In the early 1950s, the British mathematician Alan Turing argued that for a computer to be described as intelligent it must be able to deceive a human into believing that the computer was human.1Whilst we have yet to reach this stage considerable advances have been made in the development of artificial intelligence and expert systems. Artificial Intelligence has been defined as ‘the creation of computer programs that do things that require intelligence’. Expert Systems, a subset of Artificial Intelligence, utilise computerised reasoning based on specific expert knowledge. This use of computerised reasoning or rules combined with an expert knowledge base differentiates these systems from decision support systems. In this paper, the application of expert systems to medicine in general, and the Defence medical arena, in particular, will be reviewed.
Expert systems designed for medical purposes have been an integral part of the historical development of Artificial Intelligence expert systems. One of the earliest expert programs developed, using List Processing (LISP), was a psychotherapist program named DOCTOR. 1 As research continued, particularly at Stanford University and the Massachusetts Institute of Technology (MIT), further rule based system were developed. At Stanford, an expert system called MYCIN was developed to diagnosis blood and brain infections and to recommend appropriate therapy a system which proved to be as nearly as accurate as human physicians. 1The inference engine from MYCIN, dubbed Essential MYCIN (EMYCIN), was used to develop many new expert systems. CADUCEUS (INTERNIST) an expert system developed at the University of Pittsburgh to encompass the diagnostic knowledge of over 700 diseases, was an even more challenging project.1 The roots of most of today’s medical expert systems are derived from MYCIN, CASNET (glaucoma diagnostic system) and INTERNIST.
The expert system consists of a number of components. These include the knowledge base, which contains the expert information and ‘rules of thumb’ required to make decisions; the inference engine which problem solves; the knowledge acquisition subsystem, which allows the system to be updated and its rules to be amended: the explanation subsystem, which explains the rationale behind the decision and the communication interface with the user. A graphical representation of the system is in Figure 1. In medicine, expert systems are generally limited to systems designed for clinical decision making. These are generally either rule-based systems (IF….THEN), which have developed from original MYCIN and the EMYCIN inference engine, 4or, more recently, artificial neural networks.5 The rule-based systems have been used to develop other experts diagnostic and therapeutic systems like ONCOCIN (Cancer protocols) and PUFF (Pulmonary function); teaching tools like GUIDON and NEOMYCIN, 3and Quality Assurance systems like the ATTENDING expert critiquing system. 6 Artificial neural networks are having increasing application in the diagnosis of disease conditions from radiological images to pathological slide images.
Medical expert systems have the capability to provide improved access to a wider range of expert knowledge, increase consistency in the use of specific medical knowledge and aid in problem-solving and strategic planning.; Expert systems have, as yet, received only minimal utilisation within Defence medical services, either in Australia or overseas. Perry describes the potential for these systems within the United States (US) Air Force but stresses the need for coordination across the US Department of Defence. There is, however, much scope for the use of expert systems, both medically and militarily, and their application will be explored further. To assist in a systematic review, expert systems can be classified broadly into functional areas. These include medical diagnostics and therapeutics, computerised medical records, quality assurance and training.
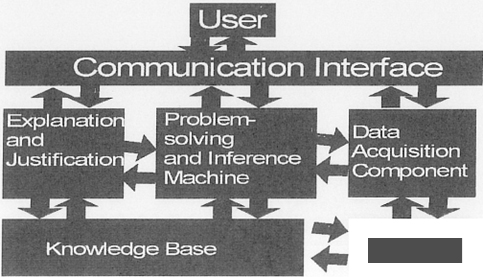
Figure 1: Components of an expert system
Medical Diagnostics/ Therapeutics
Many of the early expert systems, like MYCIN and CADUCEUS, were developed for medical diagnostic or therapeutic purposes. Most of these systems are rule-based expert systems. 1Work, however, has progressed on artificial neural networks (ANNs). ANNs systems are more adaptive and less constrained by fixed rules. The development of digital imagery systems in areas such as computerised tomography magnetic resonance imaging (MRI) and ultrasonography has allowed the creation of digital images which can easily be manipulated by computers for consideration by ANN-based expert systems. Such expert systems have proved to be useful in image classification and have been applied with limited success to diagnostic pattern recognition in MRI, nuclear medicine and chest radiographic images. Madsen also describes how a neural network expert system is able to recognise glaucomatous visual field changes.
Rule-based expert systems continue to have major applications in medical diagnostics and therapeutics. Figure 1 has outlined the various components of these systems. By developing these components, new expert systems are becoming more comprehensive, reliable and accurate. Knowledgebase and database development are an important aspect of these systems. Problems in this include the narrow focus, poor data quality, overabundant detail and inaccessible format of many databases to recent database development has included the utilisation of already established databases. At the Rennes University in France, the knowledge base of an expert system is incorporating the Human Immunodeficiency Virus (HIV) databases held at the University Hospital to provide a HIV diagnostic expert system. Many such large clinical databases are available. Ruffin noted that these databases are being developed by many large hospitals and healthcare companies. As such, they will be a goldmine of information for future expert systems. 12Military Hospitals like the Tripler Army Medical Centre in the United States, are also methodically developing databases of information on surgical and other procedures which could be used in future knowledge bases. 13The Australian Defence Force has large databases of medical information on its personnel which could be developed for these purposes. NASA has also investigated developing the knowledge base of the expert system. Whilst there is now ready access to electronic biomedical libraries, the medical knowledge needs to be engineered to be utilised in expert systems. The secondary databases, which incorporate knowledge abstracts, can operate to flag decisions inconsistent with established clinical treatment guidelines. NASA is presently trialing such a system in general practice. Research on improving the links between the knowledge base and database components are also being undertaken. These systems integrate diverse medical information systems, containing data and knowledge, into an expert system which allows the information to be accessed through a common interface.
Another bottleneck in expert system’s development is the knowledge acquisition subsystem. Current knowledge bases are largely manually built, a slow and tedious process16. They are also susceptible to becoming obsolete if not periodically updated. The use of automated knowledge acquisition systems allows domain experts to acquire specific knowledge, transform medical information into structured knowledge and then utilise that knowledge, all without requiring a knowledge engineer. One example is this process is the hypertext knowledge engineering system. (Disorder Toolbox) developed for the Medical Emergency Decision Assistance System (MEDAS). This enables physicians, without a computer science background, to add, manage and validate knowledge in the MEDAS without the need to recompile it. The use of such tools will open the doors to further opportunities in this area. 18Hasnah, however, warns that such systems need to be applied carefully to ensure that the new knowledge input is accurate and appropriate, that new heuristic rules applied don’t impact inappropriately on other knowledge areas, and that the storage of increasing amounts of information is catered for.
Research is also looking at the communication interface and the problem solving systems. This has led to the development of decision analysis support systems. Often embedded prompts, these interactive systems provide the cues to ensure the physician’s planned diagnostic or disease management plan are both appropriate and in line with current clinical templates. Ideally, the clinical templates are table driven to allow for rapid updating of the procedures and rules for diagnosis and treatment. Examples of these diagnostic and therapeutic decision support systems include QMR (Quick Medical Reference). Developed to the University of Pittsburgh and ILIAD, developed at the University of Utah. Ruffin, however, notes that these expert systems take considerable time for data entry, are expensive to update, and have difficulties dealing with multiple problems in one patients. Whilst the diagnostic and treatment protocols continue to improve, further research is needed on the communication interface and the unrealistic time frames for data entry. Otherwise, such systems will not make the jump from academic curiosity to a useful tool in a busy medical practice. More integrated systems like PsychAccess, which develop assessments of impairment outcome focused treatment plans and patient objectives, as well as diagnosis, are more likely to make this transition.
Diagnostic and therapeutic expert systems whilst having great potential, have major disadvantages which must be addressed before such systems enter common usage. Some of these problems like data entry and storage concerns have already been alluded to in previous paragraphs. Sumner and Shultz note that these expert systems should recognise their own limits of expertise be able to detail their logic for decisions and have the tools to target diagnostic dilemmas with specific questions. Interfacing with the computer also remains inadequate, an area which may be improved by voice recognition and virtual reality technology. The continued emphasis of expert systems on very small highly specialised medical areas, like MYCIN for microbial infections and CASNET for glaucoma, further abrogates their general use in medical practices. Larger and more comprehensive systems, like the ILIAD system, are required.16In addition, the inference engines of such programs lack the intuitive thought of human experts and compilers often underestimate the amount of non-expert information required to simulate this process.
Computerised Medical Records
The failure of the current paper-based medical record systems is well documented. Problems with legibility, inconsistency between health practices and information retrieval, limit their current and future usefulness. Expert systems, incorporated into intelligent computerised medical records have the potential to produce significant advances in this area. Detmer notes that the vision for computerised patient records (CPR) incorporates greater flexibility in the retrieval of patient data elements which distil the physician’s clinical diagnostic and therapeutic thought processes and assess their effectiveness, a distillation which has application in future expert systems. Epidemiological benefits aside, record linkage across databases provides improved prognostic knowledge to clinicians and assists in medical decision making. Indeed, the data from a standardised global electronic health record would allow the pooling of data for research and the improvement of the quality and reliability of expert systems. On a more mundane note, CPRs can remind physicians of routine and follow up visits, allow graphing of physiological variables over time, and provide advice to doctors on drug interactions, allergic problems and physiological contraindications. Proactive clinical templates embedded as interactive prompts, also enable the doctor to work through expert systems to verify diagnosis, treatment protocols and health maintenance requirements.
Quality Assurance
Expert systems also have increasing application in the areas of quality assurance and risk management within healthcare systems. Continuous quality improvement requires the development of practice guidelines and the collaboration of groups of specialists to improve clinical care. Without the common knowledge of normal clinical practice, provided by linked databases and expert systems, the effective application of guidelines is patchy at best. Gleiner predicts that Health Maintenance Organisations in the US will be soon linking their electronic medical records to clinical databases to produce a ‘best practice’ model for a specific condition. Such systems, promising high-quality medicine, will be useful as marketing tools. The National Committee for Quality Assurance in the US is developing the Health Employer Data and Information Set (HEDIS) to measure standardised health outcomes. The analysis of these outcomes will provide further information on the quality of care, patient access and patient satisfaction. On the health management side rule based and neural network expert systems are being utilised for claims adjudication (including fraud detection), utilisation reviews and identification of aberrant billing practices. Frankel Chernow and Rosenberg note that their utilisation review system was able to identify inappropriate utilisation of medical services and aberrant billing practices, profile physician practices and provide quality assurance feedback on gaps in clinical care.
Training
Medical training is an area that will be increasingly impacted by the application of expert systems. Increasingly, interactive medical computer systems are being used in medical schools to train students in diagnosis and the therapeutics while some medical schools, like the University of Michigan, are teaching students Applied Medical Informatics.31The advantages of computer interactive learning include immediate student-specific feedback, tailored instructional programs, objective testing of progress and an entertaining format. Expert systems, like GUIDON use a set of teaching strategy rules to develop new interactive applications. Computer-assisted instruction so developed can form the basis of a comprehensive system for lifelong education.
Post-graduate medical training can also benefit from the use of expert systems. Virtual reality systems, which generate environmental representations that allow sensory interaction, can be used to simulate the body for the purposes of anatomical study and minimally invasive, particularly laparoscopic, surgery. Practice critiquing systems have also been developed. These include ATTENDING and HTATTENDING which critique anaesthetic management and hypertensive management respectively.
Application to Military Medicine
The military medical community, particularly in Australia has yet to embrace and apply the advances being made in medical expert systems. At HMAS STIRLING, the only medical computer support system is KERMIT, a Navy specific health record and medical administration support system. Whilst the system has some primitive recall programs, the system has no expert capabilities. The MIMS prescription system is in the process of being introduced. This has some embedded prompts which will interactively question possible adverse reactions, drug interactions and allergies. On the horizon is the Health Systems Redevelopment Project (HSRP). This eight-year project, which is finally undergoing pilot system trials in Canberra. Aims to introduce interactive computer-based medical records across the Australian Defence Force (ADF). Within this computer network framework, there will be scope for diagnostic and therapeutic expert systems, computer-assisted training. epidemiological research and quality assurance programs. As the ADF is a controlled health maintenance organisation the ‘future picture of quality medicine’ with integrated registration, problem-oriented medical records, clinical templates, disease management cues and internal messaging, as espoused by Lowenstein and Greenberg, 19is becoming increasingly likely with HSRP. There are, however, many challenges still to be met. The diverse nature of medical knowledge, the lack of objective gold standards subjective variations in medical practice, preconceived ideas of what a doctor is, and poor physician acceptance, will all contribute to the successful (or otherwise) use of artificial intelligence in medicine.
Conclusion
Medical practice has utilised expert systems since the early days of artificial intelligence research. In this paper, the role of such systems in diagnosis, therapy, quality assurance, medical records and training have been reviewed. The benefits of such systems in producing more productive and effective medical workplaces have yet to be fully realised. The future, however, of such medical expert systems remains promising for both civilian and military practice. To quote Marshall Ruffin 35 one of their greatest advocates ‘the future is here’.






