Introduction
Musculoskeletal injuries (MSKI) are a common problem for militaries around the globe.1,2 Countries of the Five Eyes intelligence alliance (Australia, Canada, New Zealand, United Kingdom and the United States of America) spend millions of dollars on direct patient care in the treatment of MSKI. In 2017, Canada allocated nearly CA$200 million towards implementing strategies related to injury prevention for the Canadian Armed Forces (CAF).3 The CAF recognises MSKI as a fundamental factor impacting operational readiness and the health of its members, not to mention being the leading cause of medical attrition.4,5 MSKI are also the most common reason for a CAF member being unable to deploy.5
In 2010, Hauret et al. emphasised the need for both chronic and acute injury to be recognised in the US Department of Defence Traumatic Injury Incidence.2 At the time, only acute traumatic injuries were recorded, excluding common injuries such as tears of the meniscus or rotator cuff, stress fractures and recurrent shoulder dislocations.2 This recommendation to broaden the scope was significant since chronic injuries are often reported at a higher rate than acute MSKI in most military units.6,7 These injury types differ based on their origin. An acute injury results from a specific inciting event and has a precise mechanism.6 A chronic injury, also referred to as repetitive strain injury (RSI) or overuse injury, is caused by the cumulative effect of micro-traumatic forces, is progressive in nature and results from a combination of modifiable and non-modifiable risk factors.2,8
The literature is limited surrounding injury trends, mechanisms and occupational factors that contribute to MSKI in the CAF.9 Between-sex differences in MSKI have been observed in actively serving military members by other nations; however, available data on CAF members is minimal.9 -11 As the Department of National Defence of Canada (DND) has set a goal of increasing the presence of females in the CAF from 15% to 25% by 2026,3,9 building knowledge around sex-specific MSKI should be a priority. Furthermore, other nations have observed differences between occupational roles,6,12-14 with special operations forces, pilots and aircrew reporting significantly greater MSKI rates than other military occupations.6,13,15
The CAF and other nations have documented injuries involving the spine and neck of pilots at rates ranging from 70% to over 90%;1,15-18 other body regions are often not considered. Investigations and reporting of MSKI trends in active CAF members, male or female, are sparse and therefore limit determinations whether sex disparities exist among the ‘high risk’ occupational trades like pilots.7,9,17Personal protective equipment (PPE) such as helmets and night vision goggles (NVGs) have been associated with neck pain intensity and incidence.17-20 While neck pain and spine injury rates are important to track, especially when up to 80% of pilots report experiencing neck pain during their career,15,17 understanding MSKI for other body regions is also relevant.21 Expanding beyond the spine could help reduce pain affecting this body region in pilots, as neck pain is often associated with other factors, including mental health status and injuries to other areas.21,22 Shoulder injury, for example, is often associated with chronic neck pain that can be reduced with exercise protocols aimed at improving scapular kinematics.22 Knowledge of MSKI affecting other tissues and joints is imperative for rehabilitation and prevention purposes but has not been explored thoroughly in CAF pilots.13,23 Describing the different trends, types and associated factors of MSKI among male and female CAF pilots is essential for developing prevention strategies aimed at offsetting the impact on operational readiness and quality of life for these members.13,15,17,19 Thus, the purpose of this study is to provide a preliminary examination of possible sex disparities in MSKI experienced by actively serving CAF pilots and identify body regions most affected.
Materials and Methods
Participants and data collection
From September 2020 to February 2021, data for this cross-sectional study were collected via a questionnaire developed as part of the ‘Multi- stage approach to addressing sex-disparities in musculoskeletal injuries in military members’ research project. The aims of this project included assessment of MSKI, reproductive health and barriers to recruitment and retention in the CAF. The study inclusion criteria were: being a member of the CAF (past or present) and ages between 18–65 years. The research team and project stakeholders recruited via posters, social media, newsletters and snowball methods. The questionnaire was accessed, and informed consent was provided via the online cloud- based survey development software SurveyMonkey Inc. (San Mateo, USA). The local Research Ethics Board (H-04-19-3442) approved this study, and the procedures were performed in accordance with the Declaration of Helsinki.
For the present study analysis, data were included only from participants who identified as currently serving CAF pilots. Military Occupational Structure Identification (MOSID) or written response was provided in the descriptive section of the questionnaire to determine if a respondent was a pilot by trade. Actively serving was indicated by a response of ‘Regular Force’ or ‘Reserves Force Class A, B, C’ to the question ‘What category best describes your current status within the CAF?’. Responses of ‘Medically Released’ or ‘Retired’ were excluded. No pilot participants indicated ‘Intersex’ or ‘Prefer Not to Answer’ in response to ‘What was your sex at birth?’. Between-sex comparisons were conducted between ‘Male’ and ‘Female’. Demographic variables reported age (years), current weight (kg), height (m), body mass index (BMI; calculated as kg/m2) and years of service (years) were collected to characterise the population. Figure 1 illustrates the inclusion process flow chart.
Musculoskeletal injuries
For clarity on the definition of RSI, questions aimed at gathering chronic injury data were primed with the following statement: ‘Now questions on repetitive strain or overuse injuries. By this we mean injuries to muscles, tendons or nerves caused by overuse or repeating the same movement (e.g., ruck marching) over an extended period. For example, carpal tunnel syndrome, tennis elbow, plantar fasciitis or tendonitis. In case of retired/released members, please indicate the most accurate reply while a serving member.’ The participants were then asked, ‘While serving, did you ever have any injuries that you felt were due to repetitive strain?’ to which the possible responses were ‘Yes’ or ‘No’. If the response was ‘Yes’ to an RSI injury, the participant was asked, ‘What part(s) of the body were most affected by repetitive strain injuries (select all that apply)?’. For a complete list of possible body region responses, please see Appendix 1.
Questions aimed at gathering acute injury data were primed with the following statement: ‘Now some questions about serious acute injuries. Think about physical injuries, likely caused by a significant level of exertion or a single incident of trauma, which were serious enough to require at least 24 hours off work after it to recover from. For example, a broken bone, a sprain. In case of retired/released members, please indicate the most accurate reply while a serving member.’ The participant was then asked, ‘While serving, did you ever have any acute injuries that were serious enough to take at least 24 hours off from work?’ to which the possible answers were ‘Yes’ or ‘No’. If the participant responded ‘Yes’ to an acute injury that fit the description, they were asked, ‘Of the following injuries, what type(s) did you experience (select all that apply)?’ (Appendix 1). They were also asked, ‘What part(s) of the body were most affected by acute injuries that were serious enough to take at least 24 hours off from work (select all that apply)?’ (Appendix 1).
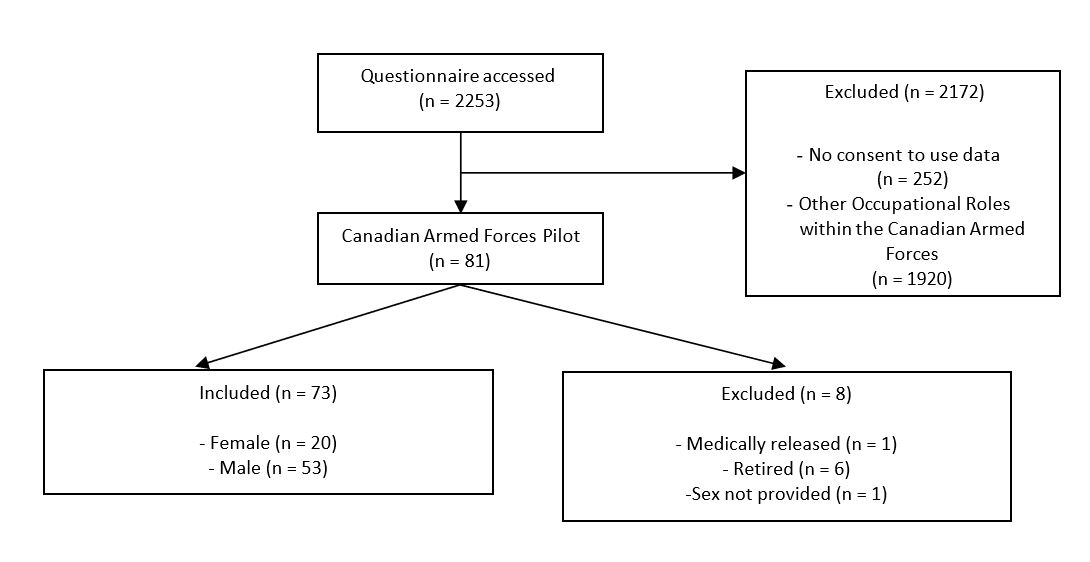
Figure 1. Flowchart of inclusion of participants
Impact of musculoskeletal injury
To understand how RSI impacted the career of participants, they were asked, ‘Do you feel any of your repetitive strain injuries impacted your career progression or length?’ to which the possible answers were ‘Yes’ or ‘No’. The same question was asked for acute injury.
Risk factors or mechanisms of musculoskeletal injury
Self-reported mental health and physical health were assessed on a 5-point Likert scale where participants indicated their health status as ‘Poor’, ‘Fair’, ‘Good’, ‘Very Good’, or ‘Excellent’. Responses were then grouped into ‘Good to Excellent’ and ‘Poor to Fair’.
To determine if the injury reported was related to military work, the participants were asked, ‘Do you feel that your major repetitive strain injuries were primarily a result of activity or activities related to military work requirements?’ and ‘Do you feel the activities primarily responsible for causing these acute injuries are related to your military work?’. Possible answers for both questions were ‘Yes’ or ‘No’. Regarding PPE and combat uniform size availability, participants were asked, ‘Overall, are/were you satisfied with the available combat uniform/PPE sizing?’. For the analysis, ‘Not satisfied’ and ‘Satisfied’ were combined and compared with ‘Indifferent’, ‘Somewhat satisfied’, and ‘Very Satisfied’. PPE and uniform comfort was determined by ‘Overall, how comfortable are/were you in your combat uniform (including PPE)?’ with the possible answers being ‘Very uncomfortable with movement limitations’, ‘Somewhat comfortable with some movement limitations’, ‘Somewhat uncomfortable with some movement limitations’, ‘Very comfortable with no movement limitations’, or ‘Indifferent’. For the analysis, ‘Very uncomfortable with movement limitations’, ‘Somewhat uncomfortable with some movement limitations’ were combined and compared with ‘Indifferent’, ‘Somewhat comfortable with some movement limitations’, and ‘Very comfortable with no movement limitations’. To indicate if PPE or uniform affected work performances, ‘Overall, has your uniform/PPE negatively affected your work performance’ was asked with possible answers of ‘Yes’ or ‘No’.
Statistical analysis
Data were presented descriptively as absolute (n) and relative (%) frequencies, as well as mean ± standard deviation (SD). Data normality was checked using the Shapiro-Wilk test. Comparisons between sexes for the continuous variables were performed using the independent t-test for normally distributed variables and the Mann-Whitney test for the non-normally distributed variables. Chi-square test, Fisher’s Exact test and likelihood ratio were used when applicable to determine the association between sex and the MSKI-related variables in the full population and among only those who reported having an injury. Significance level was set at p-value < 0.05. All analyses were conducted with IBM SPSS Statistics version 27 (SPSS Inc., Chicago, Ill, USA). The participants who answered ‘No’ to overall RSI or acute injury were included in all body region and acute injury type analysis as ‘No’. Additionally, participants who answered ‘No’ to overall RSI or acute injury were included as ‘No’ in the analysis of injury impacting the participants’ career.
Results
Descriptive data
Of the 2001 participants that gave consent to the questionnaire, 73 respondents indicated they were actively serving pilots using provided MOSID and CAF status. Twenty of the pilots identified as female, 53 as male, with demographic information outlined in Table 1.
Repetitive strain injuries
Eighty per cent of females compared to 49.0% of males (p = 0.017), reported having RSI while serving. Significant differences were also observed when stratified by body region (see Figure 2). The most commonly reported body regions for RSI were neck, lower and upper back.
Table 1. Characteristics of Canadian Actively-Serving Pilots by Sex (n = 73)
| Category | Total Mean + SD or Frequency (%) | Females Mean + SD or Frequency (%) | Males Mean + SD or Frequency (%) | Between-sex significance (p-value) |
|---|---|---|---|---|
| n | 73 | 20 | 53 | – |
| Age | 38.7 + 10.3 | 35.6 + 7.2 | 39.9 + 11.1 | 0.146 |
| Height (m) | 1.8 + 0.1 | 1.7 + 0.1 | 1.8 + 0.1 | < 0.001* |
| Weight (kg) | 83.6 + 13.7 | 83.9 + 11.6 | 83.5 + 14.3 | 0.890 |
| BMI (kg/m2) | 26.3 + 4.2 | 25.4 + 5.3 | 26.7 + 3.6 | 0.053 |
| Years of Service | 18.1 + 9.7 | 15.3 + 6.6 | 19.2 + 10.5 | 0.128 |
| Mental Healtd (% of ‘Good’, ‘very good’, and ‘excellent’)# | 84.8 | 80.0 | 87.0> | 0.476 |
| Physical Healtd (% of ‘Good, ‘very good’, and ‘excellent’)# | 92.4 | 100.0 | 89.1 | 0.312 |
| PPE size availability satisfaction (% of ‘not satisfied’ and ‘somewhat satisfied’)† | 54.5 | 68.4 | 48.9 | 0.150 |
| Levels of PPE comfort satisfaction (% of ‘Very uncomfortable witd movement limitations’ and ‘somewhat comfortable witd some movement limitations’)† | 36.4 | 68.4 | 23.4 | <0.001* |
Data was presented as mean + SD for continuous variables and frequencies (%) for categorical variables. BMI = body mass index; kg = kilograms; m = meters; SD = standard deviation; PPE = personal protective equipment.
Between-sex differences for body weight were compared using independent t-test. All other continuous variables were compared using Mann-Whitney test. Between-sex differences for PPE size and PPE comfort were analyzed using Chi- square and for Mental Health and Physical Health using Fisher Exact test.
*Significant difference between sexes (p < 0.05). #Total sample size is n = 66 (n = 20 females and n = 46 males). †Total sample size is n = 66 (n = 19 females and n = 47 males).
When asked if the reported RSI has impacted career progression or career length, 20.9% of pilots responded ‘Yes’, with no significant difference between males (18.5%) and females (25.0%; p = 0.706).
Acute injuries
Acute injury prevalence for females was 65.0% compared to 43.0% for males (p = 0.100). No between- sex differences were observed between acute injury type (see Figure 3b). Sprains and strains were the most commonly reported acute injury type for both males (34.0%) and females (40.0%) with no sex differences (p = 0.631). Acute injury rates by body region for total, male and female are outlined in Figure 3a. Head (p = 0.044) and neck (p = 0.048) injury rates significantly differed between sexes with females reporting higher frequencies.
When asked if the reported acute injuries had an impact on career progression or length, 17.7% of pilots responded ‘Yes’, with no significant difference between males (19.1%) and females (15.4%) (p = 1.000).
Physical and mental health status
Analysis of physical and mental health was conducted with 20 female and 46 male participants (Total N = 66) due to missing data for these additional questions. No significant difference between males (89.1% ‘Good’ to ‘Excellent’: 10.9% ‘Poor’ to ‘Fair’) and females (100.0% ‘Good’ to ‘Excellent’: 0.0% ‘Poor’ to ‘Fair’) was observed in physical health rating (p = 0.312). Of the pilots who reported RSI, no significant difference was observed in physical health status between males (80.0% ‘Good’ to ‘Excellent’: 20.0% ‘Poor’ to ‘Fair’) and females (100.0% ‘Good’ to ‘Excellent’: 0.0% ‘Poor’ to ‘Fair’) (p = 0.137). Of the pilots who reported acute injuries, no significant difference in physical health status was observed between females (100.0% ‘Good’ to ‘Excellent’) and males (81.2% ‘Good’ to ‘Excellent’: 18.2% ‘Poor’ to ‘Fair’; p = 0.274). Overall, 84.8% of pilots rated their mental health as ‘Good’ to ‘Excellent’, while 15.2% reported as ‘Poor’ to ‘Fair’, with 80.0% of females and males 13.0% indicating the lower levels (‘Poor’ to ‘Fair’). No difference between females and males for low levels of mental health status in pilots who had RSI (18.8% vs 12.0%, respectively, p = 0.662) or acute injury (30.8% vs 22.7%, respectively, p = 0.698) was reported.
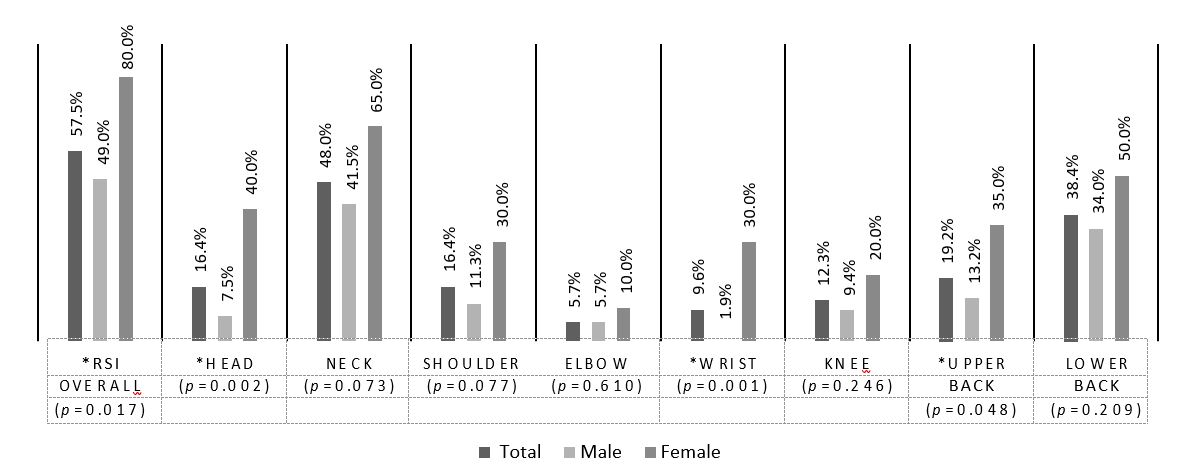
Figure 2. Rates of repetitive strain injuries by body region (Total [n = 73], Males [n = 53], Females [n = 20])
*Significant difference between sexes (p < 0.05). RSI = Repetitive Strain Injuries
Personal protective equipment
Of the 19 females and 47 males (reduced sample size due to missing data) that responded to the questions related to PPE (n = 66), 42.1% of females indicated their PPE negatively affected work performance compared to 25.5% of males (p = 0.185). Lower levels of PPE comfort (‘Very uncomfortable with movement limitations’ and ‘Somewhat uncomfortable with some movement limitations’, compared with ‘Indifferent’, ‘Somewhat comfortable with some movement limitations’, and ‘Very comfortable with no movement limitations’) were reported by 68.4% of females compared to 23.4% of males (p < 0.001). Female pilots who had RSI reported low levels of PPE comfort at a higher rate than males (75.0% vs 21.7%, respectively, p < 0.001). Similarly, female pilots who had acute injuries reported lower levels of PPE comfort at a higher rate than males (83.3% vs 20.0%, respectively, p < 0.001).
Overall, no significant difference was observed in PPE size availability (p = 0.150), with low levels of satisfaction (‘Not Satisfied’ to ‘Satisfied’ compared to ‘Indifferent’, ‘Somewhat Satisfied’, and ‘Very Satisfied’) reported by 68.4% for females and 48.9% for males. Pilots who had RSI reported low levels of satisfaction with PPE size availability (‘Not Satisfied’ to ‘Satisfied’ compared to ‘Indifferent’, ‘Somewhat Satisfied’ and ‘Very Satisfied’) at rates of 75.0% for females compared to 47.8% for males (p = 0.090).
No sex-disparity detected between female and male pilots with acute injury reporting low levels of satisfaction with PPE size availability (83.3% vs 55.0%, respectively, p = 0.139).
Discussion
Findings from this exploratory study suggest that sex-related differences in MSKI exist among pilots in the CAF. In particular, several sex-related differences were observed for injury types, and certain areas of the body were affected at a greater frequency than others. While the most reported anatomical regions affected by RSI, regardless of biological sex, were the back (upper and lower), shoulders and neck, females reported more RSI of the head, neck and upper back compared to their male counterparts. Female pilots also presented a higher prevalence of overall RSI. Body regions most commonly affected by acute injury were the neck, shoulder, knee and ankle. The rate of acute injury to the head and neck was higher for females versus males. Our findings are in agreement with other reports on pilots, with the neck being the most common region affected by RSI and acute injury,13,18,20,24 and we add novel information highlighting greater susceptibility among female CAF members.
The female spine differs from the male in that the thoracic region is less kyphotic and the cervical spine is almost straight (slight kyphotic), whereas the male cervical spine is typically lordotic and the thoracic spine more kyphotic.24 These anatomical differences tend to contribute to an increased risk of whiplash trauma and more severe clinical outcomes for females in automobile crashes.25,26 While whiplash was not expressly examined, this study differs from others involving military pilots in that we also described acute injury types. To this point, though sex disparities were not found for acute injury type, sprains and strains were identified as the most common form of acute injury. This information can guide targeted prevention strategies that include protective measures for body regions most at risk of sprains and strains.
(a)
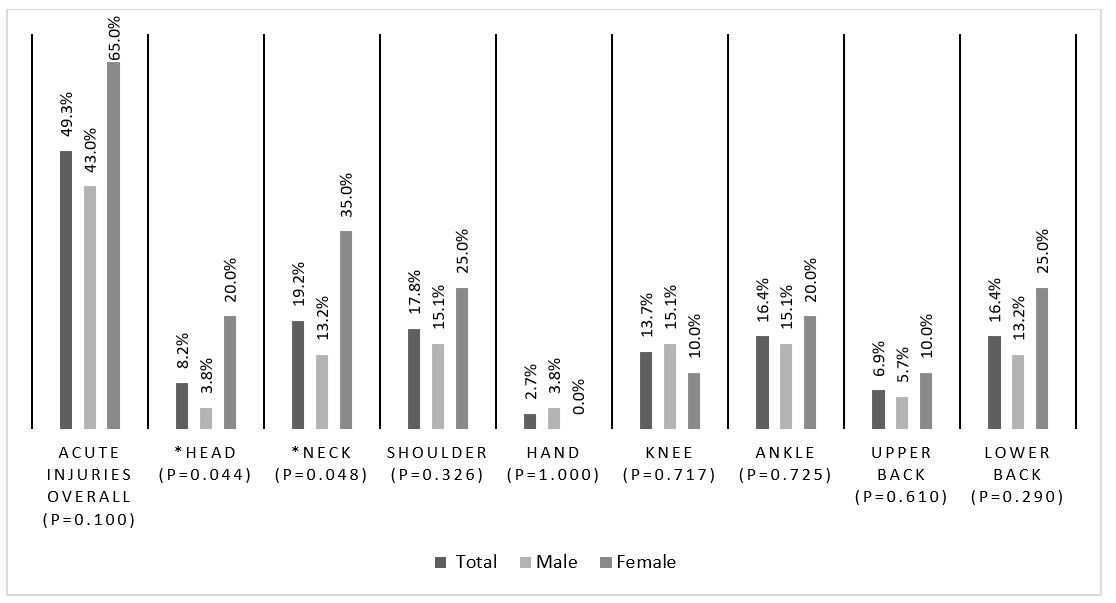
(b)
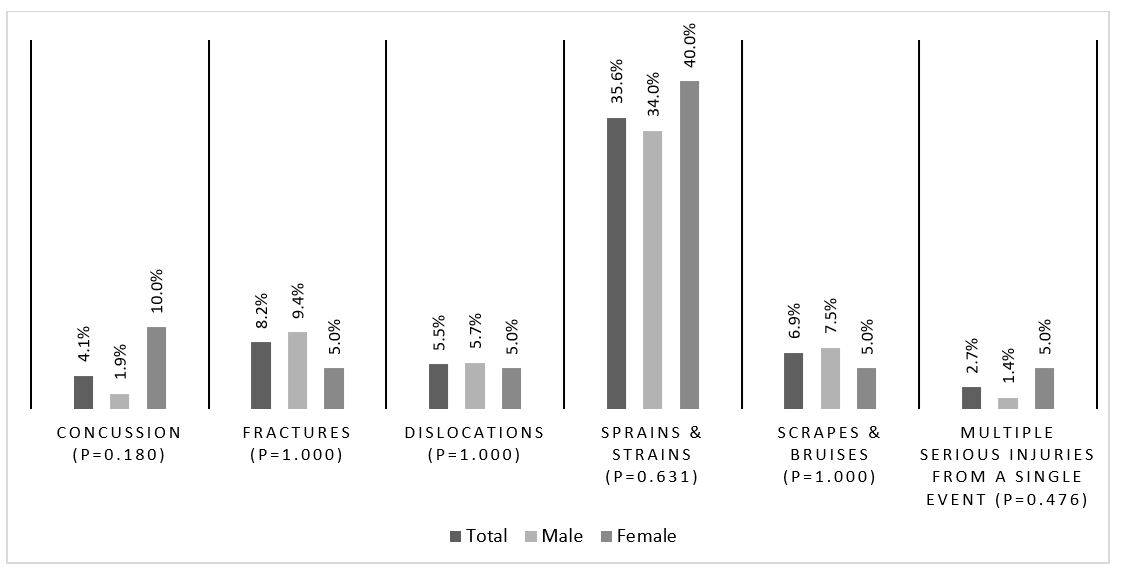
Figure 3. Rates of Acute Injury by Body Region (a) and by Type (b). Total [n = 73], Male [n = 53], And Female [n= 20]
*Significant difference between sexes (p < 0.05)
Beyond the neck, other body regions most affected by RSI in our findings are in accordance with previous reports of upper-body injury and pain among both fixed and rotary wing pilots.13,17,20,27 More research is needed to inform physical training, PPE and MSKI education strategies to address the increased risk of injury in the female pilot.
As mentioned previously, associations between mental and physical health factors and MSKI risk have been identified in military populations.1,13,16,20,27 Though perceptions of mental health have been associated with injury and pain in body regions around the spine,1 our findings indicate the majority of CAF pilots perceiving their mental health as ‘good’ to ‘excellent’, regardless of sex or injury history. Exploring psychosomatic factors associated with MSKI in CAF pilots might offset performance deficits that can occur when experiencing pain.16 Although most of the respondents in the present analysis indicated high mental health status, future studies might evaluate mental health using validated assessment measures to assess the impact this may have on injury risk. Regarding physical health, similar to Tegern et al.,13 our results suggest most CAF pilots, irrespective of sex and injury status, perceive their physical health as ‘good’ to ‘excellent’. Our questionnaire did not include physical fitness levels beyond achieving the minimum fitness standard of the CAF, though other nations have identified high levels of physical fitness as protective against MSKI in pilots.27 Future research is recommended to objectively assess physical health markers and define optimal levels of physical fitness for CAF pilots to be protected against MSKI. Physical training programs aimed at supporting the CAF pilot should consider total physical output (occupational, physical training and lifestyle) as high volumes of physical activity have been identified as a risk factor for MSKI;27-29 longitudinal studies to better understand the effect of exercise training type, intensity and load are recommended.
PPE (e.g., helmets, body armour and NVGs) has previously been associated with MSKI in pilots.17,27,30 Our findings suggest that PPE and uniform size availability is less than satisfactory for CAF pilots.
Low levels of satisfaction with PPE comfort were consistently reported in pilots with both RSI and acute injury, with females being more affected. Poorly fitting PPE is a common problem for females in tactical roles.31 Small innovations have been made, including the creation of ballistic vests designed for the female torso.32 Other militaries and police forces now provide body armour tailored to the female anatomy, though it is not currently available for CAF members.31 Introducing ballistic vests specifically designed for females would benefit pilots as unisex body armour is wide at the chest, limiting shoulder flexion required for tasks like shooting and operating an aircraft.31 Investigations into PPE and uniform size and procurement of equipment designed for the tactical female may benefit MSKI reduction strategies, as has been previously recommended.30
The participants in the present study were not asked to identify their aircraft,and determining MSKI risk differences based on plane or helicopter models is beyond the scope of this study. However, when comparing neck pain intensity and incidence in CAF helicopter crews, CH-146 Griffon aircrew appear to be at higher risk than others due to aircraft design and physical demands during flight.17 Sustained awkward postures, combined with vibration, G-force and PPE, are frequently cited as mechanisms for MSKI in male pilots.17,20,24,27,33 A review of the literature and recent data suggest that no between- group differences in MSKI rates exist between fixed and rotary wing male pilots, justifying our inclusion of both.13,24
This study represents a secondary analysis of data from a self-report questionnaire that was aimed at understanding MSKI, reproductive health and other health-related factors in the CAF. The questions were not aircrew or pilot-specific; investigation to better understand mechanisms and factors associated with MSKI in this population is recommended. While the sample size available for this analysis was small, it has a higher representation of female pilots compared to other studies (n = 20 in our study vs n = 10 from previous research), allowing for between-sex comparisons.18 Further, this study has a representation of 27.4% female, which is higher than the Royal Canadian Airforce membership of 17% female.34 Another strength is the inclusion of both RSI and acute injury data. The cross-sectional design does not permit establishment of causality; as such, our findings are intended to be used as a guide for future investigations aimed at identifying causal factors of MSKI among CAF pilots.
Despite generally reporting good levels of perceived physical and mental health, MSKI rates for CAF pilots are high. In addition, female CAF pilots appear to be at greater risk of RSI, and sex disparities exist in body regions most affected by MSKI. Research is needed to guide strategies aimed at mitigating sex disparities in MSKI and reducing the overall burden of these injuries on CAF pilots.
Corresponding Author: Kristi Adamo, Kristi.Adamo@uottawa.ca
Authors: C Edwards, D da Silva, T Nagpal, S Souza, J Puranda, K Semeniuk, K B Adamo
Author Affiliations:
1 University of Ottawa – Faculty of Health Sciences 2 Brock University
Appendix 1– List of questions and answers from the survey used to determine the information analysed in the present study (n = 16 questions).
Question: Which category best describes your current status within the CAF?
Answer:
a) Regular Force
b) Reserve Force Class A, B, C
c) Retired
d) Medically Release
e) Other – please specify:
Question: What was your sex at birth? Answer:
a) Male
b) Female
c) Intersex
d) refer not to answer
Question: Overall, are/were you satisfied with the available combat uniform/PPE sizing?
Answer:
a) Not satisfied
b) Satisfied
c) Indifferent
d) Somewhat satisfied
e) Very Satisfied
Question: Overall, how comfortable are/were you in your combat uniform (including PPE)?
Answer:
a) Very uncomfortable with movement limitations
b) Somewhat comfortable with some movement limitations
c) Somewhat uncomfortable with some movement limitations
d) Very comfortable with no movement limitations
e) Indifferent
Question: Overall, has your uniform/PPE negatively affected your work performance?
Answer:
a) Yes
b) No
Repetitive Strain Injury
Now questions on repetitive strain or overuse injuries. By this we mean injuries to muscles, tendons or nerves caused by overuse or repeating the same movement (e.g., ruck marching) over an extended period. For example, carpal tunnel syndrome, tennis elbow, plantar fasciitis or tendonitis. In case of retired/released members, please indicate the most accurate reply while a serving member.
Question: While serving, did you ever have any injuries that you felt were due to repetitive strain?
Answer:
a) Yes
b) No
Question: What part(s) of the body were most affected by repetitive strain injuries (select all that apply)?
Answers:
a) Head, Eyes, Ears (e.g., eye strain)
b) Neck,
c) Shoulder,
d) Upper arm
e) Elbow,
f) Lower arm
g) Wrist (e.g., carpal tunnel)
h) Hand
i) Thumb (e.g., BlackBerry thumb)
j) Other fingers (e.g., sniper finger) Hip
k) Thigh
l) Knee (e.g., bursitis)
m) Lower leg (e.g., shin splints)
n) Ankle (e.g., Achilles tendonitis)
o) Foot (e.g., plantar fasciitis)
p) Toes
q) Upper back or upper spine, excluding neck
r) Lower back or lower spine
s) Chest, excluding back and spine
t) Abdomen or pelvis, excluding back and spine
u) Other – please specify:
Question: Do you feel any of your repetitive strain injuries impacted your career progression or length?
Answer:
a) Yes
b) No
Question: Do you feel that your major repetitive strain injuries were primarily a result of activity or activities related to military work requirements?
Answer:
a) Yes
b) No
Acute Injury
Now some questions about serious acute injuries. Think about physical injuries, likely caused by a significant level of exertion or single incident of trauma, which were serious enough to require at least 24 hours off work after it to recover from. For example, a broken bone, a sprain. In case of retired/ released members, please indicate the most accurate reply while a serving member.
Question: While serving, did you ever have any acute injuries that were serious enough to take at least 24 hours off from work?
Answer:
a) Yes
b) No
Question: Of the following injuries, what type(s) did you experience (select all that apply)? Answers:
a) Concussion/head injury
b) Broken or fractured bones
c) Dislocation
d) Sprain or strain, including torn ligaments and muscles
e) Scrapes, bruises, blisters, including multiple minor injuries
f) Multiple serious injuries, resulting from a single event (exclude multiple minor injuries)
g) Other – please specify:
Question: What part(s) of the body were most affected by acute injuries that were serious enough to take at least 24 hours off from work (select all that apply)?
Answers:
a) Head, Eyes, Ears (e.g., eye strain)
b) Neck,
c) Shoulder, Upper arm
d) Elbow,
e) Lower arm
f) Wrist
g) Hand
h) Breast
i) Hip
j) Thigh
k) Knee, lower leg,
l) Ankle, foot
m) Other – please specify:
Upper back or upper spine, excluding neck lower back or lower spine chest, excluding back and spine abdomen, excluding back and spine pelvis, excluding back and spine
Question: Do you feel that any of your acute injuries impacted your career progression or length?
Answer:
a) Yes
b) No
Question: Do you feel the activities primarily responsible for causing these acute injuries are related to your military work?
Answer:
a) Yes
b) No
Health Status
The following questions relate to your perceptions about physical and mental health in general. For retired/released members, please indicate the most accurate reply while a serving member.
Question: In general, how would you rate your physical health?
Answer:
a) Poor
b) Fair
c) Good
d) Very good
e) Excellent
Question: In general, how would you rate your mental health?
Answer:
a) Poor
b) Fair
c) Good
d) Very good
e) Excellent


