Abstract
Background: The Royal Australian Air Force’s Health Services Wing (HSW) continually seeks to improve the training and credentialing of medical officers in order to provide a high-quality healthcare capability. The CAMMO Project aims to inform an evidence-based approach to the training and credentialling of General Duties Medical Officers (GDMOs).
Purpose: Stage 2 of the CAMMO project is a scoping review of the medical literature on the acquisition and maintenance of the critical care skills GDMOs may require to be proficient in, as identified in Stage 1 of the project.
Method: A systematic search of the medical literature was conducted, and data pertaining to the acquisition and maintenance of the identified critical care skills was analysed.
Results: A total of 2401 titles and abstracts were screened, identifying 21 studies that were appropriate for analysis.
Conclusion: Based on the literature search results, there is limited relevant literature available to guide the learning curve and appropriate skill maintenance intervals for many critical care skills. However, there is a sufficient literature base in other areas to provide some guidance. Literature on the rate of skill degradation and recommended retraining intervals may have particular relevance to RAAF, where deployment length must be considered.
Introduction
The Critical-skills Acquisition and Maintenance in Medical Officers (CAMMO) Project is an initiative of Headquarters HSW seeking to inform appropriate training and credentialing of General Duties Medical Officers (GDMOs) expected to perform critical care skills. It is one of projects currently being undertaken by HSW and the wider defence force attempting to optimise medical officer training. Stage 1 of this project identified a list of critical care skills that GDMOs may be required to be proficient in (Figure 1). Stage 2 of the CAMMO project involves a systematic review of the medical literature to define the training requirements for proficiency in those skills, and the retraining requirements for maintaining proficiency. Stage 3 intends to explore and recommend alternative systems for training and credentialing of GDMOs based on the findings in Stage 2.
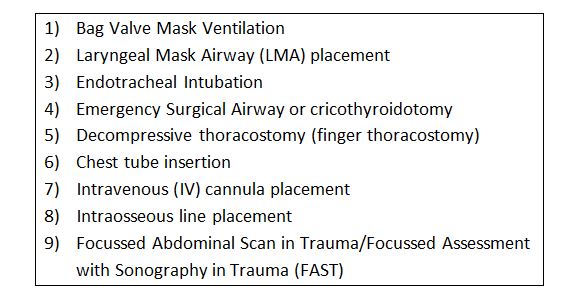
Figure 1: List of Critical Care skills identified in CAMMO Stage 11
Methods
A systematic search of the CINAHL and MEDLINE databases utilising the CKN platform was conducted in May 2016 and repeated in August 2021. Search terms were used for each critical care skill listed in Figure 1, including equivalent terms, combined with terms relating to skill acquisition and maintenance (e.g. ‘“Laryngeal Mask Airway’” OR ‘“LMA’” OR ‘“Supraglottic Device’” AND ‘“skill acquisition’” OR ‘“skill maintenance’” OR ‘“learning curve”’ OR competence OR CUMSUM). To broaden the search, reference lists of all included articles were reviewed for other potential studies to include. Of the 2401 titles and abstracts screened, 10 were not available in English, and a further 2332 were irrelevant to the critical care skill, skill acquisition or maintenance. Full texts of the remaining studies were evaluated, and the following exclusion criteria were applied:
- No objective measure utilised to measure skill acquisition or maintenance
- Evaluating a proprietary product, rather than a skill.
Fifty-nine papers were assessed for eligibility, with 21 included in this review (see Figure 2). Relevant information from included articles was organised according to the critical care skill and presented in results.
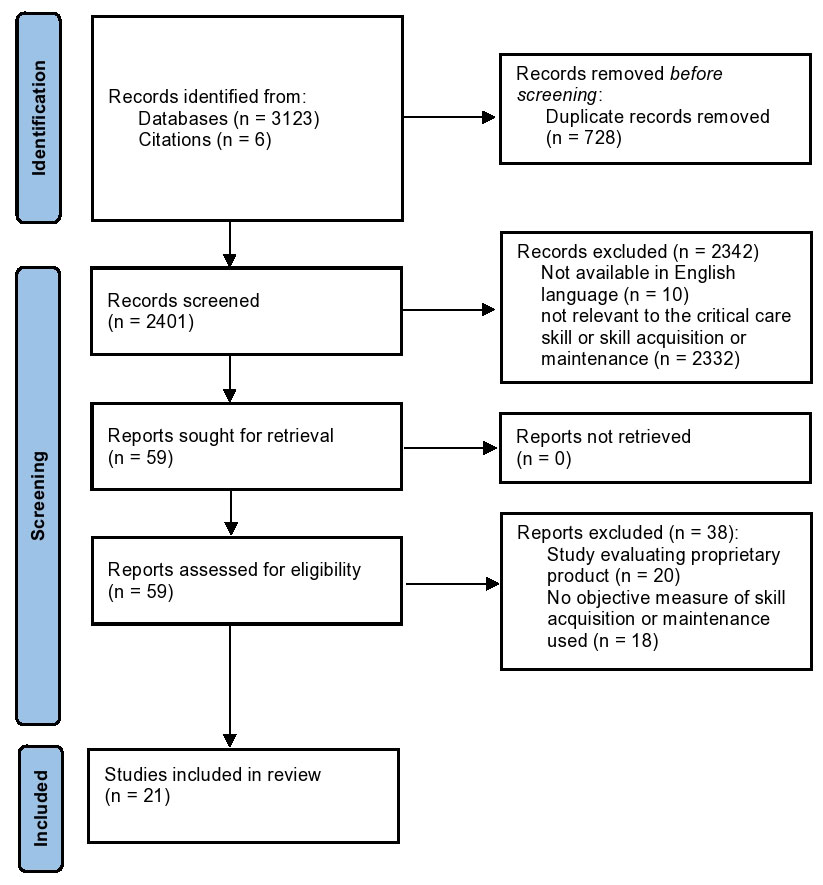
Figure 2: Flow Diagram of study selection.
Results
Table 1 shows the results of the systematic literature search, organised tofor the critical care skill evaluated. A wide variation in the volumes of available literature was identified across the different skills, with the highest number of search results, and ultimately relevant articles, found for Endotracheal Intubation (ETI) at 1677 and 7, respectively. Decompressive/finger thoracostomy failed to identify any relevant studies.
Table 1: Results of the systematic literature search according to critical care skill
| Critical care skill | Total identified in search | Not available in English | Not relevant to critical care skill | Testing a proprietary product | Doesn’t objectively measure skill acquisition or maintenance | Included |
|---|---|---|---|---|---|---|
| BVM ventilation | 33 | 0 | 32 | 0 | 0 | 1a |
| LMA placement | 209 | 0 | 190 | 15 | 0 | 4 |
| ETI | 1677b | 6 | 1661 | 0 | 3b | 7a |
| Cricothyroidotomy | 158 | 1 | 144 | 4 | 4 | 5 |
| Decompressive thoracostomy | 0 | 0 | ||||
| Chest tube insertion | 183 | 1 | 178 | 0 | 4 | 0 |
| IV cannula placement | 8 | 0 | 3 | 0 | 3 | 2 |
| IO placement | 109 | 2 | 103 | 1 | 0 | 3 |
| FAST | 24 | 0 | 20 | 0 | 4 | 0 |
b Include 1 article identified from review of reference lists
Skill acquisition
Several relevant studies were identified pertaining to skill acquisition in LMA placement, ETI , emergency surgical airway/cricothyroidotomy, IV cannula placement and intraosseous line placement. The data from these is displayed in tables 2–-6. In addition, Buis et al.2 authored a 2015 systematic review defining the learning curve of ETI using direct laryngoscopy, which included 13 articles (including Toda et al. in Table 3). They concluded 51-–75 cases were required to reach a success rate of >80% with a single attempt, 1-–43 cases were required to reach >80% success with two attempts, At least 50 cases were required to reach a >90% success rate with two attempts. The authors also noted that the learning curve in the prehospital setting was much steeper and did not plateau as quickly (>30 attempts to plateau prehospital vs 20-–25 in the elective setting). Some studies utilised CUSUM (cumulative summation) and LC-CUSUM (learning curve – -cumulative summation). CUSUM and LC-CUSUM are statistical tools designed to track competence in a procedure. Participants log their attempts and successes, and algorithms are used to determine the adequacy of performance. They differ in that CUSUM considers successive successes and failures, and that successive failures may cause the participant’s performance to be deemed inadequate. It detects a deviation in performance from adequate to inadequate and places a greater emphasis on failures. In LC-CUMSUM, successive failures cannot cause a participant’s performance to rise above 0 (defined as inadequate performance), thus placing less emphasis on the series of failures that may occur when a new skill is being learnt.3
Table 2: Skill acquisition in Laryngeal Mask Airway (LMA) placement
| Study | Setting | Cohort | Parameters | Outcome |
|---|---|---|---|---|
| Mohr et al.4 | German hospital, operating theatres | Ten anaesthesiology residents at the beginning of their training, undertaking their first 40 LMA insertions | Success defined as ability to ventilate through LMA. Number of attempts to success documented. Attempts were divided into groups of five consecutive placements for analysis. | Participants showed a statistically significant improvement in the number of attempts required for success between the first five (1.45±0.82) and after 40 (1.16±0.37, p <.03). However, there was no difference between the first five and the rest on average, suggesting quite a flat learning curve. |
| Lopez-Gil et al.5 | Paediatric hospital operating department. Residents underwent didactic training in placement of LMA in children, followed by demonstration during an operative case. Participants were supervised by and received feedback from consultant anaesthetists. | Eight third-year anaesthesia residents with no prior experience in LMA placement. Initially 10 participants, but two failed to complete the required number of cases. | Participants were supervised in LMA placements in 75 cases each that were deemed acceptable based on aspiration risk, likely airway pressures required and surgical factors. Complications for each attempt were recorded. Analysis was based on grouping attempts chronologically into five series of 15 attempts each. | A total of 189 complications occurred in 121 children. There was a significant decrease in complication rates between each period of training from 62% in the first series of 15 to 2% in the final series. |
| Hein et al.6 | Australian skills development laboratory utilising part task trainers (PTTs) | Fifty-five first-year paramedic trainees with no prior LMA placement experience. | Participants were shown an instructional video and underwent guided practice with four attempts each on three different PTTs (total 12 attempts). Success was defined by ability to ventilate the PTT. Success and time to success were recorded. | PTT 1—Success improved from 34/55 participants in attempt 1 to 55/55 in attempt four with mean insertion time dropping form 54.3 sec to 26.8sec; PTT 2—success improved from 41/55 at attempt one to 51/55 in attempt four with mean insertion time improving from 44.1–27.6 sec; PTT 3—there was no statistically significant improvement in success (55/55 to 55/55) but an improvement in mean insertion time 24.9 to 20.2 sec from attempt one to four. |
Table 3: Skill acquisition in Endotracheal Intubation (ETI)
| Study | Setting | Cohort | Parameters | Outcome |
|---|---|---|---|---|
| Ishizuka et al.7 | Paediatric patients, in hospital but outside the operating theatre | 10 Paediatric Fellows | CUSUM analysis. Acceptable standard defined as >90% success rate with unlimited attempts | 39–60 intubations required to reach standard. |
| Young, A et al.8 | Operating theatre in Madigan Army Medical Centre, Tacoma, Washington | 11 PGY 1 surgical residents. Supervised by consultant anaesthetists. | CUSUM analysis, >95% success rate (correct placement, confirmed by capnography within 30 sec) | Determined it takes 19 attempts to get off the learning curve (i.e., starting to have a series of successes). However, >95% success rate not reached by any candidates (21–37 attempts each). |
| Toda et al.9 | Operating theatre on ASA 1 or two patients. | 32 Paramedics following a training course. | Observational study. No predetermined success rate defined. Up to 2 attempts allowed per patient. | <13 intubations led to no improvement. 87% Success rate was reached after 30 attempts |
| Je et al.10 | Two Urban Emergency Medicine Departments in the USA. | Three emergency medicine residents in their first 2 years of residency in a hospital in the USA. | LC-CUSUM. Adequate performance >90% success rate, inadequate performance <80% success. Two attempts allowed per patient, no immediate complications allowed. | A total of 342 intubations were recorded. A mean number of cases to adequacy was 74.7 (95% CI of 62.0-87.3). 80% success rate reached after mean of 30 cases. |
| Ospina et al.11 | Operating theatres, Columbia | Four anaesthetics trainees | CUSUM, >95% success rate within two attempts per patient | Trainees each required a different number of cases: 41, 55, 83 and 152 to reach the determined success rate. |
| Kim et al.12 | Observational study in emergency department resuscitation rooms in single centre in Seoul, South Korea. Patients in cardiac arrest over 2 years. | 11 emergency medicine trainees. 110 intubation experiences included in the study. | Cohort divided into five groups according to their experience in ETI. Qualified success defined as ETI within 60 sec without complication. Highly-qualified success defined as ETI within 30 sec without complications. Other parameters measured included first pass success, oesophageal intubation, endo-bronchial intubation and time of interrupted chest compressions. | The most experienced group (Q5) had a mean of 103 previous intubation experiences, compared with 26 in the least experienced (Q1). First pass success was 81.8% in Q5 compared with 36.4% in Q1 (P = 0.004). Qualified success improved from 13.6% in Q1 to 63.6% in Q5 (P = 0.020). Highly-qualified success was 0% in Q1 and 31.8% in Q5 (P = 0.002). A linear regression analysis estimated a rate of 80% qualified success required 137 ETI experiences and 90% qualified success required 157 ETI experiences. For highly-qualified success in 80% of cases 220 ETI experiences would be required and 243 for 90% highly-qualified success. |
Table 4: Skill acquisition in emergency surgical airway/cricothyroidotomy
| Study | Setting | Cohort | Parameters | Outcome |
|---|---|---|---|---|
| Wong et al.13 | Airway model used, no equipment set-up required, time and success were recorded over 10 successive attempts, utilised percutaneous dilating cricothyroidotomy set (Seldinger technique). | One hundred and two anaesthetists | Success defined as <40 sec to successful cricothyroidotomy. | Improvement in time plateaued after four attempts, from a mean time of 41 sec to 30 sec. Improvements in success plateaued after five attempts, with a success rate of 96%. |
| Buopane et al.14 | Air way model used, Following a 1-day training session participants were timed to successful cricothyroidotomy using either a Melker or QuickTrach set, over five successive attempts | Forty volunteers including anaesthetists, residents, paramedics and nurses | No explicit definition of successful cricothyroidotomy given. | Statistically significant improvement in mean time to cricothyroidotomy between the first (48.7 sec) and fifth (27.8 sec) attempts. No significant difference between the fourth and fifth attempts. |
| Shetty et al.15 | Designed to mirror the method of Wong et al. Airway model used, equipment for Seldinger technique (Melker). Participants provided with study materials and demonstration. Time to successful insertion was recorded for five successive attempts. | Thirty volunteers with varying levels of medical experience (resident to specialist). | Success defined as <60sec to successful cricothyroidotomy. Time from skin preparation to lung inflation. | Statistically significant improvement in insertion times seen across all five attempts. Mean time for initial attempt was 62.1 sec and 39.1 sec for the fifth attempt. The rate of improvement decreased across the attempts from -23.0sec between attempts 1 and 2 and -6.1sec between attempts four and five (P < 0.001). |
Table 5: Skill acquisition in intravenous cannula placement
| Study | Setting | Cohort | Parameters | Outcome |
|---|---|---|---|---|
| Murgatroyd & Jones3 | Single teaching hospital in UK; real patients, supervised practice | Ten medical students | Successful IV cannulation with a single puncture of the skin. CUSUM and LC-CUSUM were used. Acceptable failure rate was defined as 20% and unacceptable as 40%. | Students had between 50 and 65 attempts each. Using CUSUM analysis five did not meet the threshold, the average number of attempts to reach the threshold was 41. Using LC-CUSUM all participants reached an acceptable level of competence with an average of 25 attempts required. |
| Ault et al.22 | Single hospital in USA. Nursing staff underwent a didactic and practical training program utilising mannequins to teach peripheral IV using ultrasound prior to being allowed to utilise the skills on real patients. | Eight nurses selected to undergo training in ultrasound guided peripheral IV, based on experience in cannulation and lack of experience with ultrasound | Allowed up to three attempts at two sites. Successful cannulation defined by the ability to aspirate blood and flush saline using the cannula. Patients were selected based on previous requirement for the use of ultrasound for cannulation or a lack of visible or palpable veins. | Seven out of eight participants completed training. Average number of encounters required for 10 successful IV cannulations was 25 with a range of 18–30. |
Table 6: Skill Acquisition in Intraosseous placement
| Study | Setting | Cohort | Parameters | Outcome |
|---|---|---|---|---|
| Ong et al23 | Simulation using a bone model and the EZ-IO device. Training provided on the device using the same model prior to the study attempt. | 25 medical students, nurses and physicians with no previous experience using the device. | Allowed multiple attempts to gain successful IO access. However, success was not explicitly defined. | 23 of the 25 (92%) participants successfully gained IO access in the first attempt. Overall 24 of 25 successfully gained IO access with a mean time of 13.9 sec. |
| Polat & Oguz24 | Cadavers used in hospital in Turkey. EZ-IO device used. A demonstration of the use of the device was given prior to the participants’ attempts. | 50 interns from a single hospital, with no previous experience in gaining IO access. | Participants attempted insertion of the IO in 10 cadavers tibias. Time to success and success rate recorded. | Significant decrease in the time required to gain IO access at each attempt between the first and eighth attempts, with a reduction in mean time from 84.64 secs to 39.48 secs. No significant improvement in the time to gaining access in subsequent attempts. Authors suggest that the first three to four attempts at gaining IO access should be supervised. |
| Levitan et al.25 | Cadaver study in American Hospital. EZ-IO device used. A 5-minute presentation including one demonstration on the use of the device. | 99 practitioners (42 emergency medicine consultants, 13 other physicians, 31 emergency trainees, 13 non-physicians) | Participants were allowed three tibial insertions on cadavers following training. Success was defined as insertion with stable bone position without extravasation of fluid. | Success at first, second and third attempts was 96.9%, 94.9% and 100% respectively. Median insertion time was 6 sec. |
Skill maintenance
A limited number of papers relating to skill maintenance of critical care procedures were identified. These were primarily related to LMA placement and emergency surgical airway/cricothyroidotomy.
Ander et al.16 studied a cohort of 39 emergency medicine residents in a single centre in the USA. They were trained on the insertion of LMAs, Fastrach intubating LMA and the Combitube and tested on the time taken to insert the three devices in a mannequin successfully They were then retested 6 and 12 months later. The ventilation of the mannequin defined success. Their study demonstrated a small, statistically significant increase in individuals’ time to ventilation using the LMA (3.3 sec, 95% CI 2.67–-4.33 sec) and Combitube (2.9 sec, 95% CI 0.33–-5.0 sec) over the study period and a small decrease in the Fastrach insertion time (-3.3 sec, 95% CI -6.27 to -0.32 sec). The authors suggest that this demonstrates retention in skills using a rescue airway device at 12 months.
Hein et al.6 split the original cohort of 55 paramedic students (described in Table 2) into two cohorts and tested their skill retention at 6 months. Those with interval experience in LMA placement were excluded. One cohort underwent retraining (similar to the initial training) before undertaking a scenario, and the control group had no retraining. Both groups showed a significant increase (P < 0.05) in time to successful ventilation compared with the end of their initial training. The intervention group was significantly faster than the control group (94sec vs 209sec; P = 0.029).
Boet et al.17 studied the skill retention of cricothyroidotomy using the Melker kit. Thirty-four anaesthetists were trained on how to use the kit using mannequins. They were tested following the training and then at 6 or 12 months, depending on randomisation. The study showed no significant drop in performance at the 6 or 12 month test in either group (P < 0.05).
However, participants were tested against their own standard and were not made to achieve a defined standard. It also showed a greater, although still not significant, drop in performance at 6 months compared to 12 months, which leads to some questions regarding validity.
Kuduvalli et al.18 performed a similar study on 25 anaesthetists using simulations of a ‘“can’t intubate can ventilate (CI)’” and a ‘“can’t intubate can’t ventilate (CICV)’” scenario. They were tested at either –6-8 weeks or 6–-8 months after the initial scenario, and assessed for adherence to the Difficult Airways Society (DAS) guidelines. In the CI scenario, there was a decrease in deviation from the DAS guidelines in both follow- up groups. There was a statistically significant increase in the mean time taken to place an LMA in the 6–-8 month follow-up group (P < 0.05), compared to their initial testing. Such a degradation was not seen in the 6-–8 week group. In the CICV scenario, both follow-up groups maintained a significant decrease in deviation from the DAS guidelines (P < 0.01). An initial improvement in the time taken to effective jet ventilation was seen in the 6-–8 week group (P < 0.05);, however, it was not maintained in the 6–-8 month group. There was a significantly longer period of oxygen desaturation in the 6–-8 month follow- up group, compared with the 6–-8 week group (P = 0.029). The authors recommended training intervals of less than 6 months based on their study.
Youngquist et al.19 tested ETI and BVM ventilation in paramedic students after initial training and an interval of 7–-21 months. Participants were randomised to different forms of retraining or control in the interim, and tested against a predefined list of skill components to determine a grade (fail, pass, high pass or honours). The odds of scoring among the higher grades on ETI testing were statistically lower for each additional month elapsed since initial training, with an OR of 0.93 (95% CI = 0.87 – 0.98). However, performance in BVM ventilation was maintained across the study time. It was noted that the paramedics in the study regularly performed BVM ventilation in their duties, but not ETI
Conclusions
Based on the literature search results, there is limited relevant literature that guides the learning curve and appropriate skill maintenance intervals for many critical care skills. However, in other areas, such as LMA placement, ETI emergency surgical airway, IV cannulation and intraosseous placement, there is a sufficient literature base to provide some guidance.
The results for LMA placement showed a relatively flat learning curve, with participants able to place the LMA successfully most of the time with very little practice (<5 attempts), particularly in mannequins. However, participants in both included studies utilising real patients4,5 showed improvements in the success rate of placements and decreasing complications after 40 and 45 attempts, respectively. The different definitions used for successful placement may account for the difference in the numbers of attempts to succeed. Alternatively, the contrasting results may indicate a different learning curve between placement in mannequins and humans. Ander et al.16 suggest that the skill is maintained for 12 months;, however, their data, showing an improvement in the time to insertion of a Fastrach airway during the study period, suggests that some interval experience may have been gained (data was collected on interval experience but not presented). Hence, the conclusion regarding skill maintenance must be questioned. Hein et al.6 produced a somewhat conflicting result, with increased time to successful LMA placement after a 6- month interval. However, the scenario testing skill retention was more involved and on a different mannequin than the initial training. Hence, whilest the study demonstrates improvement in skill retention following retraining, it is not definitive proof of skill fade at 6 months in its own right. The highest number of studies and, perhaps, the most robust data on learning curves was related to ETI Drawing firm conclusions remains hampered by the small number of participants in most studies, and the heterogeneity of methods and definitions of success. Overall, the studies showed that a greater than 80% success rate with two attempts could be achieved with relatively little experience. However, most studies suggested that around 50 cases were required to improve that success rate to >90% with two attempts. Wong et al.13 showed a steeper learning curve for prehospital intubation. Data from Je et al. and Kim et al., compared with Buis et al., suggests that it may take more attempts to learn the skill of intubation in the prehospital or emergency department setting compared to the operating theatre. This conclusion is supported by other studies comparing success rates of trainees in different environments.20 Other skills were not studied in the prehospital environment, However, it seems likely that success rates for other skills would follow a similar trend.
The study design of Kim et al.12 differed significantly from the other studies on intubation by grouping participants based on their previous experience in ETI The use of real patients undergoing CPR was also unique. It is unclear what resulted in the higher number of experiences with ETI required to achieve the competence suggested. The most likely explanation is that successful ETI is more difficult to achieve in patients undergoing CPR. Other factors may include the low number of intubation experiences across the cohort during the 2-year study period years (average of 10 each), the resuscitation room environment compared with the operating theatre, and the statistical analysis applied to extrapolate estimates for proficiency However, it could again be argued that the challenging circumstances for the participants in this study may more accurately reflect those faced by GDMOs when they called on to perform intubation.
The studies regarding emergency surgical airway suggest a flat learning curve in simulation models, with five or fewer simulations required for the success rate to plateau. It is unclear how this translates from the simulation environment to clinical practice. Kudavalli et al.18 suggest that a minimum retraining interval for this skill should not exceed 6 months. Prahbu et al.21 are widely quoted as recommending a training interval not exceeding 3 months at the Difficult Airway Society Meeting in 2001 after showing skill fade with the Melkher kit over that period.
The studies IV cannulation suggest that it may be a relatively difficult skill to attain and maintain a high success rate. Murgatroyd and Jones3 defined a relatively large tolerance for failure compared with the other skills, and half of the participants failed to reach that standard with CUSUM analysis. Ault et al. allowed three attempts at cannulation at two different sites (albeit in a complex patient cohort), and participants still required an average of 25 encounters for 10 successes.22 In contrast, IO placement had a very flat learning curve, demonstrated in simulation environments.23,25
Discussion
The frequency at which GDMO are required to perform critical care skills on a patient in extremis is low;, however, the consequences of failure may be dire. GDMOs may be disadvantaged in several ways in attaining and maintaining these skills. Firstly, for skills with a significant learning curve, they may not have the opportunity to climb that curve and reach a level of mastery where skills plateau. Also, these studies suggest infrequency of the practice of these skills will lead to a degradation in performance. In essence, all these skills could be considered for GDMOs in the same way preparing for a ‘“Can’t intubate, Can’t oxygenate’” scenario is for an anaesthetist, a low-frequency occurrence with potentially catastrophic consequences of failure. In light of this, and considering that the best evidence available for retraining critical care skills comes from studies surrounding emergency surgical airways or cricothyroidotomy, an ideal scenario would be that the interval for all the critical care skills GDMOs are required to be proficient in would not exceed 3 months.
There is further support for narrow retraining intervals of infrequently used skills in the wider medical literature. Studies have shown significant degradation in transthoracic echocardiography and some surgical skills 1 month after training.26,27 Laparoscopic surgical skills and advanced life support skills show deterioration at 6 months.28,29 Some protection in skill retention has been shown with experience and regular practice.29 Several studies have shown that teaching skills with distributed training (teaching a skill over a number of sessions spaced out over weeks to months) as opposed to massed training (teaching a skill in a non-interrupted block of training), was significantly protective against skill degradation.27,30 This was tested using surgical skills and was true across different regimes of distributed training.27,31
The retraining intervals discussed above are significant when the lengths of deployments are taken into consideration, as many are 6 months or greater, and there is good evidence of skill fade within that period. It may also have relevance to specialist deployments with low-frequency requirements for procedural skills;, however, that topic is beyond the scope of this discussion.
Many of these studies were undertaken in a simulation environment. While it is difficult to practice many of these skills outside the simulated environment, it is also unclear exactly how well skills gained in this environment translate to patient care.32
It is recognised that individual specialist colleges set retraining intervals for some of these skills as part of Continuing Professional Development (CPD) requirements. In ML-3, GDMOs must belong to the Royal Australian College of General Practitioners (RACGP) or the Australasian College of Rural and Remote Medicine (ACRRM), and, as such, are bound to their CPD requirements. Regardings critical care skills, RACGP requires BLS in each triennium,33 and ACRRM requires ALS and specific training requirements based on areas of special skills (e.g. anaesthetics or emergency medicine).34 There is obviously discordance between these requirements and those suggested above. Although an in- depth review of the CPD requirements of the specialist colleges in Australia is beyond the scope of this review, the author is unaware of any colleges with requirements as stringent as those suggested. While the review conducted was unable to identify a broad base of evidence for the required training and retraining for all the critical care skills that GDMOs potentially require, a number of key points and recommendations could be formulated based on the data:
- The literature provides guidance on the volume of practice required to become proficient in some critical care skills, although it is lacking in others.
- There is variation in the learning curve for different critical care skills and different environments.
- There is some guidance in the literature on the skill degradation that critical care skills suffer.
- For many critical care skills, the recommended retraining interval may be shorter than typical deployment durations.
Corresponding Author: R. McCarthy, rowan.mccarthy@defence.gov.au
Authors: R. McCarthy1
Author Affiliations:
1 Royal Australian Air Force – Headquarters Health Services Wing






