSA Hasret3,4, Özkan Recep1,5 Baysal Abdullah1,5
Author Affiliations:
1 Ministry of Health of Turkey,
2 Osmaniye Tuberculosis Dispensary
3 Erzurum Ataturk University
4 Department of Public Health Nursing
5 Palandoken District Health Directorate


