Abstract
Disease has often determined the outcome of tropical military campaigns. This is especially true in Burma (Myanmar), where entire armies have been incapacitated by fever thought to be due to malaria during the Sino-Burmese Wars (1765–1769), the Anglo-Burmese Wars (especially the first in 1824–1826) and World War II (1942–1945) when the British 14th Army fought against the Imperial Japanese Army. The monsoon limits military activity logistically, but malaria following the rains still can incapacitate armies, particularly in forested areas favoured by the Anopheles vector. Strict discipline applied to imperfect chemoprophylaxis was successful in World War II and will be required in any future conflicts. Political instability in parts of Southeast Asia continues to make malaria a disease of abiding military medical interest and necessitates better forms of chemoprophylaxis.
Malaria determined military outcomes in Burma (Myanmar) across three centuries
Tropical Southeast Asia has repeatedly resisted invasions from Eurasian empires by wars of attrition fought over difficult terrain and complicated by infectious diseases that decimated foreign armies. Historically, it is difficult to know exactly what stopped the Mongol invasion of Vietnam’s Red River Valley in the 13th century; attributed to evil spirits, it seems likely that malaria was involved. The modern southern boundaries of China were determined both by geographic and disease limitations on invading armies. Three historical examples over the past three centuries stand out in terms of Burma (currently known as Myanmar) with Chinese invasions in the 18th century, British/Indian invasions of the 19th century and the Imperial Japanese Army’s invasion during World War II in the 20th century. In all three instances, febrile diseases known certainly to be malaria only in the last instance determined the ability of commanders to maintain deployed forces and thus largely determined military outcomes. As political instability continues to cloud the future of Burmese politics, it is worth reviewing the historical record to understand why military operations in Southeast Asia were constrained by malaria and why this threat remains for any complex public health emergency in tropical Asia.
Sino-Burmese Wars
He also decided to ignore the pleadings of his officers and began the campaign at the height of the rainy season… hoping that the ‘miasma would not be everywhere’.1
A series of unsuccessful Chinese invasions of Burmese territory occurred in 1765–1769 as the Qing dynasty pushed its influence southwards against the Burmese who were otherwise occupied against their traditional Siamese enemy. When Chinese forces (green standard or reserve army) were drawn into northern Burma (Bhamo), disease destroyed thousands of soldiers due to enteric and malarial causes. Reports were received that 800 of 1000 soldiers in a single garrison had died of disease.1 After two preliminary seasonal invasions using local forces from Yunnan failed to make an impression in the Shan Hills, Imperial prestige became involved, and a larger effort using Manchu bannermen (regular army) forces was planned (see Figure 1). Invasion of the central Irrawaddy Valley initially succeeded but pressure on the extended supply lines and increasing disease deaths stopped the offensive short of the capital of Ava.1 Only a few dozen survivors of the 10 000 strong force were stated to have made it back to China. The fourth and final attempt of this series in 1769 began during the rainy season in contravention to the Burmese military knowledge that this was not the time to launch military operations.1 A Burmese border fortress was remarkably stubborn, slowing the Chinese advance until both the soldiers and its commander were ill from fever. By the end of 1769, a peace treaty was negotiated in order to stabilise the border and permit the invaders to retreat back into China. The Sino-Burmese Wars are widely regarded as the greatest military frontier failures of the Qing, ultimately costing the lives of the four senior military commanders and 70 000 soldiers largely killed by disease.1

Figure 1: Mongol (Qing dynasty) troops of the Blue Banner in the Chinese Army during the 17th century, similar to those who participated in the Sino-Burmese Wars of 1765–1769. Painting dating to Emperor Qianlong’s reign. Considered in public domain as a historical object >200y old.
(Source: http:// chinese-armour.freewebspace.com/photo2.html)
Anglo-Burmese Wars
The detachment was immediately attacked with a malignant jungle fever peculiar to the country, which in a few days reduced it to about twenty men capable of doing duty.2
Conflict between the adjacent empires of the London- based East India Company that had displaced the Mogul rulers of India and the Burmese occurred over the border provinces of Manipur and Arakan in the early 19th century. By 1824, the British felt compelled to push the Burmese back along the frontier, and initial reverses eventually held to a sea-borne invasion of Rangoon by the Indian Army strengthened by a few British regiments. The Burmese forces retreated up the Irrawaddy river fortifications while the British/ Indian soldiers progressively became ill from enteric and malarial fevers. Eventually, superior British artillery (including rockets) killed many soldiers, including the Burmese commander, and a truce involving large financial repartitions was settled on the condition that the invaders leave Burma.1
Casualties largely due to disease were very high but variably calculated (see Figure 2). It was estimated that of the 40 000 British and Indian soldiers engaged, 15 000 (38%) died. Of the 3586 European soldiers who originally occupied Rangoon, 3115 died (86%), but only 150 of those deaths occurred in battle.3 The War Office in London stated that 5.25% of British soldiers commanded by General Campbell died in battle, but 67.5% (>1:12 ratio) died of disease during the two-year war.4,5 The Arakan invasion force (which never reached Rangoon) is thought to have experienced 44% casualties largely due to diseases among its European soldiers, while its Indian contingent had 57% casualties; their commander General Morrison died of disease while being evacuated to England.2
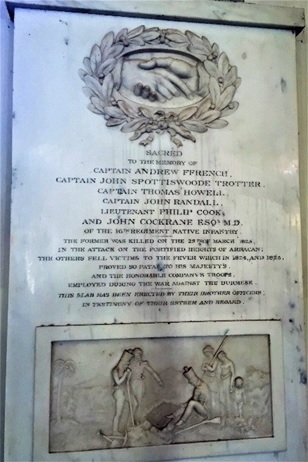
Figure 2: Memorial plaque in St George’s Cathedral Madras (Chennai) to six Indian Army (16th Native Infantry) officers who died (one in combat, five from disease, including a medical officer) during the First Anglo-Burmese War of 1824–1826.
(Source: Photographer WestCoastMusketeer under Creative Commons in Wikipedia 2016)
World War II
Good doctors are no use without good discipline. More than half the battle against disease is fought not by doctors, but by regimental officers. It is they who see that the daily dose of mepacrine … is taken…If mepacrine was not taken, I sacked the commander.
I only had to sack three; by then the rest had got my meaning. Field Marshall Sir William Slim6,7

Figure 3: Bronze statue in Whitehall, London of Field Marshall William Slim (later Viscount) commander of the British 14th Army in Burma during World War II 1942–1945.
(Source: Photographer Hydeblake in public domain from Wikipedia 2007)
After the fall of Singapore in 1942, the Imperial Japanese Army invaded Burma with four infantry divisions and rapidly sent two understrength Indian Army Divisions retreating into India through the highly malarious Assamese jungle. A sick, beaten army of stragglers eventually made it back into India just ahead of the monsoon rains of 1942.6 Malaria was a major factor in developing sufficient manpower to construct the British/Indian 14th Army into the eventual fighting force it became after its formation in 1943. After a failed Allied offensive in the Arakan in 1943, the entire Indian 6th Infantry Brigade was infected with malaria, and in the last three months of the offensive 18 000 soldiers with malaria were evacuated back to India.7 The Imperial Japanese Army then conducted an ill-advised and poorly- supplied offensive in 1944 to capture Imphal in India but was stopped by the stubborn defence of Kohima. The 14th Army counter-attacked and reached the Irrawaddy Valley after capturing Mandalay. In the reverse of 1942, the Allies chased the Japanese Army back down towards Rangoon, destroying isolated units as they tried to flee into Thailand during the monsoon. Burma was the greatest land-based defeat of the Imperial Japanese Army during all of World War II.
Malaria contributed greatly to the defeat of the Imperial Japanese Army in Burma just as its control gave the British/Indian 14th Army an important medical advantage against its enemy. LTGEN William Slim, whose quote begins this section, was convinced that malaria was largely a matter of military discipline once it was known that the imperfect, yellow-dye mepacrine (atabrine) would stop malaria if taken daily (see Figure 3). Disease casualties on both sides were high but can be estimated because by the 20th century malaria was known to be a parasitic disease spread by mosquitos that could be diagnosed by microscopic examination of the blood. In 1943 the 14th Army’s illness rate was an enormous 1200/1000 men with >5000 malaria cases per day at peak with malaria rates between 100–250/1000 men.8 Most hospitalisations were due to illness, of which malaria was clearly the chief cause especially given the propensity of Asian malaria to relapse. By 1945 the overall Allied hospitalisation rates of malaria were one-sixth (10/100 men) of peak levels with only six deaths from 14 000 cases.7 Japanese malaria casualties can only be estimated. However, essentially, all infantry soldiers in Burma developed malaria at some point in the campaign, which, even if it did not kill them, greatly reduced their combat effectiveness.
Discussion
Malaria retains its particular significance to military operations in Southeast Asia, even today, because it can rapidly increase from a very low baseline to infect and subsequently incapacitate most of a deployed force. For example, East Timor had a very small malaria problem in 1999 until it was massively disrupted by the Indonesian withdrawal that resulted in a malaria epidemic, infecting the Australian peacekeepers.9 Malaria is not restricted to military members but contributes to complex public health emergencies with massive refugee movements, such as the Vietnamese invasion of Cambodia in 1979.10 Although Southeast Asia has made great progress in some areas of malaria control, the disease is far from eliminated and its potential to disrupt military operations remains. Moreover, current political instability in Burma and uncertain Chinese intentions throughout the region only increase the potential of future emergencies in the area to have a malaria component. Chemoprophylaxis options have advanced considerably since World War II; however, LTGEN Slim’s emphasis on discipline enforced by unit officers as the key to making drugs an effective military malaria control measure remains true today.
Corresponding author: Dennis Shanks, Dennis.Shanks@defence.gov.au
Authors: D Shanks1,2
Author Affiliations:
1 ADF Malaria and Infectious Disease Institute
2 University of Queensland – School of Public Health






