T J Watt, E James Kehoe
Abstract
Arts-based activities are increasingly being offered to current and former military members as an adjunct to their established therapeutic interventions. Individuals who undertake arts-based activities have shown reductions in both anxiety and depressive symptoms. However, little is known about the specific mechanisms engaged by these activities or the duration of their positive effects. The current research aims to test changes in four mechanisms—specifically, behavioural activation, belonging, therapeutic alliance and flow states—that have been prominent contributors to success in established therapeutic interventions. The mechanisms plus changes in anxiety, depression and core self evaluations were assessed during a four-week art-based program for veterans that included visual, written, musical or theatrical streams in a nonclinical setting. Participants demonstrated increased positive changes in all four mechanisms and core self evaluations, which peaked at the end of the program. Conversely, anxiety and depressive symptoms reduced in a similar pattern. Over a six- month follow-up, the scores on all measures returned to levels similar to their baselines.
Introduction
Military service exposes members to various traumatic and non-traumatic stressors that create the potential for poor mental health.1 As adjuncts to established therapeutic interventions, there is increasing interest among therapists and veterans alike in the possible benefits of members’ pursuing arts-based activities alongside their main treatment.2 Such arts-based activities include visual, written, musical and theatrical modalities. In this context, the present paper describes a portion of the evaluation for a program of art-based activities aimed at supplementing the treatments of wounded, injured and ill military personnel. This program, badged as the Arts for Recovery, Resilience and Teamwork Skills (ARRTS) program, was initiated by the Australian Defence Force (ADF) in 2015.
Prior to the present study, the evaluation comprised 31 of the 119 participants who were contacted 18 months or more after completing the four-week ARRTS program through 2015, 2016 and mid-2017.3 These former participants responded on a retrospective basis to 16 statements concerning their experiences, for example, ‘I had a sense of achievement from the activities I undertook’. The participants were asked to tick a box as to whether the statement applied to them before, during, and/or after the program. In addition, there was a question asking the duration of the effect following the program. The respondents also completed a measure of psychological distress (K10) and a Core Self Evaluations Scale (CSES), both of which are described in greater detail in the method section. This retrospective survey revealed that the participants experienced ongoing benefit from the ARRTS program from 18 months up to 48 months later.3
As may be apparent, the previous survey was limited to a small number of former participants surveyed considerably after the program. The present study aimed to fill the gap in our knowledge regarding the participants’ experiences during the program and in an immediate follow-up period of six months. Whereas the retrospective study focused on categorical judgements concerning remembered experiences, the present study provided a more detailed longitudinal, quantitative assessment of the participants’ experiences. In addition, the study was based on a more substantial sample (final N = 92) recruited from five cohorts who completed the ARRTS program between late 2017 and late 2019.
Art and mental health
Art-based activities have demonstrably assisted veterans and civilians experiencing anxiety, depression and PTSD.2 Beyond remediation of mental health disorders, art-based activities have been associated with improved resilience, sense of belonging, quality of life, and reductions in stress, anger, physical complaints and social isolation.4 Specifically for veteran populations, art-based activities in the forms of visual, written expression and theatre have demonstrated mental health benefit.5
Despite these promising results, art-based activities have not been well standardised. Among other things, the activities have been conducted by specialised art-therapists and art educators, which was the case for the ARRTS program. So far as can be found, published literature on the use of art educators has been limited to children diagnosed with autism.6
The underlying mechanisms
The present study was conducted to identify specific mechanisms through which participants experience the benefits of art-based activities. In other types of psychological therapy, four mechanisms have been prominent contributors to therapeutic success. As will be detailed below, they are behavioural activation, belonging, therapeutic alliance and flow states.
Behavioural activation: Undertaking activities that provide a sense of purpose, achievement or enjoyment in a clinical context are broadly called ‘behavioural activation’.7 Active recreational pursuits (e.g., artistic activities, hobby crafts, and sport) and even passive enjoyments (e.g., watching a movie, relaxing in a bath) may achieve behavioural activation. Multiple clinical studies have demonstrated that behavioural activation may be described as ‘a low-intensity guided self-help’ treatment that improves depressive symptoms. Behavioural activation may also reduce anxiety symptoms, but empirical support for this proposition has been debated.8
Belongingness: A sense of belonging can improve mental health in a variety of settings. By the same token, a sense of belonging can lead people to become more resilient and less vulnerable to common mental health concerns.4 Being part of a group and the resulting processes were a mechanism by which visual art-based activities have achieved positive outcomes for veterans.2
Common Factors: There are four recognised categories of factors common to patient-therapist relationships.9 The largest category is the ‘working’ or ‘therapist alliance’,10 which is a combination of the bond, trust and vision shared by the therapist and patient. The other three categories are: client- specific factors, such as the patient’s engagement, motivation, openness to change and expectations about engaging in therapy; therapist-specific factors, including skill, training, and ability to interact with the patient; and finally, therapy-specific models and techniques, such as credibility, placebo effects, therapy structure and therapy focus.
Flow states. Flow states are commonly described as living in the present, including the ability to become fully immersed in an activity with energised focus and enjoyment, potentially losing the sense of space and time.11 Activities that produce a flow state may be connected to relief from debilitating anxiety. Along similar lines, the absorption in an activity can enhance satisfaction from an optimal challenge and increase belief in competence, thus influencing the enjoyment of activities.
Core self-evaluations: A higher-order personality trait comprised of locus of control, neuroticism, self- efficacy and self-esteem—called an individual’s core self-evaluations—has been proposed as influential for an individual’s effectiveness in the workplace.12 People who have high core self-evaluations will think positively of themselves and be confident in their own abilities. Conversely, people with low core self-evaluations will have a negative appraisal of themselves and will lack confidence. A person’s core self-evaluations are a predictor of job performance, job satisfaction and more effective goal setting. Beyond the workplace, a person’s core self- evaluations may contribute to their overall outlook and accordingly mental health.
Psychological distress: Psychological distress, a construct comprising of symptoms of anxiety and depression, is one of the regularly assessed mental health concerns within the ADF. Prevalence in any 12 months for these disorders is 9.5% for depressive disorders and 14.8% for anxiety disorders.1
Research questions
Based on the above considerations, the present study addressed the following questions concerning the participants’ experience during the ARRTS program and within a six-month follow-up period.
Do the participants experience changes in the underlying mechanisms of behavioural activation, belonging, common factors and flow states?
Do participants experience changes in anxiety and depressive symptoms?
Do the participants experience changes, if any, in trait-based characteristics as assessed by the CSES?
Method
Respondents: The respondents (N = 92) were recruited from five ARRTS programs conducted between late 2017 and late 2019. The respondents represented 86% of participants across the five programs. The respondents were primarily current serving members of the ADF, with the inclusion of a few civilian first responders as outlined in the demographics (Table 1).
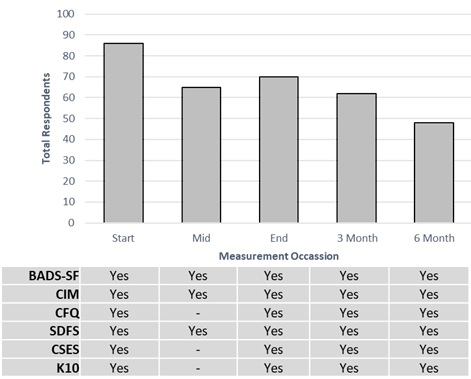
Procedure: At the start of each program, the prospective respondents were provided with an information pack including a research outline, respondent information statement and consent form via email. For the program participants who consented, a link to the Qualtrics online platform was sent at each measurement occasion. On each occasion, the respondent could complete the survey via phone, tablet or computer. For each respondent, there was a maximum of three measurement occasions during the program: (1) Days 3–5, (2) Days 12–14, (3) Day 28, plus three- and six-month follow- up occasions. Data collection for common factors, core self-evaluations and psychological distress occurred at the start, end, three- and six-month measurement occasions, with behavioural activation, belonging and flow occurring at all occasions, as shown in Figure 1. The study was approved by the Departments of Defence and Veterans Affairs Human Research Ethics Committee, Protocol 853-17.
Measures
Behavioural Activation for Depression Scale – Short Form (BADS-SF): The BADS-SF was used to measure behavioural activation. It consists of nine items, which were developed using a university population.13 For each item, the participant was asked to read a statement and rate how often the statement was true during the past week on a seven-point scale ranging from 0 (‘not at all’) to 6 (‘completely’). Five items concerned the frequency and quality of recent activities, e.g., ‘I was an active person and accomplished the goals I set out to do’. The other four items, which were reverse- scored, concerned avoidance and rumination, e.g., ‘I engaged in activities that would distract me from feeling bad’. The BADS-SF is reported to have sound psychometric properties, e.g., Cronbach’s α =.819.13
Community Integration Measure (CIM): The CIM is a measure of belongingness, which rates perceived connections within a community with respect to general assimilation, support, occupation and independent living.14 While originally designed for those who have had a traumatic brain injury, the measure has been validated by McColl, Davies, Carlson, Johnston and Minnes14 using both patient samples (Cronbach’s α =.830) and university samples (Cronbach’s α =.780). The CIM contains ten declarative statements, rated on a five-point Likert scale (always agree, sometimes agree, neutral, sometimes disagree, always disagree), where ‘always agree’ was coded as 5, and ‘always disagree’ was coded as 1. Higher scores are interpreted as reflecting higher levels of community integration.
Common Factors Questionnaire (CFQ): The CFQ was developed for this study from a list of 15 factors10
Table 1. Respondent demographics
| Demographics | |
|---|---|
| Gender | |
| Male | 65% |
| Female | 35% |
| Age | |
| <30 | 29% |
| 30-39 | 33% |
| 40-49 | 23% |
| 50-59 | 14% |
| >60 | 1% |
| Rank | |
| Officer | 26% |
| Senior Non-Commissioned Officer | 12% |
| Other rank | 55% |
| Civilian | 8% |
| Service | |
| Navy | 31% |
| Army | 46% |
| Air Force | 15% |
| Civilian | 8% |
| Creative Stream | |
| Visual arts | 40% |
| Creative writing | 22% |
| Acting and performance | 10% |
| Music and rhythm | 28% |
including, among others, rapport, trust, shared goals and empathy between a program participant and their instructor. The CFQ was designed to measure similar relationship factors deemed important in a variety of settings containing an artistic instructor. The questionnaire used a five-point Likert scale (strongly disagree, somewhat disagree, neither agree nor disagree, somewhat agree, strongly agree). Higher scores indicate a closer relationship between the respondents and their instructor. The questionnaire demonstrates appropriate reliability when tested with a university sample (N = 395) (Cronbach’s α =.822). Factor analysis revealed three factors, being instructor alliance, goal orientation and personal development.
Short Dispositional Flow Scale (SDFS): The SDFS provides a brief assessment of a nine-dimensional conceptualisation of flow state as a cognitive construct.15 The scale was developed using samples from the general Australian population (Cronbach’s a =.810). The scale contains nine statements concerning an activity nominated by each participant, for example, the artistic activity undertaken during the ARRTS program. The nominated activity rated the experienced flow state on a 5-point scale (never, rarely, sometimes, frequently, always) with higher scores indicating a greater sense of flow. For example, one statement is, ‘My attention is focused entirely on what I am doing’.
Core Self-Evaluations Scale (CSES): The Core Self- Evaluations Scale (CSES) was developed out of a four-component model of Core Self Evaluations and has been validated for measuring an individual’s aggregate evaluation for each factor.16 The scale consists of 12 items and uses a five-point Likert scale (i.e., strongly disagree, disagree, neutral, agree, strongly agree) to score responses. Examples of statements include, ‘I am confident I get the success I deserve in life’, and ‘I am filled with doubts about my competence’. The overall score has demonstrated a reliable Cronbach’s a of 0.88.
Kessler 10 (K10): The K10 is widely used to measure psychological distress based on anxiety and depressive symptoms.17 The K10 has ten items that each ask, ‘about how often did you feel…’, for example, ‘nervous’, ‘hopeless’, ‘depressed’, etc. Four items address anxiety symptoms, and six items address depressive symptoms. The response scale consists of a five-point rating ranging from ‘none of the time’ to ‘all of the time’. Thus, lower scores indicate less psychological distress. The K10 is reported to have sound psychometric properties, e.g., Cronbach’s α =.930 for the general population.17
Figure 1. Total respondents at each measurement occasion
Statistical analysis
Statistical testing was conducted using multivariate analysis of variance (MANOVA) for repeated-measure designs. For reporting MANOVA results, their textual description includes the F statistic and its p value.18 For significant effects, the effect size is also reported, using the d statistic, which represents the median of the 95% confidence interval for the difference among the contrast-weighted means expressed in standard deviation (SD) units. Using Cohen’s19 recommendations, effect sizes of 0.20, 0.50 and 0.80 SD units were considered small, medium and large, respectively.
Results
Behavioural Activation for Depression (BADS)
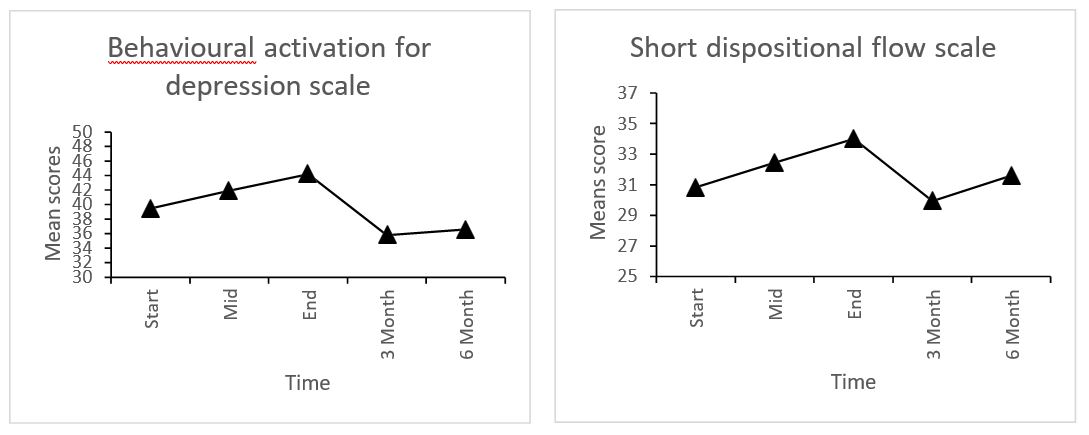
Figure 2, Panel A plots the mean behavioural activation scores from the BADS across five measurement occasions. The mean scores rose from 39.5 at the start of the program to 44.2 at the end of the program. Thereafter, across the three- and six- month follow-up periods, the scores dropped to 35.8 and 36.6, respectively. Across all occasions, there was significant curvature as seen in a medium-sized, quadratic trend F (1, 317) = 10.94, p <.01, effect size =.393.
Community Integration Measure (CIM)
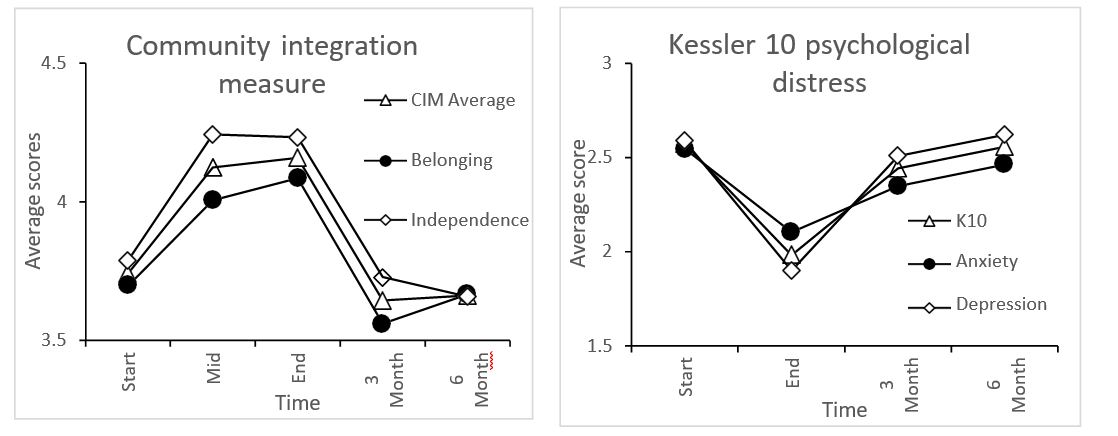
Figure 2, Panel B shows the average mean score for the CIM plus separate mean scores for the factors of belonging and independence. The three mean scores showed a pronounced rise from the start of the program to its midpoint, after which further rises were slight. After the program, the mean scores largely reverted to their starting point within the initial three-month follow-up period. The quadratic trend for the belonging factor was small and significant F (1, 316) = 7.05, p <.01, effect size =.317, while the quadratic trend for the independence factor showed a medium significant effect F (1, 316) = 18.70, p <.01, effect size =.510. Overall, the CIM as a joint measure of belonging and independent participation in a community had a small significant quadratic trend, F (1, 316) = 13.11, p <.01, effect size =.433.
Common factors
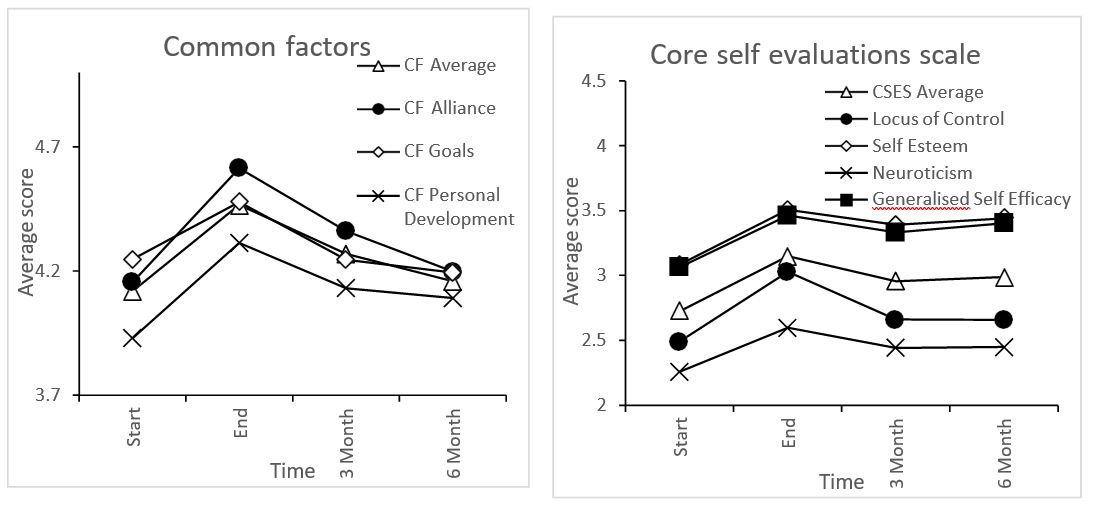
Figure 2, Panel C shows the average mean scores of common factors, including the three factors of therapeutic alliance, goals and personal development. Overall, all groups showed an increase in the experience of common factors from the start to the end of the program with a gradual decline over the three- and six-month period following the program. Overall, common factors as a total measure had a small significant quadratic trend F (1, 250) = 7.34, p <.01, effect size =.348. Among the three factors, therapeutic alliance had a pronounced quadratic trend, F (1, 250) = 14.00, p <.001, effect size =.481. Goals had no significant quadratic trend (p >.05), however, personal development had a small yet significant quadratic trend F (1, 250) = 5.02, p <.05, effect size =.288.
Flow state
Figure 2, Panel D shows the mean scores for the Short Dispositional Flow Scale (SDFS). Experienced flow states increased from the start of the program, through the middle stage, until the end of the program. Following the end of the program, flow states decreased at the three-month mark, prior to an upward excursion at the six-month mark. The planned statistical comparisons yielded a small yet significant quadratic trend F (1, 291) = 4.33, p <.05, effect size =.263. Regarding the apparent increase between three-month and six-month marks, a post- hoc test comparing them failed to reveal a significant difference, F (1, 291) = 2.30, p >.05, effect size =.320.
Core Self Evaluations (CSES)
Figure 2, Panel E plots the mean CSES scores, which showed a small significant quadratic trend over measurement occasions, F (1, 254) = 4.83, p<.05, effect size =.280. Among the four subscales, only locus of control showed a significant quadratic trend, F (1, 254) = 7.46, p <.01, effect size =.348.
Psychological distress
Figure 2, Panel F shows the mean K10 scores, including the means for the anxiety and depression factors. Overall psychological distress reduced throughout the program, as did the means for anxiety and depression. Following the program, psychological distress increased in the first three months with a further gradual increase over the period between three and six months. Overall psychological distress had a significant quadratic trend, F (1, 260) = 12.88, p <.01, effect size =.452. Similarly, there were significant, small quadratic trends for the anxiety scores, F (1, 260) = 6.98, p <.01, effect size =.333, and depression scores F (1, 260) = 13.21, p <.01, effect size =.458.
Figure 2. Longitudinal graphs of responses
A D
B E
C F
Discussion
Main Findings
Concerning the three research questions, the longitudinal pattern of the results consistently showed significant quadratic trends of small to medium size, with all effects reducing over time. The scores for the underlying mechanisms consistently grew throughout the program, but within the six- month follow-up period, returned their initial states. Conversely, the K-10 scores for anxiety and depressive symptoms showed an improvement as evidenced by a decline during the program followed by a return to their previous state during the follow- up period. Finally, the CSES showed a small rise followed by a return to baseline. Among the four subscales, only locus of control showed a significant quadratic trend.
Relationship of current findings to previous research
Longitudinal trends: The quadratic trends seen in the current results for the ARRTS program are consistent with the trends seen in the evaluation of established therapies, such as CBT, for anxiety and depressive symptoms. Meta analyses and systematic reviews of therapies for anxiety and depression have indicated, after an initial improvement during therapeutic intervention, the duration of treatment effectiveness only extends across intervals of a few weeks to a few months.20,21 In one longitudinal study, there was a 50% relapse rate for anxiety and depressive symptoms; clients who had residual depressive symptoms at the end of therapy were twice as likely to relapse in a 12-month follow-up period.22
Behavioural activation: The current findings established that art-based activities conducted by professional art instructors could achieve reductions in both anxiety and depressive symptoms among respondents. These reductions are consistent with previous findings23 that art professionals can promote behavioural activation without specific mental health training. Furthermore, the behavioural activation and reductions in anxiety and depression were short-lived, lasting no more than three months. This duration parallels the pattern revealed by a meta-analysis of the effects of behavioural activation interventions for 1–3 months post-treatment.24
Common factors: It has long been established that common factors are an important component of established therapies.25 The current research has for the first time demonstrated art-based activities delivered by art professionals could also engage the common factors. In particular, the common factors of therapeutic alliance and personal development were statistically significant, while apparent goal setting did not achieve significance.
Belonging: The current results add to previous evidence that people undertaking group art-based activities experience an enhanced sense of belonging alongside other positive therapeutic outcomes.4 This sense of belonging appears to temporarily fill the gap in belonging that the participants may experience when separated from their previous military unit. A sense of belonging to a military unit has been found to protect against anxiety and depression.26
Flow states: The current research adds to the existing evidence that concentrated engagement in art-based activities fosters a beneficial state of flow.27,28 Previously, flow has been postulated to be an underlying product of art-based activities, and therefore flow has a significant place in achieving positive outcomes in art therapy.29
Implications
To potentially prolong the beneficial effects of the ARRTS program and ones like it, a program of follow-up arts-based activities for participants may be worthwhile. In a previous paper in this series, Watt and Kehoe30 found that respondents were interested in ongoing participation in arts- based groups (55%) and/or a ‘catch-up’ with the respondents’ program members. In addition, there is evidence that individual and group skills are maintained by refresher sessions at three- to six- month intervals.31-34
Limitations and future directions
Although the number of respondents was limited, and there was attrition over the measurement occasions, the impact of the ARRTS program was consistent across participants. Thus, the analysis had the power to detect small to medium effects. A larger sample with the current ARRTS population, including the provision for a control group, would have been desirable. However, a proposal to create an untreated control group was rejected by the relevant ethics committee. A future way of increasing the power of analysis would extend the focus of arts- based activities beyond current ADF members to discharged veterans and other first responders.
This research focused on mechanisms engaged by the ARRTS program. The picture of the candidate mechanisms could be further refined. For example, a measure of working alliance specifically for artistic activities could be used.35 The focus of the effects of the program on a well-validated measure of anxiety and depression (K10) could also be expanded to include more global validated measures of outcomes such as quality of life, along with the ongoing benefits from the ARRTS program experienced by previous participants up to 48 months later.3 Given the longer duration of the experienced categorical benefits compared to the shorter-lived changes in the quantitative mechanism scores and K10, it would be worthwhile to follow up with future participants in any art-based activities using a suite of quantitative and categorical measures.
Conclusion
The positive impact of the ARRTS program for both present participants and those in the retrospective study3 was, it should be remembered, added to the already rigorous, multidisciplinary treatments of psychological and physical injury provided through the ADF. Although the effects of the arts-based activities were small to medium, they represent a cumulative contribution to the already substantial treatment received by the ARRTS participants. Future research is required to address the limitations of the current study further while seeking to create a greater understanding of the effect of the ARRTS program. Thus, there is reason to test whether it be worthwhile for the Department of Veterans Affairs and other related organisations to introduce corresponding arts-based programs for discharged personnel, who are often a risk of mental health challenges.27
Corresponding Author: T J Watt Authors: T J Watt1,2, E Kehoe1
Author Affiliations:
- UNSW, Psychology
- Australian Army



