By John Edward Cunningham SSE MB SS and Andrew M. Ellis MB BS FRACS
John Edward Cunningham BSc MB BS
Major, 1st Health Support Battalion
Orthopaedic Registrar, Mona Vale Hospital
Andrew M. Ellis MB BS FRACS
Major, 1st Health Support Battalion
Senior Lecturer, University of Sydney
Orthopaedic Surgeon, Royal North Shore Hospital
ABSTRACT
Fractures of the clavicle are very common and often effectively managed non-operatively, especially when they occur in the middle third. Mal-union is the expected outcome, which fortunately does not usually produce a significant functional limitation in the general population (1). In soldiers, however, there may exist a subgroup of the population in whom traditional non-operative management and results may impart a disability, which may then affect performance, and a subsequent downgrading of their PULHEEMS Employment Standard (PES). Given their requirement to carry heavy packs and webbing, and the physical demands of their profession, there has been discussion favouring the increased use of internal fixation.
This paper discusses the classification of clavicular fractures and their prognosis in the general population. The options of operative and non-operative methods of treatment are compared for each fracture type. Mid clavicular fractures, which are the most common in the general population, may benefit from open reduction and internal fixation (ORIF) in soldiers with a view to minimising the degree of malunion. The outcome of ORIF needs to be balanced nonetheless against the complication rate associated with operative intervention, so as to inform the reader of the balance of factors associated with such decision making.
KEYWORDS
Clavicle, fracture, clavicular, military, soldier, defence force, non-union, mal-union
INTRODUCTION
Fractures of the clavicle represent a common fracture in the general community, estimated to be involved in 5% to 12% of all adult fractures (1-4). There is currently no data collection on specific fractures in the Australian Defence Force (ADF), but there is no reason to suspect that it is any less common in this group.
It is important to appreciate the distinction between the subtypes of clavicular fractures, as each will behave differently, and have different implications on soldiers’ recoveries. Whilst malunion with good clinical function is usually the rule of a healing clavicular fracture, many will go onto non-union, or give a poor functional result despite healing within acceptable limits.
Soldiers, like elite athletes, may represent a unique subgroup of the population for whom even slight anatomical defects may become functionally significant (5). Any soldier that is required to carry a pack and webbing may become symptomatic of any mal-union if it produces a prominence under their straps. Other situations that may require consideration include those members who wear harnesses, being paratroopers, pilots and loadmasters. This paper will review the current literature on the management of clavicular fractures, their treatment in the wider community, and discuss various aspects of their treatment that may be relevant to the soldier.
EVALUATION
The clavicle is a bony structure linking the axial skeleton with the upper appendicular skeleton and is very close to vital neurovascular structures and the apices of the lungs. It contributes to about 30° of the range of motion of the shoulder girdle and is important for complete shoulder elevation (1).
Making the diagnosis of a fractured clavicle is usually quite straightforward, with pain and swelling in the region following mild to severe trauma. Stress fractures of the clavicle have also been reported in the literature, although they are exceedingly rare, and associated with sportsmen performing repetitive actions (6). The patient may hold the ipsilateral arm close to the trunk. Examination should include a complete neurovascular examination of the ipsilateral upper limb looking for brachial plexus or subclavian vessel injury, as well as a close examination of the skin overlying the fracture site. “Inside-out” compound fracture wounds may appear to be a simple graze after the skin flap has closed over, and bleeding ceased. An AP X-ray view of the clavicle is usually all that is required, but should include the sternoclavicular joint and the entire shoulder girdle to rule out other associated injuries. Stress radiographs may be required to evaluate distal third fractures and their ligamentous injuries, and oblique X-rays may be useful to confirm the diagnosis if in question. An estimation of the shortening of the clavicle, if any, and degree of comminution should also be made.
CLASSIFICATION
Clavicular fractures have traditionally been classified according to their position along the length of the clavicle, being in the proximal, middle and distal thirds (7, 8). It is reported that between 75 and 80% for all clavicular fractures occur in the middle third (8).
PROXIMAL THIRD FRACTURES
Fractures of proximal (medial) third of the clavicle are rare. There is a very strong ligamentous complex around the proximal end, so any displacement is usually minimal, and results with non-operative treatment can be considered to be good (1).
For completeness, it is worthy to note that dislocations of the sternoclavicular joint can occur. They are usually either external or internal, relative to the sternum. If external, they can usually be managed non-operatively, whilst internal dislocations should be regarded as an emergency, as they reduce the size of the thoracic outlet, and can compress vital structures (9, 10). In both cases, orthopaedic consultation should be sought.
DISTAL THIRD FRACTURES
Fractures of the clavicle near its distal end, comprising about 18% of all clavicular fractures, are sub-classified into three subtypes according to Neer (11). Type I fractures (Figure 1) occur without damage to the coracoclavicular ligaments, the fracture being located just distal to the ligamentous attachment. The intact ligament “holds down” the proximal end of the fracture in close apposition to the distal end, and so these fractures usually heal adequately without operative intervention (7, 11-13). However, in a long term follow-up study of non-operatively managed fractures of this type, 11% of patients reported persistent symptoms of pain, and 33% healed with some deformity owing to excessive callous. For a soldier carrying a pack, this may become problematic, with the straps of the pack rubbing against any lump. This may be an indication for a non-acute operation, to excise excess callous and/or bony prominence once the fracture is healed.
Figure 1: Type I Distal Clavicular Fracture
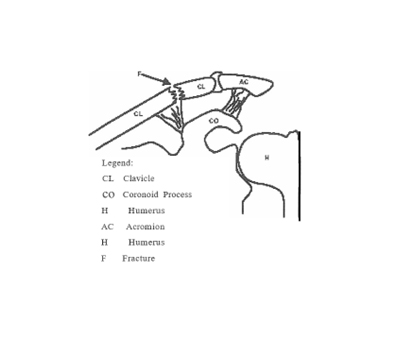
Type II fractures (Figure 2) occur just proximal to the coracoclavicular ligament, allowing the proximal end of the fracture is allowed to become elevated. It is therefore prone to non-union, with rates reported around 20 to 30 % (12, 14-17). For this reason, internal fixation is generally recommended even in the normal population (2). There is no reason to suspect that this indication would be any less relevant in the military setting.

Type III fractures of the distal clavicle (Figure 3) are intraarticular and involve the joint space of the acromioclavicular joint. In the past these have thought to be predisposed to developing a painful non-union (7, 11), yet in a recent small study, l4 patients with Type III fractures were managed conservatively and none of them displayed radiographic evidence of non-union (12). Resection of the lateral end of the clavicle, once an adequate period of time has passed with non-operative treatment, is an effective method of treating this complication should it occur (18).
MIDDLE THIRD FRACTURES
By far the majority of clavicular fractures, 70% to 80%, occur in the middle third (2, 19), and the treatment of these is probably the most controversial. Treated non-operatively, they are resistant to non union (between 0.8% and 5%) but mal-union is common (about 30%) in the adult population (3, 11, 20-24). In almost any other bone in the body, such results would suggest that open reduction and internal fixation (ORIF) would be the treatment of choice. The functional result in the general population however is very good despite these high rates (13,23), although the recovery may take some time (21).
If we take our example of the soldier, however, it may be proposed that any degree of mal-union or risk of non-union is unacceptable given their higher demands on their clavicles and shoulders. It is for this reason that we need to carefully examine our treatment regimes for these types of fractures.
The standard method of performing ORIF of a midshaft clavicle fracture is by the application of a plate and screws. It is not without risks, though. Interestingly, ORIF acutely increases the non-union rate, and is associated with a high rate of complications- between 12% and 20% of all ORIF’s of the clavicle will suffer at least one complication (25-27). These complications include infection, plate breakage, and of course, non-union, and all complications are increased in the non-compliant population, and in severely comminuted or shortened (>2.4cm) fractures (28-30). Indeed, studies of performing ORIF to acutely fractured clavicles report non-union rates of between 6% and 12%, and mal union rates of 12%, although these were on patients who had severely displaced fractures with comminution to begin with (25). We are left, then, with the quandary – damned if we do, and damned if we don’t (ORIF).
TABLE 1: Indications for ORIF of acute clavicular fractures
| Absolute | Compound fracture requiring debridement Association with neurovascular compromise |
| Relative | In the multi trauma patient in a “floating” shoulder |
There is little argument with regards to the accepted indications for ORIF of acutely fractured clavicles (Table 1) (7, 31). In the soldier, though we need to consider ways in which we can minimise the risk of non-union and mal-union to an acceptable level. Clearly, ORIF of these fractures is not a solution, as it actually increases the rate of non-union. Mal-union rates, however, are reduced with ORIF, and as this is an important consideration for a soldier, we may feel compelled to recommend acute ORIF, despite the high risks of the procedure (Table 2).
Table 2: Non-operative vs operative management complications of middle third clavicular fractures
Non-Operative ComplicationsOperative Complications
| Mal-union (30%) | Mal-union (12%) |
| Non-union (0.8-5%) | Non-union (6-12%) |
| Functionally poor result | Infection Neurovascular compromise Miscellaneous surgical complications Functionally poor result |
See text for references
Alternatively, we may look at maximising non operative treatment initially, and resorting to ORIF only after non-operative management has failed. Mal union and non-union of the clavicle can be well treated by osteotomy, bone grafting and internal fixation (28-30), although in the soldier the plates may need to be removed before they can return to full duties (5).
CONCLUSION
The modern soldier places enormous demands on his or her shoulders and clavicles, and a mal-united or non-united clavicula fracture can disable them considerably. One should therefore regard clavicular fractures in the military perhaps more seriously than amongst the general population. Operative management may be absolutely indicated in a setting of multiple trauma and neurovascular compromise and relative contraindications both strong and moderate are increasing as our knowledge of the demands placed on the upper limb in the soldier expand. Personnel who require optimal use of the upper limb may benefit from a procedure that restores the clavicle to length and maintains an anatomic reduction, provided that complications of non-union and delayed union are avoided. Fractures of the middle third of the clavicle are the most common, and subtleties of their treatment can be lost if practitioners follow a “recipe book” approach to their management. Accurate collection of data on the incidence and treatment of these fractures in the ADF should be a priority.



