Dysentery (blood and pus in faeces) has been an epidemic disease in armies throughout history. The Australian Imperial Force (AIF) encountered epidemic dysentery in both Gallipoli in 1915 and Palestine in 1918. During World War II, dysentery epidemics were a military problem in Queensland and Northern Territory. A massive dysentery epidemic involving AIF soldiers, Japanese soldiers and civilians was prominent in Papua New Guinea during 1943, killing thousands in the highlands. Prisoners of War (POW) in Asia, particularly along the Burma–Thailand Railway, died at high rates from chronic dysentery. Where available, as in Australia, successful treatment with early antibiotics such as sulphaguanidine limited mortality. Dysentery during field exercises was seen in Australia during the 1960s and remains a modern risk, especially in developing countries and in refugee camps, complex emergencies and natural disasters when sanitation measures fail.

Figure 1: Pioneers of the 1st BN AIF on the Gallipoli Peninsula in August 1915. They are making wooden latrines (‘thunderboxes’) during the height of the dysentery epidemic.1 AWM photo C01921, now in the public domain.
Dysentery is defined as blood and pus in diarrheal stools. It has cast a shadow over military operations for centuries and the Australian Defence Force since its beginning. Traditionally separated into bacillary (usually caused by Shigella sp) and parasitic (usually caused by Entamoeba histolytica) forms, both are highly infectious by faecal–oral spread. Although potentially lethal, dysentery’s great military impact is from its ability to make many men suddenly ill during sieges or invasions. Epidemic dysentery occurs when soldiers are crowded into unhygienic situations, as happened on the Gallipoli Peninsula in 1915. Particular risk factors during the Gallipoli campaign were the rocky soil preventing normal latrine construction (see Figure 1), extreme limitation of water supplies for washing, and a tactical situation that left men crowded into trenches for days with nowhere else to defecate. The Official History states that ‘“Dysenteric diarrhea” had become almost universal’, meaning that Gallipoli for the ANZACs of 1915 was like a siege in the pre-antibiotic era. Fifty Australian soldiers are listed as having died of dysentery with an approximate case fatality rate of 5%. However, it was the primary cause of medical evacuations, which peaked at >10% of the force in a single week. Temporising control measures to screen food and burn animal manure to reduce flies were insufficient to impact the spread of dysentery and only decreased as cold weather developed. Dysentery was one of many factors that led to the debilitation of soldiers on Gallipoli and the eventual abandonment of the position as untenable.
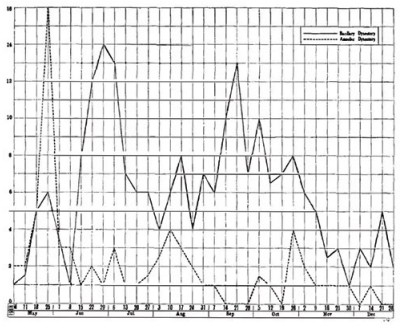
Figure 2: Weekly dysentery cases/1000 men in the Desert Mounted Corps of the Egyptian Expeditionary Force in Palestine during 1918. Graph 13 from summer in the Jordan Valley in the Official History of the War.
Dysentery also had a significant role in the Palestine campaign of 1918 when the ANZAC Corps consisted largely of mounted infantry in the extremely hot Jordan Valley during the summer. Holding such inhospitable territory against the Turkish Army was difficult, and dysentery/diarrhea was a constant factor, as seen in Figure 2. Blackburn described the clinical picture with a predominance of bacillary cases for which there was no treatment, although amoeba could be treated with emetine. Twenty per cent of autopsies performed by Fairley at No 3 Australia General Hospital in Egypt showed amoeba. Therefore, most deaths were either acute infections driven by the Shiga bacterial toxin or chronic infections resulting in malnutrition and debilitation.
Later the desert campaigns in the Middle East from 1940 were familiar territory to the Australian Army of World War II in Egypt, where dysentery continued to be a pervasive medical problem. The principal advance in therapeutics was the earliest sulpha drugs, as the poorly absorbed sulphaguanidine performed well against Shigella in the pre-resistance era of antibiotics. During the war, hundreds of thousands of tablets of sulphaguanidine were used to get sick soldiers back into action and likely inadvertently helped enteric organisms evolve drug resistance factors.
During the mobilisation of troops in Australia, especially after the bombing of Darwin in 1942, dysentery was a problem in rural areas where the military infrastructure to defend the country was being established. The Northern Territory was a hub for such activities, and a General Hospital there recorded 114 cases in which 6 days of treatment with sulphaguanidine was usually sufficient to return soldiers to duty. In central Queensland, an unfamiliar species of Shigella was encountered in 42 soldiers, which was eventually described as Shigella boydii. The common risk factor for Shigellosis was not geography as much as poor sanitary infrastructure leading to epidemics.
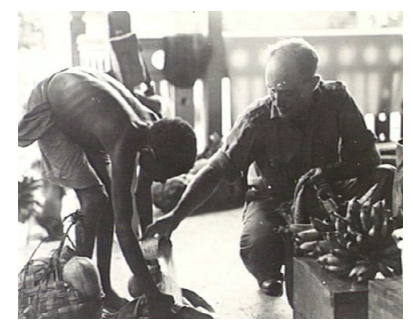
Figure 3: Australia and New Guinea Administrative Unit (ANGAU) officer exchanging rice for fruit on Karkar Island, 4 Jun 1944, where it was estimated that a high proportion of inhabitants had developed dysentery and malnutrition during the Japanese occupation. AWM photo 073824, now in the public domain.
By 1943 when the Australian Army had primarily moved to New Guinea, it was thought that dysentery was becoming a manageable medical problem, at least within the military. This did not account for the highly toxic form of the disease caused by Shigella dysenteriae, the introduction of which was blamed on the Japanese invaders. A case series of 503 soldiers from a military hospital in New Guinea showed that 13% of the more than 1000 dysenteric organisms isolated were due to this remarkably pathogenic organism with a potent toxin. Worse was to come as Shigella dysenteriae began journeying through the highly populated but socially isolated highland areas where civilians became collateral damage during the fighting. Although the severity and lethality of dysentery in otherwise healthy New Guinea men was known from the mining camp epidemics affecting contract labourers, its impact on entire communities was greatly magnified in 1944 by its ability to disrupt village food supplies that were already tenuous due to wartime logistical disruptions. See Figure 3. A staggering number of patients were admitted to an increasing number of emergency hospitals during 1944. Dysentery progressively moved across the New Guinea highlands in a fitful manner, even reaching isolated tribal groups uninvolved in the conflict as the pathogen was carried by people travelling across the rugged mountain paths. No one knows how many thousands of civilians died in Papua New Guinea during the wartime dysentery epidemics. However, post-war surveys of village populations suggest that 5% of populations died in some groups, and many took over a generation to recover their previous numbers.
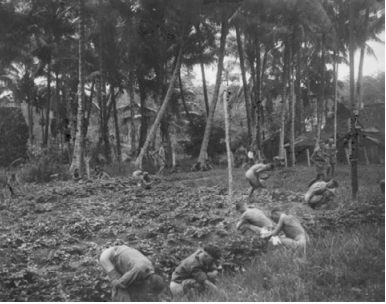
Figure 4: Allied POWs of ‘F Force’ suffering from dysentery relieving themselves while on a break from the train ride into Thailand to work on the Burma–Thailand Railway 1943. AWM photo P02569.184 now in the public domain by PTE George Aspinall
Prisoners of War (POWs) were particularly affected during World War II, where dysentery was one of the leading causes of death in Australian soldiers captured by the Imperial Japanese Army. Rarely was this a single event, as dysentery usually worked with a variety of factors to wear down a prisoner’s resistance until he succumbed; ‘Dysentery did kill large numbers of British, Australian and Allied men in Japanese prisons and working camps, not so much through lack of therapeutic agents, but through concomitant malnutrition, exhaustion and disease.’ Those working on the Burma–Thailand Railway were particularly at risk, with entire wards of the camp hospitals dedicated to dysentery patients (see Figure 4). In the absence of even basic medications in POW camps, other interventions were tried in an attempt to halt the mortality from chronic dysentery, such as diverting colostomies and whole blood transfusions. Given the extreme circumstances, it is a wonder that the mortality rates were not greater than that observed, with roughly one-fifth dying in the camps overall, with particularly unfortunate groups experiencing overall mortality rates up to 40%. High mortality rates were not confined to western soldiers as many Chinese and Korean POWs died of dysentery during the Korean War.
Dysentery was primarily a problem of small-scale outbreaks in particular units during the Australian Army’s participation in the Vietnam War during the 1960s. A 1969 twelve-soldier outbreak of Shigella flexneri in a signals unit caused the entire unit to be quarantined to prevent a larger epidemic in the entire brigade at Vung Tau. The small infectious dose of Shigella meant that any breakdown in field sanitation, sometimes occurring during unit parties, could be followed by an epidemic of dysentery. Not all outbreaks occurred overseas; one epidemic was observed in military reservists on exercise in South Australia in 1964. Advances in antibiotics meant dysentery was not a lethal event during the Vietnam War but certainly was a major infectious disease threat with the more generic diarrhoeas. Since the Vietnam War, the Australian Army has been deployed into many complex emergency and post-disaster missions where a breakdown in water and sanitation systems, poor food safety and displaced populations raise the possibility of dysentery epidemics. The Goma refugee camps in Zaire (now the Democratic Republic of Congo) were a spillover effect of the Rwandan war and genocide. Despite the emphasis on cholera in refugee and internally displaced persons camps, more deaths may have been due to drug-resistant Shigella dysenteriae, as enteric contamination rarely involves a single pathogen. In 2013, a large outbreak of Shigellosis commenced in an internally displaced persons camp in Papua New Guinea, resulting in around 1200 cases. The Cox’s Bazar region of Bangladesh hosts the highest density of refugees anywhere in the world. In 2017, outbreaks of bloody diarrhoea were reported to have a significantly higher case fatality rate than outbreaks of acute watery diarrhoea among the refugees in Cox’s Bazar, who had fled violence in Myanmar. As seen in New Guinea in 1944, epidemics of dysentery spread outwards from the main conflict zones to involve civilian populations otherwise uninvolved in the complex public health emergency. Globally, dysentery remains an important disease, especially in developing countries and in countries affected by humanitarian emergencies. In 2016, Shigella was the second only to rotavirus as a cause of diarrhoea mortality. War and extreme disruptions of civil communities by other disasters in the future will continue to carry the risk of dysentery epidemics; it is well we learn from our corporate history to avoid the worst outcomes when pathogens and disasters interact to the detriment of stressed populations.






