ABSTRACT
TRAINING MILITARY PERSONNEL to manage military casualties is difficult. Within the Australian Defence Force (ADF), experience of major trauma is limited to those who work routinely in the emergency and trauma environments. Despite the increase in operational activity in recent times, the opportunities for medical teams to obtain sufficient and realistic experience remain limited. Traditional methods of training are perceived to lack realism whereas the full-scale simulated environment is recognised in other domains as enhancing the quality of training. This paper describes the training program aimed at improving the management of military casualties. During a two-year period, medical teams from the Australian Defence Force attended training sessions at the Sydney Medical Simulation Centre. They were required to manage a series of medical emergencies, which were video¬ taped. The recordings were used to facilitate a debriefing session at which human factors were highlighted as a component of integrated clinical management. Simulated training is an excellent way of improving knowledge, skills and behaviour. Personnel have identified the level of realism and the capacity to reproduce events in “real¬ time” to be a major factor in the value they attribute to this method of training. The incorporation of high fidelity simulators into team deployment training may prove to be a cost-effective method of improving the performance of medical teams on operations.
INTRODUCTION
TRAINING MILITARY PERSONNEL to manage military casu¬alties is difficult. Experience of major trauma is limited to those who work routinely in the emergency and trau¬ma environments. Even those who work routinely in such environments experience a civilian pattern of trau¬ma, which is different in significant ways from military trauma. For example, penetrating injury is relatively uncommon in the Australian civilian environment. Although there has been an increase in operational activity in recent times, the opportunities for medical teams to obtain the necessary experience remain limited. Traditionally, training has relied on methods of instruc¬tion that are perceived to lack realism. Lectures, skill stations and “moulaged” actors or manikins are not real enough. Strategies to place Australian Defence Force members in civilian trauma hospitals have been excel¬lent but may be limited by numbers, “hands-on experi¬ence”, doctrinal and lack of collective training issues.
In other domains, which include civil and military aviation, the full-scale simulated environment is recognised to enhance the quality of training. The simulated environment is well recognised beyond aviation and is now routinely used in the military environment to train on weapons and weapon systems, command and communication systems and in critical decision-making. Recognising the potential for the application of the simulation environment for medical training, the Sydney Medical Simulation Centre has developed expertise in
medical simulation.
In 1998, courses were developed for the Australian Defence Force as a collaborative project with Medical Officers of the Royal Australian Army Medical Corps. The ultimate aim of this method of training is to produce better-prepared medical teams and so reduce the “learning curve” effect that often blights the early stages of operational team deployment.
The smallest building block of health support within the Australian Defence Force is the resuscitation team. Each resuscitation team consists of a medical officer, a nursing officer, an advanced medical assistant, a medical scribe and an orderly. The role of the resuscitation team is to work together and manage effectively the resuscitation of military casualties, using methodology developed in advanced trauma life support to rapidly diagnose and treat life-threatening injuries. Onward transfer to a surgical facility for definitive treatment would then be considered after resuscitation and stabilisation of the casualty.
The critical point to be made is that teams and not individuals perform resuscitation of casualties. In order to work effectively as a team, each member must bring a minimum knowledge set, competence in certain skills and a role defined by a duty state¬ment. Understanding the importance of the team in the process of resuscitation, the Australian Defence Force has developed a doctrinal environment that encourages teamwork by standardised equipment, treatment protocols and policy directives.1.2 This allows interchange between teams, such as might occur on operational duty, secure in the knowledge that equip¬ment and protocols will be identical and new team members will be assuming corresponding roles.
TRADITIONAL TRAINING
A significant amount of instruction occurs in the class¬ room. Training on “part-task trainers” has been an essential part of this and skills such as intubation, cannulation and cardiopulmonary resuscitation are traditionally taught using such methods. Added to this are field exercises using surrogate patients and the contribution of this to team training is important. Casualties on such exercises are often “moulaged” and may carry cards describing the mechanism of injury, often with photographic representation of genuine injury. The progress of the casualty through the health facility will be controlled by directing staff who will advise the team of changes in the state of the casualty’s condition and efficacy of any treatment. Additionally, individual skills are often improved by means of College-accredited courses including the Field Nursing Course and the Early Management of Severe Trauma Course of the Royal Australian College of Surgeons. For others, the use of an attachment to civilian hospitals through a process known as a strategic alliance enables regular members of the Australian Defence Force to experience civilian trauma. At a medical assistant level, however, this can be limited by restrictions on direct patient care associated with registration and profession¬ al issues.
All the training detailed above allows the participants the opportunity to learn and practise skills before exposure to a military casualty. Unfortunately, the lack of realism associated with the traditional environment detracts from the overall learning experience. There is a gap between training and experience and this remains wide enough for those Australian Defence Force personnel undergoing such training to report that they do not get a “feel” for the specialty of military trauma.
Australian Defence Force teams need to sustain high levels of operational preparedness and capability. ADF Health Teams often have to deploy at short notice into situations where large numbers of casualties need to be treated. Such situations have included civilian aid to the victims of the Vanimo tidal wave or civilian casualties associated with peacekeeping operations, including East Timor.
Recognising this, medical officers of the Australian Defence Force approached the Medical Simulation Centre and the Department of Anaesthesia and Pain Management at the University of Sydney and, in collaboration, developed courses for military simulation aimed at providing an experiential training environment of simulated battlefield injury reproduced with a high degree of fidelity.
MILITARY SIMULATION METHODOLOGY
The Sydney Medical Simulation Centre
The Sydney Medical Simulation Centre is based at the Royal North Shore Hospital, St Leonards, New South Wales, Australia. The Simulation Centre opened in 1997 primarily to provide a simulated environment for anaesthesia training and subsequently has devel¬oped a number of courses in other fields, including trauma management. The Centre relies on an experi¬enced faculty working in major trauma centres with anaesthetic and surgical backgrounds in both the civilian and military fields.
Within the Centre is a simulation suite that uses an advanced simulator manikin of a type manufactured by MedSim-Eagle Simulation Inc., Fort Lauderdale, Florida. This “full patient, high-fidelity simulator” is an adult-sized manikin fitted with a variety of electromechanical and pneumatic devices and connected to a computer and a variety of sensors. Complex software programs enable the manikin to operate automatically by controlling the vital functions. Sophisticated mathematical modelling of the manikin’s physiological and pharmacological responses to physical interventions, or drug administration, allows integration with the control systems so that realistic responses can occur in “real-time”.
The manikin is constructed in such a way as to allow the full range of airway manipulations and instrumentation from basic head tilt and chin lift, through endotracheal intubation to the provision of a surgical airway. Chest trauma has been modelled to allow a variety of pathological states from simple pneumothoraces to cardiac tamponade to be simulated. The manikin can be cannulated and pulses can be palpated. The blood pressure is generated by the computer model and can be supplied to monitoring equipment when appropriate. Sensors monitor interventions such as oxygen therapy, ventilation and drug administration, and the appropriate physiological responses are programmed to occur realistically. The manikin can be spoken to and questioned relying on a member of the directing staff to provide the appropriate response using a microphone linked to a loudspeaker located by the head. Neurological signs and symptoms, including arm movement, maybe simulated and the manikin also exhibits pupillary reflexes.
Scenarios
Complex computer modelling, associated with high¬ fidelity representation of the response to medical intervention, allows elaborate injury scenarios to be developed (e.g. Table 1). Typically the scenarios are of the blast, penetrating or violent injury, such as might be encountered by a standard resuscitation team. Envenomation and myocardial ischaemia and other emergencies are also regularly modelled.
The scenarios can be tailored individually to allow specific training aims to be incorporated into cases. Teams using the Centre have included those from the Royal Australian Navy, who have simulated medical emergencies associated with diving and decompression illness, and joint Service teams who have been tasked with providing medical support with chemical, biological and radiological capabilities to security forces at the Sydney Olympics. The level of difficulty of each scenario can be modified to take into account differences in the requirements of various teams allowing an almost endless permutation of available scenarios.
The Process of Simulation
Over the last two years, more than 200 ADF personnel have been trained through the Centre, principally members of the Australian Army and Navy. Training has included the specific preparation of resuscitation teams for operational deployment overseas as well as the basic training of new teams and continuation training of experienced ones.
The process of training using the simulator is straightforward. Members usually train for a day or so in the unit environment, refreshing both individual and team skills prior to spending their time at the simulator. It is then usual for two teams from a unit to attend, alternating as either active participants or observers in a variety of resuscitation scenarios, usually numbering between four and six, during the course of a day.
The process of simulator training involves six stages:
- Orientation. Objectives for training are set along with an introduction to the Centre.
- Familiarisation. The students are introduced to the simulation manikin, learn about its characteris-tics and are given the opportunity to practice appropriate skills such as intubation and cannula¬tion prior to a full scenario-based simulation (This is an important step in diffusing anxiety and recog-nising the strengths and limitations of the simula¬tion environment).
- Simulation. Over a 20 minute period, full sce¬nario-based simulation occurs without interrup¬tion. The simulation is recorded on video and also broadcast in an adjacent viewing room where other members of the unit watch the resuscitation and prepare to participate in the debriefing.
- Debriefing. This takes about 30 minutes and is a peer discussion process facilitated by the senior medical officer of the unit concerned and an instructor from the Simulation Centre. During the debriefing, the video is used as a framework for discussion (All participants and observers get an opportunity to discuss a range of clinical and human factor issues).
- Conclusion. The process of reviewing the day’s events including a summary of lessons learned during the day.
- Feedback. All participants are asked to fill out an anonymous course appraisal questionnaire.
TABLE I: Example of Army Scenario Simulation “running sheet” – July 2000
| Summary: | Manikin | Mine Injury Soldier with multiple fragment injuries and traumatic amputation leg. Significant Hypovolaemia Hypoxia |
| Set-Up: | Moulaged multiple wounds to lower limbs, traumatic amputation leg, and abdomen punctures. Supplemental oxygen in situ Lying on-field stretcher with field medical report Spontaneous movements and painful stimuli Self-ventilating RR20 Sp02 85% on air Class 3 shock BP 100/60, P110 low volume Trigger hypovolaemic shock scenario. |
|
| Expected Responses: | Initial assessment Follows CTR Hypovolaemic shock and abdominal injury. Venous access and fluid resuscitation Nasogastic tube,DC and antibiotics. Consider airway control if unconscious. Assess priority and plan evacuation |
|
| Debriefing Points: | Early recognition of hypovolaemic shock. Prompt treatment of life-threatening conditions before completion of the initial assessment Haemorrhage control |
MEASURING THE EFFECTIVENESS OF SIMULATION TRAINING.
Methods
By means of a questionnaire, participants in military simulator training courses reviewed ranges of variables. These included factors that might affect individ¬ual performance, teaching style and instructor style and an overall self-assessment of performance in the simulator environment.
Results
For the purpose of assessing attitudes and value of training, the questionnaire was administered to 62-course participants. This included eight doctors, 10 Nursing officers and 44 Medical Assistants. Approximately one half were full-time members (30) and a similar proportion female (29).
Value as a training activity
In general, the activity was reported by participants as having high training value. Participants were asked to use a visual analogue scale to rate aspects of training in the simulator. One correlated with poor and five with excellent.
When asked to rate the overall value of the activity all rated the value as greater than four, with 58 (90.6%) rating the activity as five. In particular, the vast majority of activity subsets within the simulation scenario were rated by most participants as greater than four out of five on the VA scale (see Table 2).
Table 2: Value of Simulation as a Training Activity (n=64).
| Visual Analogue Response: | 1 | 2 | 3 | 4 | 5 | No Answer |
| Managing a Simulated Problem | 1 | 0 | 0 | 12 | 48 | 1 |
| Reviewing the Video | 0 | 1 | 0 | 11 | 47 | 3 |
| Discussing the Case with the Group | 0 | 0 | 1 | 16 | 43 | 2 |
| Receiving Feedback from Instructors | 2 | 0 | 0 | 10 | 49 | 1 |
| Overall | 0 | 1 | 1 | 11 | 47 | 2 |
Individual comments were sought as to the most useful and least useful aspects of the training. Thirty-five comments were entered (54.6%) with respect to most useful and five (7.8%) with respect to least useful. The comments were overwhelmingly positive, for example:
- “Equally useful to me as a non-medical person to a medical person in everyday life.”
- “Video debrief- good critical appraisal of scenario.”
- “The practical side of things in such a realistic situ¬ation. Feedback after scenarios. Familiarity and practice and to see other roles.”
- “The group discussion that focused on “the team” – usually discussion focused on medical officers only”
“Reflection, Team building.” - “Extremely useful.”
- “Feedback – know when you go wrong and how to fix it up. Using new equipment and knowing which bits work and which don’t.”
Effect of various simulation environment factors on performance
The simulation environment is highly realistic yet not real. The manikin, though high fidelity in terms of the software models that drive the simulated responses, has limitations. Subtle changes of physiological response such as colour change, sweating and capillary return (a measure of peripheral circulation) cannot yet be modelled. The simulation environment is potentially threatening. There is a testing and com¬petency element and individuals must perform with other team members in a scenario in which “the patient” may potentially die. About two-thirds of par¬ticipants (60.9-76.5%) found their performance improved by the factors of the simulation environ¬ment and only a small number (mean 2, 3.1%) found their performance degraded by these factors (Table 3).
Table 3: Effect of Simulation Factors on Performance (n=64)
| Visual Analogue Response | Degraded | Not Affected | Improved | No Answer |
|---|---|---|---|---|
| Patient Simulator | 4 | 9 | 49 | 0 |
| Operating Room Environment | 0 | 19 | 39 | 4 |
| Equipment | 2 | 17 | 41 | 2 |
| Scenario Design | 1 | 11 | 49 | 1 |
| Presence of Peers | 1 | 17 | 42 | 2 |
| Anticipation of Stressful Events | 4 | 15 | 40 | 3 |
DISCUSSION
Simulation training helps in the learning process. It enhances the acquisition of knowledge and skills by providing a realistic environment for training and it facilitates learning by setting it in a relevant clinical context (experiential learning).3
Training in a high-fidelity simulator helps learning at different levels. It can enhance the acquisition of knowledge and skills, reinforcing the importance of these by setting training in a realistic environment using scenario-based episodes of care to place such learning in a real-time relevant clinical context.
For the individual, patient error committed in the simulation environment is safer. Although a scenario may lead to death and the environment is perceived as real, the events are less traumatic than in a clinical situation. Shortly after the ending of the scenario, the recognition that such an event has occurred in a simulation environment rapidly becomes apparent. Though the environment is perceived as stressful, respondents in this survey did not significantly report degradation of behaviour by environmental factors. They individually and consistently reported simulation to have high value and the process of debriefing and video replay of critical events featured strongly in this. It is reasonable to infer from this that participants found the ability to become aware of error by this means to be an important reason for the value of the experience.
By basing training in the Sydney Medical Simulation Centre, expert opinions and advice can be readily available for training sessions so enabling the reinforcement of key points and the clarification of uncertain ones during the simulation process. The debriefing process has always included clinicians with high levels of appropriate experience including qualifi¬cations as EMST instructors and University appointments. Rather than using whatever becomes available in “real life”, simulation training can be planned in advance to include rare or difficult events6.¬ It has been shown that in anaesthesia some trainees have preferred training in the simulator to training in the operating or emergency room for these reasons.7 In the training with ADF, it is not possible to obtain real-life exposure to some injury. The successful modelling of chemical warfare agents and the effects of blast and fragmenta¬tion, both extremely rare in civilian experience, has shown simulation training to be the most realistic way of training ADF members to respond to these injuries.
Simulation training for resuscitation teams works in two ways. Individuals are able to obtain new knowledge and can experiment with “cause-and-effect” relationships observing realistic responses to treatments given or interventions performed. They can learn how to use new equipment or protocols and they can do so in stages or at their own pace. Team training is especially suited to the use of video debriefing.
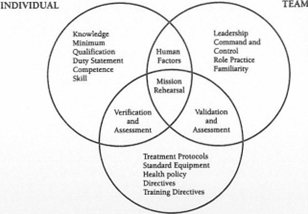
Resuscitation is a crisis event and memory of such events is often inaccurate8. Individual members of a team often perform in relative isolation and a video recording of the scenario provides an opportunity for all to observe their own work and that of others. Human factors become apparent during video debrief¬ing. Team function is a combination of individual and team skills (Figure 1).
Leadership, communication, situational awareness and resource utilisation are often issues that are not readily brought to mind when assessing performance, but aviation work showed how deficiencies in these areas could diminish team effectiveness. Observers can view the video recording and can assess clinical and behavioural skills, although it may be difficult to accurately correlate the performance in the simulator with that in ‘real-life’.
FIGURE 1: Simulation centres on mission rehearsal, a number of factors come into play.
HOW DOES SIMULATION WORK?
Experience with significant numbers of military teams being trained through the simulation centre has shown that time spent in the simulator is perceived as excellent training. In general, advanced patient simu¬lator training is highly rated, as is the teaching style, particularly in the use of video debriefing. 11.12 The sim¬ulated environment is felt to be challenging, realistic and practical and is beneficial with respect to aspects of teamwork in a way rarely seen in the peacetime environment. The environment is felt to be stressful because of the video scrutiny and personal perfor¬mance by many is felt to be sub-optimal presumably because of this factor. Others, however, felt that per¬formance was enhanced by the extra anxiety.
CONCLUSION
Medical Simulator training is an excellent way to improve knowledge, skills and attitudes. Personnel have
identified the level of realism, and the capacity to reproduce events in real-time, to be a major factor in the value they attribute to this method of training. This method of training is consistently rated very highly by the majority of participants and has thus been shown to be a very effective way of developing competence and capability in the building block of ADF Health opera¬tions: the resuscitation team. The incorporation of high¬ fidelity simulators into pre-deployment training may prove to be a cost-effective method of improving the performance of medical teams on operations.



