ABSTRACT
Background: Scleroderma is a connective tissue disease, which has been associated with different occupational exposures.
Methods: We present a case report of a patient who developed localised scleroderma after occupational exposure to epoxy adhesives.
Results: Physical and histological examinations revealed presence of skin plaques, characteristic of morphea, in a disseminated pattern.
Conclusion: This case may reinforce previous reports that exposure to epoxy resins could provoke localised
scleroderma.
Keywords: Scleroderma; morphea; epoxy resins; occupational disease; adhesives.
INTRODUCTION
SCLERODERMA IS A GENERALISED DISORDER associated with inflammation and degeneration of connective tissues, culminating in intense and diffuse fibrosis. It is characterised by fibrosis of the skin, blood vessels, and visceral organs.
Morphea, also referred to as localised scleroderma, is characterised by erythematous or flesh-colored skin plaques, which become sclerotic and develop ring-like lesions with central hypopigmentation. In this article, we present a patient, who developed occupational morphea, and review the literature concerning occupational exposures associated with scleroderma.
CASE REPORT
A 40-year-old male, an Israeli Air Force (IAF) employee since 1974, had been working in a plastics department that dealt with the repair, maintenance and manufacture of aircraft and helicopter parts.
A detailed walkthrough of his workplace revealed various work processes and tasks. These processes involved cutting and polishing fibreglass-made parts, removal of paint coatings, cleaning of equipment, and application of a vast number of adhesives, most of them epoxy resin-based.
Throughout the years, he was exposed, on a small scale, to a vast number and range of chemical agents, such as silicon rubber, and organic solvents such as toluene, xylene, styrene, and methyl-ethyl-ketone (MEK). The main substances he worked with were fibreglass fibres, due to cutting and polishing aircraft parts, and epoxy resins, used as adhesives and sealing agents. The patient had no history of smoking, alcohol overuse, medication use, allergies or other special hobbies. He also had no history of occupational diseases.
For most of the years, he had been working without gloves, so that a significant skin exposure to epoxy resins probably existed all the time. In addition, he did not use a protection mask on a regular basis. The plastics department is situated in a natural ventilated room isolated from other departments.
The department consists of four workstations equipped with appropriate slotted side-draft hoods. For the last five years, his department has been environmentally monitoring by the IAF occupational health department. Environmental monitoring was commenced as a result of a detailed walkthrough.
Since 1997, 23 air samples for fibres and organics (fibreglass, toluene, styrene, MEK and xylene) have been collected during yearly environmental monitoring. Exposure of workers to these materials was estimated by collecting personal air samples from their breathing zones during working time. Personal samples were collected by a sampling tube, which was placed at a specific location near the worker’s neck. Personal sampling for toluene, styrene, MEK and xylene was performed by drawing air through a charcoal tube. The glass fibres where collected on mixed cellulose ester membrane. The sampling pumps (SKC-222, SKC Inc.) were calibrated by bubblier calibrator (Gilibrator, Gillian Inc.) and set at an airflow rate of 0.75 1/min. The air was drawn for at least 15 minutes. After sampling, each tube was closed with appropriate cover and placed in the refrigerator. The samples were analysed within two weeks using a high-pressure liquid chromatography (HPLC, Varian 5000) equipped with UV (ultraviolet)
365nm detector and column (Thermohypersil, inside diameter 4mm, reverse phase C8, 5mm, Length 15sm). The column temperature was kept at 28oC. The detector signal was integrated and the data were processed.
Environmental monitoring for styrene, toluene, MEK and xylene revealed Low exposure levels in most samples (Table 1). Levels exceeding the action level, and above the threshold limiting value-time weighted average (TLV-TWA®, ACGIH®) were found for styrene. As only one measurement of Toluene revealed very high exposure level, it was regarded as sample contamination (Table 1).
Biologic monitoring had been performed during all the years he has been working, including a medical examination; blood tests, including complete blood count, liver and kidney function tests; spirometry and chest radiography, without any pathological results. No toxicological tests were done due to the low levels found in the air. The 12-fold increased value for toluene in 1999 was assessed as a sample contamination in view of the very low measured values throughout all other years.
Two and a half years ago, he noticed the appearance of a rash on the posterolateral aspect of his right proximal forearm, 2.5cm in diameter, with a concomitant mild itching sensation. This was followed by other Lesions on both arms (Figures 1 and 2) and the further spreading of lesions to his abdomen, chest, shoulders and legs, although most of the lesions were confined to the forearms and chest.
| YEAR | MEK | TLV=200 Xylene ppm |
TLV=100 Toluene ppm |
TLV=50 Styrene ppm |
TLV=20 Fibreglass fiber/cm3 TLV=1 |
|---|---|---|---|---|---|
| ppm | |||||
| 1997 | 0.67 0.28 0.029 |
||||
| 1998 | 0.047 | 0.D1 0.008 |
0.17 0.026 |
0.28 | 0.04 0.01 0.16 |
| 1999 | 0.35 634# |
<0.01 | |||
| 2000 | 0.48 | ||||
| 2001 | 0.018 <0.025 |
<0.02 | |||
| 2002 | 7.97 | 1.04 | 15.52* | 0.46 |
Table 1: Environmental monitoring results in the Plastic department. (* levels exceeding Action level; # Level exceeding Threshold limiting values).
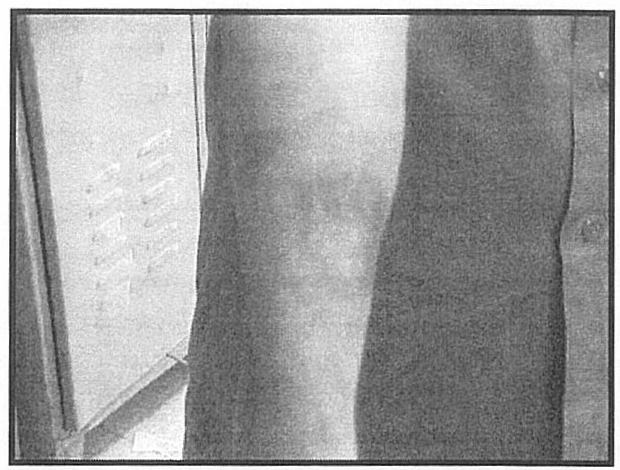
Figure 1. Forty-year-old worker, exposed to epoxy resins with a ring-like skin lesion with peripheral hyperpigmentation and central hypopigmentation on his right arm.
Dermatological examination revealed round hyperpigmented plaques, of 2-4 centimetres in diameter, with hypopigmented zones and atrophic skin (Figures 1 and 2). The patient denied any joint pains, digestive, or respiratory complaints. Physical examination was otherwise normal.
Biopsy of one lesion revealed dermis with almost complete absence of skin adnexae. Thickened and hyalinised collagen fibres were present within the fibrotic dermis. Focal vacuolar alteration at the dermo-epidermal junction were also present. These findings are consistent with morphea.
The patient was referred to the IAF occupational physician who recommended a change to his job. No medical treatment was provided, apart from periodic dermatological examinations. After one year of follow up, no new lesions were detected and no evidence of systemic involvement was found. No regression or progression of the lesions was noticed as well.
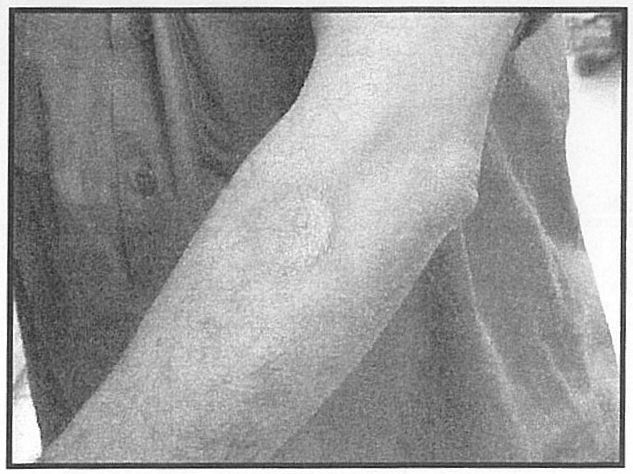
Figure 1. Ring like skin lesion with hyper and hypopigmentation and sclerotic changes.
DISCUSSION
We have presented a case of a worker engaged in manufacturing and repair of aircraft parts, associated with heavy skin exposure to epoxy resins, who developed generalised morphea, after 25 years of working with them.
Several reports describe an association between scleroderma and occupational exposure to silica dusty, vinyl chloride monomers’ and different solvents.6 There are few publications, however, linking occupational exposures to morphea specifically'<>”. Exposure to organic solvents, such as perchloroethylene (metal degreaser), trichloroethylene and tetrachloroethylene have been associated with morphea development’.,.”.
Only two patients, with a scleroderma-like disorder induced by epoxy resins, have been reported in the literature until now.13 Both patients were employed in a chemical factory where they were exposed to the polymerisation process of epoxy resins. Their clinical presentation included fatigue, burning and itching sensation of the skin, sclerotic changes of the skin over the entire body, hair loss, edema of the extremities, sclerodactyly and muscular weakness. No abnormal laboratory tests were detected. Electrocardiograph and chest radiographs were normal. Pulmonary function tests showed a slightly decreased vital capacity. Follow up at 17 years showed disappearance of their systemic manifestations. No internal organ involvement was detected during those years. 14
Histological examination revealed restoration of the normal pattern of collagen bundles, compared with previous skin biopsy specimens. These two cases, related to short exposure to epoxy resins, had an acute onset (about one month after starting work), without involvement of internal organs but with systemic signs and symptoms and with a fairly good prognosis.
The incubation time in other scleroderma-like disorders can be very long, ranging from 4 to 44 years . In our case, the patient presented a skin rash compatible with morphea, after 25 years of heavy exposure to epoxy resins, and without systemic involvement. The mechanism of morphea is probably immunological and not as a result of a primary irritant, so we can see the lesions distant to the primary contact area. Given the widespread use of epoxies, and the small number of reported cases of morphea related to epoxy resin exposure, the possibility of coincidence between cannot be excluded.
A casual association, between organic solvents such as toluene, xylene, styrene, or MEK, is possible. Yet, the use of organic solvents in this department was minimal (mainly for cleaning surfaces before repairing and maintenance procedures).
Significant exposure to fibreglass could exist in the process of cutting and polishing aircraft parts. Skin exposure may produce mechanical irritation, which results in severe skin itching, whereas allergic dermatitis is unlikely to be due to fibreglass.
Pinpoint excoriations are the principal clinical findings related to fibreglass exposure, although occasional inflamed papules may be present. In this case, however, the clinical features were totally different. Environmental monitoring of fibreglass did not reveal levels above the action level (Table 1). We also found no relation between morphea development and fibreglass exposure in the medical literature. In view of all these factors, a causal relation between fibreglass and morphea development is not expected. Interestingly, exposure to silica dust has been implicated in the induction of scleroderma.
We propose a contributory relation between the exposure to epoxy resins and the skin changes described. This was based on our observations, made on the walkthrough of the workplace, had revealed a heavy use of epoxy resin adhesives without any skin protection in our case study.


