Abstract
The aim of the article is to discuss the importance of providing adequate health advice and support to troops deploying within Australia away from base areas. This was developed through a briefing of a unit exposed to Ross River Virus (RRV) within SouthEast Queensland. The results of an epidemiological study conducted to investigate the above will be highlighted and the effects on the members involved, their unit and our understanding of the disease itself will be discussed. Recommendations in regard to ongoing basic health maintenance advice, preventative health refresher training and ongoing disease surveillance within Australia will conclude the article.
Introduction
Ross River Virus (RRV) is a mosquito borne Arbovirus active within Australia and areas of Australian strategic interest. The disease infects thousands of Australians a year, with economic effects through loss of man-hours and productivity amounting to millions of dollars. The latest Notifiable Disease statistics for Queensland (April 1999) report a seasonal pattern of notifications (Jan-Jun with peaks in March) with 1638 notifications reported for the year to date (2071 mean year to date 94-98).
Defence personnel are likely to be at a greater risk in some areas than the general community. They find themselves deployed in areas of risk, operating in environments representative of the vector’s natural habitat. Troop concentrations facilitate the transmission of the virus between personnel. There is an associated risk that troops returning to home base areas can translocate the disease to new areas where the right conditions may exist for the disease to present as a short term problem, if not endemic.
Also known as Epidemic Polyarthritis, the disease is transmitted by a number of mosquito vectors via native animal hosts. Endemic in the Shoalwater Bay Training Area (SWBTA), Townsville and South Eastern Queensland, the disease causes symptoms ranging from a transient rash and flu-like illness to headaches, fevers and mild to severe polyarthritis. This last feature of severe joint pain has given its common name, and represents the most debilitating factor.
As the symptoms of RRV are similar to a number of other diseases, blood serum testing is needed for infection with RRV to be confirmed. The presence of IgM acutely after onset of symptoms should be noted, followed (usually within 10 days) by rising titres of IgG. As false positive IgM results are possible, it is necessary that IgG be identified before confirmation of infection can be made.
Background
During the period 18-28 March 1999, 169 mixed military and civilian contract personnel deployed to Tara, South-East Queensland for a 10 day exercise. In the weeks following their return, 3 members presented with debilitating illness and were found to be IgM positive RRV on investigative serology. Following discussion with the Army Malaria Institute (AMI) as to the extent that the disease may have infected the subject group as a whole, it was proposed that a study be conducted to establish the features of the exposure. This would assist understanding the disease as relatively little is known in this area of epidemiology.
Significance
Exposure of a sub-group was clinically suspected, but it was believed that an unknown additional sub-group was infected but only mildly symptomatic or asymptomatic. These cases should be IgM positive, but may not have presented for treatment or went unrecognised due to only minor symptom complaints.
AMI advised that the Clinical to Subclinical disease ratio in this type of population was as yet unclear and that, from a military health point of view, there was significant research value in investigating this group. Locally, we were also interested in whether preventative measures taken against mosquito borne infection by the troops in the field had any relationship to the final epidemiological findings.
Conduct
A serological study was conducted under an ethics committee approved AMI standing protocol for Arbovirus Surveillance. A questionnaire tool was developed in order to obtain information relating to the exercise, possible previous RRV exposure, use of preventative measures and post-exercise illness.
Volunteers from members of the unit (and other similar local units) who did not attend the exercise were encouraged in order to provide control subjects and to assess the baseline RRV IgG status of the resident population.
A briefing was conducted 20 May 99 before a unit administration parade, and volunteers were called for. 100 members subsequently presented for enrolment, with questionnaires completed and blood samples taken later that day within the unit area. Volunteer attendance was facilitated through a coordinated release from normal workplace duties on a section by section basis.
Members were greeted on presentation to the study area, and questionnaires were provided for completion. Personal regimental details were recorded separate to questionnaires, with non-identifying sequential numbers issued to ensure privacy. As the privacy number was the only means of tying questionnaires and blood samples to individual members, the study coordinator secured the personal records as per ethical research guidelines.
| Subjects | No | Age (in years) | Height (in cm) | Weight (in kg) | Sex (M,F ) |
|---|---|---|---|---|---|
| Exercise | 67 | 28.7 (19-45) | 176.7 (160-193) | 83.1 (46-112) | 59, 8 |
| Non-Exercise | 33 | 33 (22-58) | 177.1 (155-193) | 79.7 (51-117) | 27, 6 |
Demographics
Of the 169 members who deployed to the exercise area, 39.6% (67) volunteered for enrolment in the study. 33 additional members from the unit, and other local units, were enrolled to participate as control subjects, to total 100 samples. Demographic data for the volunteers is at Table 1.
Duration of Exposure
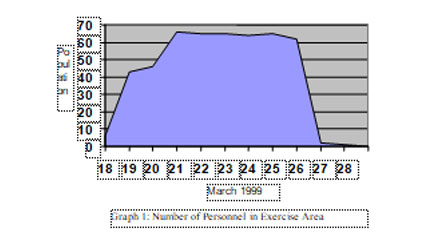
Participants were asked to note the dates during which they were in the exercise area. All exercise participants identified deployment to the area within the 11 day period 18-28 March 1999, with peak occupancy of the area occurring 21-26 March 1999. 52.2% (35) of the participants reported being in the area for 8 days. The number of personnel in the exercise area (by date) is illustrated at Graph 1.
Previous Exposure
Members were asked whether they believed they had been previously exposed, or diagnosed with RRV, and if so, when and where. 13.4% (9) of those who attended the exercise and 30.3% (10) of the control subjects reported possible previous exposure.
In nominating where they believed they were previously at risk of exposure, the following areas were identified per Table 2.
| Area/s Nominated | Responses |
|---|---|
| Townsville | 7 |
| Darwin | 1 |
| Townsville/Tully/NT | 1 |
| Townsville/SWBTA | 2 |
| SWBTA | 3 |
| Murray River | 1 |
| Not identified | 3 |
| At risk everywhere | 1 |
Preventative Measures
Volunteers were asked to address a series of questions regarding their awareness, prior to deployment, of a risk of mosquito-borne disease within the training area, and what measures, if any, were taken with regard to the risk.
40.3% (27) reported they believed there was a risk of disease in the training area prior to deployment. 89.6% (60) reported using one or more mosquito avoidance measures, e.g. sleeves down, netting at night, or clothes dipping.
97% (65) reported using a topical repellent. Responses indicated a variety of brands and frequency of use. Nominated brands are at Table 3.
| Brand | Responses |
|---|---|
| Army Issue | 12 |
| Rid | 17 |
| Skintastic | 2 |
| Aeroguard | 4 |
| Bushmans’ | 5 |
| Combination/multiple brands | 13 |
| Not identified by brand | 2 |
46.3% (31) reported attendance at preventative health briefings prior to deployment. In answering whether other preventative health measures were offered prior to deployment, 40.3% (27) indicated that additional training or resources were made available e.g. repellent, netting.
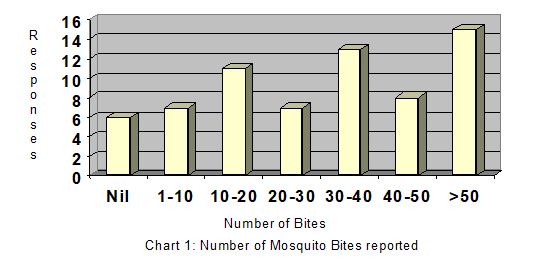
Mosquito Exposure
Symptoms and Treatment
| Responses | Number | % |
|---|---|---|
| Rash | 4 | 5.9 |
| Unwell | 30 | 44.8 |
| Headaches | 28 | 41.8 |
| Fever | 10 | 14.9 |
| Joint pains/aches | 18 | 26.9 |
| Sought medical opinion | 9 | 13.4 |
| If not, self-treated | 19 | 28.4 |
Members who had attended the exercise were asked whether they recalled having suffered any of the common symptoms of RRV infection. Over half (62.6%) reported having at least one symptom, the most common being feeling “unwell”, with headaches also featuring. The results of the Symptoms and Treatment sought section of the questionnaire are at Table 4.
14 members reported having suffered only one symptom. An additional 14 members recalled having 2 of the listed symptoms, most commonly a combination of feeling unwell with either headache or joint pain. The results from this section are at Table 5 below.
| No. | Rash | Unwell | Headaches | Fever | Joint pains/aches |
|---|---|---|---|---|---|
| 1 | 6 | 6 | 2 | ||
| 2 | 1 | 10 | 10 | 2 | 5 |
| 3 | 2 | 9 | 7 | 3 | 6 |
| 4 | 4 | 4 | 4 | 4 | |
| 5 | 1 | 1 | 1 | 1 | 1 |
9 members presented for medical opinion, reporting from 1 (felt unwell only) to all 5 of the listed symptoms. Of this group, the most common complaint was feeling unwell (8), with joint pain (7) the next most common symptom. Of the self-treatment group (19), a variety (and combinations) of relief measures were reported as per Table 6 below.
| Treatment | Number |
|---|---|
| Sleep/wait/rest/untreated | 8 |
| Paracetamol | 13 |
| Aspirin | 2 |
| Cold and flu preparation | 1 |
| Antihistamine | 1 |
| Multivitamins/mineral supplement | 1 |
| Topical cream for rash | 1 |
The reasons given by members who did not seek treatment varied from having only minor symptoms, to them not recognising possible infection and ascribing symptoms to other causes such as training injuries (aching joints) or over-work (lethargy).
Results of Serology
23% (23) of the 100 combined samples were found to be IgG positive for RRV; 16 from the exercise group and 7 from the control group.
This represents 23.8% of the exercise subjects and 21.2% of control group. Two samples were found to be IgM positive for RRV, and another sample was found to be both IgG and IgM positive for Barmah Forest Virus, all from the exercise group.
9 subjects from the exercise indicated that they believed they had been previously exposed to RRV. Only 2 were found to be IgG positive, with 1 of these also IgM positive. Of the 10 control subjects who indicated possible previous exposure, 2 were found IgG positive. The remaining 19 IgG positive results (14 exercise and 5 control subjects) had not indicated suspicion of previous exposure.
Of the 9 study members who reported for medical opinion, 2 were found to be IgG positive. Both reported feeling unwell with headaches and joint pain, with one also reporting fever. The member who presented for treatment and reported having all 5 of the
Summaries of IgM Positive Cases
| RRV Case 1 |
|
| RRV Case 2 |
|
| BFV |
|
Summary of Overall Results
Including the initial clinical cases who prompted the study, 5 members were found IgM and IgG positive for RRV (2.9% of total on exercise). There were also 2 members found IgM and IgG positive for BFV (1.1% of total on exercise). Most were from the Advance Party that arrived several days prior to the majority of the respondents. Feedback from members of this group indicates that their reports of copious mosquitoes reinforced the need for preventative health briefings. Symptoms experienced by these members to various degrees included polyarthralgia, especially in wrists and ankles, general malaise, lethargy and headaches. These correlate to the disease symptoms reported by Flexman et al in 1998. An erythematous maculopapular rash with vesicular features was also reported one of the BFV cases, again correlating with the known disease features.
The sole member who reported having all of the listed symptoms, and reported for medical opinion, was found not to be IgM or IgG positive. This is indicative of the difficulties of interpreting and diagnosing RRV infection based on clinical signs and single sample serology alone.
Value in taking Preventative Health Measures
Had the Advance Party not recognised the mosquito risk to health within the exercise area would there have been as much emphasis, if any, on preventative health preparation for this exercise? The effects upon the manpower of this unit were minimised by the reported widespread application of topical mosquito repellent and other preventative measures. For the members who presented with clinical illness symptoms, significant periods of disability through being either unfit and/or on restricted duty, not to mention personal discomfort, were experienced. Flexman et al. note that over 50% of patients still complain of joint pains up to a year after onset, with an additional group suffering lesser symptoms for a similarly long time. 1 Relapses may also occur in subsequent years. Significant cumulative effects on unit productivity and personal morale and fitness could accrue from widespread infection within a military population.
Health briefings provided before deployment appear in this study to have shown their worth. The survey reports a high percentage use of netting, sleeves down, topical insect repellent etc, as well as a high degree of awareness of the risk pre-deployment thanks to preventative health briefings. A conclusion that could be drawn from this is that pre-deployment health briefings and the use of preventative measures in the field worked to restrict exposure to this form of disease risk.
Problems with the study
The fundamental problem, for military and civilian epidemiologists alike is that RRV IgM persistence remains essentially unknown, but possibly quite long term. As is the case for other virus infections, IgM antibody resulting from RRV infection may persist anywhere from months to years. This makes interpretation of possible acute infection from a single serum sample unreliable, even in the presence of clinical illness symptoms. Most of us have antibodies to measles, polioviruses, mumps, etc. but we are not now ill with those viruses, and it is possible that symptoms experienced at any given time are produced by an illness unrelated to the antibody status. This also makes any attempts at correlation to a single event or location difficult.
A 1993 paper by Mackenzie et al, published in Australian Communicable Diseases Intelligence, advised that paired acute and convalescent-phase serum samples are required in order to make a confirmed diagnosis.2 Tests of single serum samples, at best, can only be used to make presumptive diagnoses. Flexman et al. also noted the changes needed in IgG titres for a confirmed diagnosis to be made.1 Reports of false positive IgM responses also limit the confidence in single sample test regimes.
The cases identified by this study are single sample IgM and IgG positives only. The combination of both IgM and IgG antibodies found suggests that infection may very well have occurred in those cases, but the question remains as to when. Serum samples taken within the acute illness phase would have been useful, with pre-deployment baseline samples providing even further data for interpretation. With the additional data, confirmed acute cases could have been sorted from those found to be representing only remote infections with RRV associated with clinically similar illnesses.
For accurate surveillance of the disease, each presentation needs to be associated with an illness as well as with a significant rise or fall in antibody titre. Paired acute and convalescence phase serum samples need to be taken to enable confirmation of acute disease. Until RRV and other virus infections reported to authorities are limited to those confirmed by the methodology outlined by the references, the epidemiological challenges will remain difficult to tackle.
Given the unknown persistence of both IgG and IgM, it is difficult to identify the optimal period for this study to have been conducted. It is believed that there may have been subjects who had been exposed during the exercise, who underwent only a minor
immunological response with a correspondingly minimal production of IgM resulting. The references suggest however that as IgM is currently suspected to have a prolonged persistence, this is considered less likely than was suspected before the study, although further research into such cases is recommended. For those members found to be IgG positive, it is again impossible to draw any conclusions on possible time of infection.
In relation to the Questionnaire tool, the questions were far too subjective, with no definitions given for such broad terms as ‘feeling unwell’ and ‘fever’. The time available and scope of this study limited the depth of inquiry, making such terminology necessary.
Members were also relied upon to recall details of interest, such as number of insect bites suffered, 8 weeks post-exercise. The findings cannot be relied upon to the same extent as results that could be gained from having members keep a diary, or similar record, of events of interest during a period for investigation.
The matching of the demographics of the control volunteers to the exercise subjects was imperfect, with control volunteers being on average 4.3 years older, as can be seen in the results at Table 1. It was desirable that members of similar age, rank, field experience and employment be enrolled in order for a number of possible correlations to be drawn. The volunteers who presented however tended to be more senior members of the base workshop staff, or similar. As a group, they could have been expected to have had spent more time deployed in the field during their career than those on exercise, with a relative IgG result found. Perhaps of some significance is that they were found to have a slightly lower incidence of IgG – 21.2% positive against 23.8% for the exercise group.
Recommendations
When planning for overseas deployment, the need for accurate health intelligence and the provision of prophylactic measures is recognised to be of significant importance. During peacetime when deploying on exercise within Australia, it is possible that such considerations as endemic disease within an exercise area are not considered, given our generally benign surroundings. Exercise planners and reconnaissance/advance parties need to consider the possibility of environmental disease risks when looking at an area of future interest. Public health authorities and local medical officers are able to provide information about possible hazards within their area, allowing plans for preventative health measures to be based on local knowledge.
The findings of this study suggest that basic preventative health measures limit the risk of exposure and infection from environmental hazards. Regular refresher lessons and appropriate health briefings/preparation before deployments can assist a unit to remain fully functional by negating these hazards.
Of interest from this study is the number of different types/brands of topical insect repellent reported to have been used. Given the wide variance in the content of active ingredient (DEET) in the nominated products, further analysis of the bites/topical repellent relationship could be of interest. As the army issue solution can be demonstrated to have a cost-benefit advantage (free and effective), units should ensure that all members deploying to the field are encouraged to use, and have adequate supplies, of the inservice solution.
Timely post-exercise surveillance and follow-up of reported notifiable disease, including paired acute and convalescence phase serum sampling, is vital if understanding of disease risks is to be advanced. From initial discussions prior to this study, it was apparent that there is still much to yet be determined about Ross River Virus disease. Further research into the Clinical/Subclinical Infection Ratio, IgG/IgM serum persistence and interpretation, and disease prevention is required before forces can be assured that the risk is well understood.


