SIX AUSTRALIAN BATTALIONS have served in East Timor since the beginning of the International Force in East Timor (InterFET) and transition to the United Nations Transitional Administration in East Timor (UNTAET). Whilst many other Australian Defence Force (ADF) Units have also served with InterFET and UNTAET forces, this paper will be limited to discussing the comparison of malaria attacks rates between these six battalion groups to discern factors contributing to mitigation of malaria non-battle casualties.
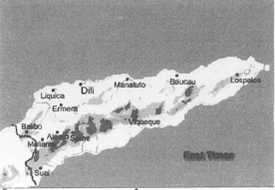
EAST TIMOR
The transmission of malaria is related to the geography and demography of East Timor. The wet season typically arrives in the last quarter of the calendar year and continues into the first quarter of the next year. The vector for malaria, the female Anopheles mosquito, steadily increases in number over the wet season due to the increased availability of breeding sites. The vector numbers peak several months after the beginning of the season. Transmission follows some months later as increased numbers of susceptible humans become infected.
The only reservoir for the malaria parasite is a human. Some humans, exposed to malaria for much of the year, maintain a degree of immunity that allows them to tolerate persistence of the parasite in their body without experiencing significant clinical symptoms. These semi-immune carriers of the parasite, as well as people acutely infected and ill with malaria, are reservoirs of the parasite.
The distance of an indigenous population, who carry the parasite, from ADF personnel is a risk factor as the flight range of the vector is generally no more than 1.5km. The vector also will not exist or fly higher than approximately 1500m above sea level, nor more than a few metres above ground level.
Initially, populations in the rural areas of East Timor were sparse. As stability improves in the UN territory, internally displaced persons are returning to their homes, which are now in close proximity to several ADF Units. Occasionally, ADF Units have been established adjacent to the path of transient populations.
As East Timor recovers from the infrastructure damage, improved drainage and water storage systems will reduce the number of breeding sites available for the vector. Simultaneously, the recovering health of the population and improved management of malaria cases at health clinics will reduce the size of the parasite reservoir.
PROTECTIVE MEASURES
Personal protective measures (PPM) include commitment to a ‘sleeves down’ policy, routinely sleeping under impregnated bed nets, regular application of mosquito repellent to exposed skin and pyrethrin dipping of uniforms and bed nets as well as adherence to anti-malarial medication (chemoprophylaxis). After the outbreak of malaria during InterFET, soldiers were likely to have became more aware of malaria and perhaps more compliant with PPM. It is not possible, however, to accurately comment on the comparative compliance with such measures. It is also salient to recognise that several Battalions had conducted exercises in malarious areas prior to deployment to InterFET or UNTAET and sustained malaria non-battle casualties from these exposures.
As well as environmental variables and proximity of malaria parasite reservoirs, battalions have varied in the range and nature of employed protective measures. Preventive Medicine (PM) assets, including personnel, equipment and consumable items were in short supply for the early forward Units in InterFET. Subsequent Units have deployed with larger and more robust integral PM assets under direct command. Later, health and entomological assessment and research teams from the Army Malaria Institute augmented PM assets.
BATTALION ANALYSIS
While a comparison of the malaria attack rates of each Battalion serving in East Timor may provide some information regarding prevention and management of malaria, any analysis or comparison of attack rates must be approached cautiously as many environmental, medical and operational variables are involved.
2 RAR
In September 1999, the Second Battalion, RAR, became the first ADF battalion to land in East Timor with InterFET. This Unit remained in the area of operations until mid-January 2000. As the wet season developed, 2RAR deployed out from Dili to part of the area now designated the Australian Battalion area of operations (AUSBATT). This area extends north from the central mountains of the territory along the border to the Savu Sea. Second Battalion included a resolute though small and lightly equipped PM element, which had difficulty obtaining equipment and supplies. Despite their best efforts, the first ADF malaria case in East Timor occurred in an outbreak striking 2RAR, following exposures in the Batugade area.
This was a particularly difficult location to hold, with an overwhelming vector problem and an enormous reservoir of parasites available in the transiting internally displaced persons returning from West Timor. The Battalion sustained 19 malaria cases during the four months of deployment in East Timor, an operation attack rate of approximately 3%.
Plate 1: 2RAR piquet over Butagade Beach, November 1999 – CAPT Bruce Russell identifying Anopheles mosquitoes centre-left.

3 RAR
The Third Battalion, 3RAR, deployed shortly after 2RAR into Dili, later onto the border on the Maliana Plain and then into the Enclave of East Timor.
The first malaria non-battle casualties from 3RAR were particularly severe with the clinical situation aggravated by the isolation for evacuation. The initial sub-units sustaining these non-battle casualties were experiencing overwhelming exposures to the malaria vector and parasite in the west of the Enclave around Citrana. In late 1999, this area was being rejuvenated both by returning waters into the river delta and returning villagers into the area, providing both vector and parasite. The Battalion headquarters and logistic elements were similarly exposed as the main city of Oecussi, situated on a flat, wet, coastal plain, rapidly increased in population.
Most of the Battalion redeployed to Australia in February 2000 after five months in the area of operations, having sustained 26 cases, an operation attack rate of approximately of 4%.
517 RAR
The Fifth/Seventh Battalion, RAR, maintained security in Dili early in the InterFET operation. The Battalion later extended operations and bases out to Liquicia and others areas around Dili. On a prolonged deployment, 5/7RAR then relieved 2RAR on the northern border in January 2000. The nature and location of operations of this Battalion potentially contributed to the fewer malaria non-battle casualties sustained; however, the duration of operations on the northern border areas is comparable to that of 2RAR.
Plate 2: Campsite of a JRAR patrol, Enclave of East Timor, November 1999 – two members of the patrol contracted falciparum malaria within two weeks.
Several significant factors of 5/7RAR mitigated vector-borne disease non-battle casualties. The integral mobility of many of the sub-Units of the Battalion allowed withdrawal from hazardous malaria exposure locations during high transmissions periods in the evenings. The Battalion made significant use of heavy engineering support particularly in the Batugade area to reduce vector-breeding sites. The Battalion deployed with a well-structured, equipped and supported PM team (lCSST), which undoubtedly benefited 5/7RAR in the prevention of vector-borne disease.
Subsequent Battalion Groups have had the advantage of the template provided by 5/7RAR (lCSSB) Group. Despite an extended deployment during a long wet season, the Battalion sustained only 13 malaria non battle casualties in East Timor, an operation attack rate of less than 2%.
6RAR
With the establishment of UNTAET, 6RAR relieved 5/7RAR in the northern border area. This Battalion was supported by elements from 7BDE including a significant PM team (7CSST). The Battalion also had the benefit of integral mobility and employed engineering support to further reduce malaria vector exposures. Initial assessments of a ‘dry season’ rotation perhaps reducing malaria exposure were reviewed as rates of malaria from (civilian) health clinics were found to peak after the midyear. Sixth Battalion were likely to have been exposed to the steady rise of parasite burden from increasing transmission occurring after vector breeding sites were established in the wet season and vector numbers increased.
While also using predominantly doxycycline for chemoprophylaxis, 6RAR sustained only seven non battle casual ties from malaria in East Timor, one of which was a reinfection giving an operation attack rate of less than 1%.
1 RAR
The First Battalion, RAR, relieved 6RAR into the second wet season of ADF involvement in East Timor. The Group was similarly equipped with a significant PM team augmented by elements of the Army Malaria Institute performing functions of a health and entomological assessment team as well as taking a field research role investigating alternative malaria chemoprophylaxis. The 1RAR Battalion Group sustained no malaria non-battle casualties in the area of operations.
4 RAR
The Fourth Battalion (Cdo), RAR, relieved 1 RAR in April 2001. The Group deployed with significant and experienced integral PM assets augmented by health and entomological assessment teams from AMI. The AMI team in collaboration with the medical elements of the Battalion Group also assessed the suitability of weekly malaria chemoprophylaxis using mefloquine (a registered antimalarial agent). Analysis of this assessment will be available shortly. The 4RAR(Cdo) Battalion Group sustained only one malaria non-battle casualty in the area of operations.
DISCUSSION
The AMI deployment to East Timor began with investigation of the malaria outbreak during InterFET. Since the outbreak, investigations have concentrated on recording the impact of malaria, antimalarial chemoprophylaxis, identifying and mapping the vector in the field, testing the acceptability of bed nets and repellents, and charting resistance to antimalarial drugs among the local malaria parasites. The vector for malaria is widely present in the AUSBATT and the local populations are effected by malaria seasonally, though to some extent all year. There is no evidence of resistance to doxycycline in East Timor, though the effectiveness of doxycycline was questioned. 1 This is consistent with the experience of other military operations2. Other military forces have found weekly malaria chemoprophylaxis regimens more suitable for operations3 ‘ and exercises in malarious areas’ and may have been the case during lnterFET for those peace keeping forces using weekly mefloquine6.
Table 1: (ADF) Malaria cases presenting in the East Timor area of operations
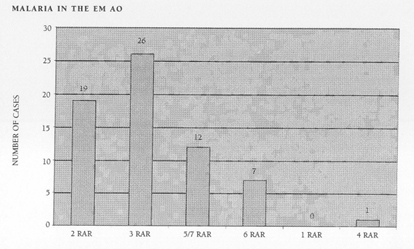
Initially, the operational attack rates for 2RAR and 3RAR were comparable to that recorded for Australian Forces in Vietnam prior to the introduction of effective malaria chemoprophylaxis with Dapsone in 19687. The subsequently developing pattern in preventative management of malaria at the Battalion level is quite evident with the evidence now available (Table l). The distinct reduction in operational malaria with the deployment of PM assets integral to 5/7RAR and sustained with 6RAR supports the value of these assets when well equipped, supported and commanded.
As East Timor re-establishes infrastructure, a reduction in breeding Sites for vectors and the human carriage of malaria parasites will reduce the malaria risk. Notwithstanding this potential reduction in malaria exposure, 4RAR Battalion Group, which earned comparable PM assets to that of the 6RAR Group, sustained only one malaria non-battle casualty during a deployment in similar seasons. 1RAR Group deployed with no malaria casualties. The apparent additional factors of weekly malaria chemoprophylaxis and the presence of an health and entomological assessment team augmenting PM assets has allowed the ADF to deploy a sizeable unit of professional educated soldiers into a highly malarious area on hazardous operations while sustaining minimal non- battle casualty from malaria.
CONCLUSION
Progressively, the integration of PM elements and health and entomological assessment teams has apparently reduced non-battle casualties sustained from malaria. Tailoring malaria chemoprophylaxis has contributed. The next challenge is prevention of post-deployment malaria non-battle casualties through further tailoring
of antimalarial agents for operations.



