Abstract
Background and purpose: This study aimed to establish the treated prevalence of Bipolar Disorder (BD) in serving members of the Australian Defence Force (ADF) in light of a 2018 study of mental disorders in the ADF and Veteran population that found a surprisingly high 12-month prevalence rate.
Method: A retrospective review of the Defence electronic Health System (DeHS) was conducted for the periods 2015–16 and 2016–17 of all eligible Defence personnel. Two psychiatrists then reviewed each record with an entry for BD to confirm whether a clinical diagnosis was present with measures to optimise inter-rater reliability.
Results: 138 431 DeHS clinical records were searched, and 36 potential cases of BD were identified in the financial year 2015–16, of which 21 were confirmed to have a diagnosis of BD. Thirty-two potential cases of BD were found in the financial year (FY) 2016–17, of which 24 were confirmed to have a diagnosis of BD. The average 12-month prevalence of BD across FY 2015–16 and FY 2016–17 was 0.03% or 2.51 per 10 000.
Conclusion: The prevalence of BD in serving members was considerably lower than in the 2018 study. Possible explanations for this finding are examined.
Key terms: Bipolar Disorder (BD), prevalence, military
Introduction
In 2018, the most comprehensive survey of Australian Defence Force (ADF) members’ mental disorders to date estimated the prevalence of Bipolar Disorder (BD) among ex-full-time ADF members to be over four times that of the general population.1 This extraordinary finding raised many questions and prompted this study. BD is a major mood disorder defined by a history of either a manic or hypomanic episode with depressive episodes, resulting in functional impairment. It is often comorbid with other conditions, including substance misuse and personality and anxiety disorders.2 The mean age of onset of BD has been reported as late teens.3 The interval between the onset of BD and the start of management has been estimated at 5.8 years.4 Thus, it is a condition where the predominant age of onset coincides with an important age demographic of the ADF workforce (18–29 years). Furthermore, the risk of suicide among people with BD has been reported as 20–30 times that of the general population,5 with suicide risk said to be particularly high among younger patients during the first few years after diagnosis.6
The 2018 Mental Health Prevalence, Mental Health and Wellbeing Study,1 of the Transition and Wellbeing Research Programme (TWRP), explored the prevalence of mental disorders among ADF members who had transitioned (i.e., discharged) from regular ADF service between 2010 and 2014. They estimated the 12-month prevalence of BD in transitioned ADF members to be 9.8% (95% CI 7.0, 13.5%). However, it is important to note that the version of the Composite International Diagnostic Interview (CIDI) used in the Mental Health Prevalence study (World Mental Health Survey Initiative Version of the World Health Organization Composite International Diagnostic Interview Version 3.07) may have led to an overestimate. Mitchell (2013) reported concerns with this version and described the subsequent development of a re-calibrated algorithm to derive BD diagnoses,8 which has resulted in lower prevalence estimates. Nevertheless, the Mental Health Prevalence study finding was still significantly higher than the Australian civilian prevalence of BD of 1.7% without the revised algorithm and 0.9% with the revised algorithm.9
The mental health and wellbeing of personnel are of critical importance to the ADF, particularly given the potentially rigorous demands placed upon members and the higher rates of death from suicide among ex-serving ADF members, especially in the younger cohorts.10 This has been highlighted by the recent Royal Commission into Defence and Veteran Suicide.11 It follows that, along with other mental health conditions, accurate and timely diagnosis and appropriate management of BD should be an essential health consideration for the ADF.
Against this background, in February 2019, Joint Health Command tasked the ADF Centre for Mental Health (ADFCMH) to investigate the prevalence of BD and Post-Traumatic Stress Disorder (PTSD) in serving members of the ADF using the Defence electronic Health System (DeHS) records. This paper presents the findings of the BD study, specifically those related to the study aim to determine the period prevalence of BD diagnoses and the relevant demographic, service and diagnostic correlates among a cohort of ADF members. The results of the PTSD audit will be published separately.
Methods
Findings are reported in accordance with the STROBE Statement.12
Study design
A retrospective audit of the DeHS of all ADF personnel with at least one health record in the financial year (FY) 2015–16 and FY 2016–17.
Setting
The ADF is an all-volunteer force comprised of the Royal Australian Navy, Australian Army and Royal Australian Air Force, with 60 831 full-time members as of 2020–21.13 Over the last 20 years, the ADF deployed overseas on several warlike, peacekeeping, humanitarian assistance and disaster relief operations and provided extensive assistance within Australia in response to natural disasters and the COVID-19 pandemic. FY 2015–16 was chosen as it was the first complete year of operation of DeHS closest to the 2018 Mental Health Prevalence Study1 period of 2010–14. A further year (FY 2016–17) was audited to confirm the results obtained in FY 2015– 16.
Participants
Individuals serving in the ADF during the 2015–16 and 2016–17 FYs, with at least one DeHS record during that period, were eligible for inclusion. Individuals for whom there was no DeHS record for FY 2015–16 and FY 2016–17 were not eligible for inclusion.
Case selection inclusion criteria
A search of all DeHS records for eligible individuals using all Systematized Nomenclature of Medicine14 search terms relating to BD. This generated a list of identified personnel with probable BD diagnoses.
The identified records were individually assessed by psychiatrist investigators (DW, EH, CNJ and DM). For each case identified, all available DeHS records for FY 2015–16 and FY 2016–17 were reviewed using a standardised checklist of questions contained in ‘drop-down’ menus in an audit worksheet using a clinical diagnosis of BD as defined in Box 1. The clinical records were accepted as ‘the source of truth’. A BD diagnosis was considered present if there was any record that a psychiatrist had made this diagnosis during the relevant period. The BD diagnosis was considered not present if there was no evidence of a psychiatrist making the diagnosis or if the diagnosis had been made but was changed from BD by the end of the relevant period.
Exclusion criteria
Cases were excluded when records showed that the individual was discharged from service before the beginning of FY 2015–16 or FY 2016–17, or the individual was not a member of the ADF.
Variables
In addition to diagnostic and treatment information, psychiatric investigators extracted a range of demographic and occupational information of interest (Box 1).
Validation and inter-rater reliability
In order to validate the operational definitions of the demographic and BD variables of interest and to maximise inter-rater reliability, the data collection process for the FY 2015–16 cohort was piloted through a review of five randomly selected probable BD records by three psychiatrists (DW, EH, DM). These data were supplied to the project’s dedicated researcher (CM), who collated data and identified areas of agreement or disagreement.
|
Box 1: Variables used in audit by psychiatrist investigators Demographic variables Age (years, as at 1 July 2016); Gender (Male, Female); Service (Navy, Army, Air Force); Rank (Other Rank, NCO, Officer). Diagnostic variables Any diagnosis (Bipolar Disorder, Not Bipolar Disorder, Not Enough Information): Diagnosis of BD in effect during FY 2016–17, even if overturned. Diagnosis is based on presence of a discharge summary or psychiatrist’s report confirming that based upon the patient’s history, collateral history, out-patient or in- patient treatment history and/or direct observation/ MSE the member has a bipolar diagnosis. If a diagnosis of BD is made prior to AUDIT period, and sustained during the AUDIT period, then it is classified as a diagnosis in the AUDIT period. Confirmed diagnosis (Bipolar Disorder, Not Bipolar Disorder, Not Enough Information): Diagnosis of BD in effect as at 30 June 2017. Diagnosis is based on presence of a discharge summary or psychiatrist’s report confirming that based upon the patient’s history, collateral history, out-patient or in-patient treatment history and/or direct observation/MSE the member has a BD diagnosis. If a diagnosis of BD is made prior to AUDIT period and sustained throughout the AUDIT period, it is classified as a diagnosis in the AUDIT period. Subtype (Bipolar I disorder, Bipolar II disorder, Other, NA): Bipolar subtype, for confirmed diagnosis only. Bipolar I assigned if Bipolar 1, all episodes. Bipolar II assigned if Bipolar II, all episodes. Other if BD not otherwise classified. NA if Confirmed diagnosis = No OR Not enough information. Year of diagnosis (Year, Not Available, NA): For Confirmed diagnosis, only, year in which diagnosis initially made. Not available if year of diagnosis cannot be ascertained from clinical records. NA if Confirmed diagnosis = No OR Not enough information. |
Where CM could not resolve the disagreement with certainty (e.g., where there was clear evidence of an error by one psychiatrist, with the other two being in agreement), these were presented back to the three psychiatrists for discussion and resolution by consensus. Following this, both the variables list and definitions were refined.
Following the piloting phase, remaining BD records were reviewed in two batches, to maintain fidelity to the methodology and definitions and to allow for further refinements to the methodology and definitions, as required. Records were randomly assigned among the psychiatrists, ensuring that two psychiatrists reviewed each record and that these pairings varied. CM received and collated records. Disagreements were resolved by a third psychiatrist review of the record and then by consensus of the panel of psychiatrist investigators. Through this process, a small number of records were excluded due to evidence of the individual having left service before the audit period.
Denominator
The average of the number of individuals identified as being in the ADF as of 30 June 2015 and 30 June 2016 (for which data is available in Annual Defence Reports15): 1) including reserves; and 2) excluding reserves, were used as denominators (Table 1).
A similar method was used to calculate the denominator for FY 2016–17 using data obtained from the relevant Defence Report (Table 2).16
Data analysis
This report describes the findings of the BD section of the audit. Data were analysed descriptively and are presented as counts and rates (percentage and rates per 10 000), overall and by area of service.
Table 1: Headcount of ADF permanent and reserve members by area of service
| Headcount 30 June 2015 – permanent | 13 949 | 29 193 | 14 262 | 57 404 |
| Headcount 30 June 2015 – reserve | 4 862 | 13 590 | 4 634 | 23 086 |
| Headcount 30 June 2016 – permanent | 14 023 | 29 672 | 14 340 | 58 035 |
| Headcount 30 June 2016 – reserve | 3147 | 13 546 | 4 765 | 21 458 |
| Average 2015–16 total headcount | 17 991 | 43 001 | 19 001 | 79 992 |
| Average 2015–16 headcount, permanent only | 13 986 | 29 433 | 14 301 | 57 720 |
Figures calculated from Table 7.14 of ADF permanent and reserve forces by gender, 30 June 2015 and 30 June 201631
Table 2: Headcount of ADF permanent and reserve members by area of service
| Headcount 30 June 2016 – permanent | 14 023 | 29 672 | 14 340 | 58 035 |
| Headcount 30 June 2016 – reserve | 3 147 | 13 546 | 4 765 | 21 458 |
| Headcount 30 June 2017 – permanent | 13 657 | 30 161 | 14 388 | 58 206 |
| Headcount 30 June 2017 – reserve | 2 823 | 13 801 | 5 070 | 21 694 |
| Average 2016–17 total headcount | 16 825 | 43 590 | 19 282 | 79 697 |
| Average 2016–17 total headcount, permanent only | 13 840 | 29 917 | 14 364 | 58 121 |
Figures calculated from reports of ADF permanent and reserve forces by gender, 30 June 2016 and 30 June 201731 (permanent headcount for 30 June 2016, kept consistent with previous values).
Ethics
Ethics approval was obtained from the Departments of Defence and Veterans’ Affairs Human Research Ethics Committee (DDVA HREC) on 13 December 2019. (143-19—Bipolar Disorder in the ADF: Estimating prevalence from Defence electronic Health System records—greater than low risk.)
Results
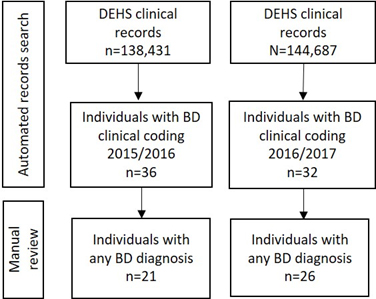
The flow chart describing the records selection process is represented in Figure 1.
Figure 1 shows that of 138 431 DeHS clinical records searched, 36 individuals were identified as having clinical coding for BD. Following manual review by the psychiatrist coders of these 36 records, 21 of these individuals were identified as having a BD diagnosis at some time during FY 2015–16. Sixteen of these individuals were then identified as having a confirmed diagnosis of BD, defined here as a diagnosis that was in effect as of 30 June 2016.
For FY 2016–17, 32 individuals were identified as having clinical coding for BD. Following manual review by the psychiatrist coders of these 32 records, 26 of these individuals were identified as having a BD diagnosis at some time during FY 2016–17. Twenty-four of these individuals were then identified as having a confirmed diagnosis of BD, defined here as a diagnosis that was in effect as of 30 June 2017.
The characteristics of individuals with a confirmed BD diagnosis is depicted in Table 3. In 2015–16, the mean age among those with a confirmed diagnosis of BD was 37 years (SD 10.4 years; median age 35.5 years; range 21–57 years). Individuals with a confirmed BD diagnosis were predominately male, with the majority identified among Army and Navy personnel. Of those with confirmed diagnoses, seven were officers and other ranks (ORs), and nine were non-commissioned officers (NCOs). Counts below five were not included to prevent inadvertent identification. Half of the individuals (n=8) with a confirmed diagnosis were identified as being diagnosed in 2015 or 2016, with most of these (n=5) being diagnosed in 2015. Of the remainder, three received their diagnoses in 2014, one in 2013 and three received their diagnoses in or prior to 2012. A record of diagnosis date could not be found for one individual.
Figure 1: Flow chart of the record selection process for FY 2015–16 and FY 2016–17, including automated and manual review processes
In 2016–17, the mean age among those with a confirmed BD diagnosis was 34.5 years (SD 8.7 years; median age 35.5 years; range 19–52 years). Individuals with a confirmed BD diagnosis were predominately male (male = 17, female = 7), while women made up approximately 17% of ADF personnel16 and were evenly spread across areas of service (Navy = 9, Army = 7, Air Force = 8). Most individuals (n=17) with a confirmed diagnosis were identified as being diagnosed in 2016 or 2017, with the majority of these (n=13) being diagnosed in 2016. Of the remainder, one received their diagnosis in 2015, four in 2014 and two received their diagnoses in 2013. Of those with confirmed diagnoses, 12 were officers and ORs, and 12 were NCOs.
In FY 2015–16, using confirmed diagnoses as the numerator, a prevalence of treated BD in the ADF, including reserves, of 0.02% or 2.00 per 10 000 was estimated. For full-time service members (reserves excluded), this increased to 0.0277% or 2.77 per 10 000 ADF. Expanding the numerator to include cases of BD during FY 2015–16, where the diagnosis was later disputed or overturned, yielded prevalence estimates of 0.0263%, or 2.63 per 10 000 among ADF, including reserves, or 0.0364% or 3.64 per 10 000 among ADF, excluding reserves. Overall, varying our numerator and denominator in these ways provided estimates that ranged between 2.00 BD cases per 10 000 ADF and 64 BD cases per 10 000 ADF.
In FY 2016–17, using confirmed diagnoses as the numerator, we estimated a prevalence of treated BD in the ADF, including reserves, of 0.03% or 3.01 per 10 000. This increased to 0.04% or 4.12 per 10 000 when reserves were excluded. Expanding the numerator to include individuals with an unconfirmed BD diagnosis was made during FY 2016–17, i.e., a diagnosis that was later disputed or overturned, yielded prevalence estimates of 0.03% or 3.26 per 10 000 among ADF, including reserves, or 0.04% or 4.47 per 10 000 excluding reserves. Overall, varying our numerator and denominator in these ways provided estimates that ranged between 3.01 BD cases per 10 000 ADF and 4.47 BD cases per 10 000 ADF. The average 12-month prevalence of confirmed BD diagnosis across FY 2015–16 and FY 2016–17 was 0.03% or 2.51 per 10 000. Variation according to the area of service is described in Table 4.
Table 3: Characteristics of individuals with a confirmed diagnosis of BD FY 2015-16 and 2016-17.
FY 2015–16 FY 2016–17
| Mean age of confirmed diagnosis of BD | 37 years (SD 10.4; median age 35.5; range 21–57) | 34.5 years (SD 8.7; median age 35.5; range 19–52) |
| Gender | Male and Female n=16* | Male n=17 Female n=7 |
| Service | Navy and Air Force n=9* Army n=7 |
Navy n=9 Army n=7 Air Force n=8 |
| Evidence of prescribing medication for BD | n=15 | n=23 |
| Year of diagnosis | 2012 or prior n=3 2013 n=1 2014 n=3 2015 n=5 2016 n=3 |
2013 n=2 2014 n=4 2015 n=1 2016 n=13 2017 n=4 |
| Rank | Officer and ORs n=7* NCO n=9 |
Officers and ORs n=12* NCO n=12 |
*Counts below five not included to prevent inadvertent identification.
Table 4: 12-month period prevalence of diagnosed Bipolar Disorder according to service, including reserves, for FY 2015–16 and FY 2016–17.
FY 2015–16FY 2016–17
| Navy | 0.03% (3.34 per 10 000) | 0.05% (5.35 per 10 000) |
| Army | 0.02% (1.63 per 10 000) | 0.02% (1.61 per 10 000) |
| Air Force | 0.02% (1.58 per 10 000) | 0.04% (4.15 per 10 000) |
| ADF | 0.02% (2.00 per 10 000) | 0.03% (3.01 per 10 000) |
Discussion
We found the 12 month prevalence for clinically diagnosed BD among serving ADF members, as recorded in the DeHS, to be 0.02% (1 July 2015 to 30 June 2016) and 0.03% (1 July 2016 to 30 June 2017), with the average 12 month prevalence across the 2 years at 0.03%, after rounding. This is much lower than the estimated 12 month prevalence of Bipolar I and II in the general Australian population (0.9–1.7%),9 and in transitioned ADF members (9.8%).1 Large population studies and anonymous military studies usually provide larger estimates of disorders than identified patient cohorts, with military personnel in particular reported to be two to four times more likely to report symptoms of a mental disorder in anonymous surveys compared to identifiable health screens.17 As a result, comparison with identified treated populations may be more helpful.
Sara and Malhi (2015) examined records of inpatient and community mental health care episodes in New South Wales, Australia, from 2002–2014 and found the average age and sex-standardised prevalence of BD in 15- to 64-year-olds was 12.1 per 10 000 population.18 Stalhman and Oetting (2012) estimated crude annual rates of incident mental disorder diagnoses from the United States (US) Defense Medical Surveillance System and Theater Medical Data Store to include deployed personnel of all ambulatory encounters and hospitalisations in all branches of the US Armed Forces from 2007–2016.19 Over the period, they found 1.2% (n=19 666) of mental health disorder diagnoses were attributable to BD with a crude annual rate of incident diagnosis of BD in 2015 of 11.3 per 10 000 person-years. Finally, Boulos and Zamorksi (2013) reviewed the medical records of a weighted, stratified, random sample (n=2045) of all Canadian Armed Forces personnel who deployed in support of operations in Afghanistan from 2001–2008 (n=30 513) and found a weighted cumulative incidence of BD of 0.3%.20
Possible explanations for our findings include, first, that there were very few serving members of the ADF with BD. This could result from a ‘healthy worker effect’ where recruitment and the rigours of military service have excluded those with BD. The healthy worker effect refers to employed persons being considered ‘inherently healthier than the general population, which also includes persons who are unemployable because of sickness or disability’.21 The healthy worker effect was originally described in civilian occupational health studies and has been extended to include the military22, where routine medical assessments occur (e.g., before and after deployment) and access to health care is readily available. However, this would apply to all current serving/active-duty military Mental Health Prevalence studies.
Second, serving members of the ADF with BD symptoms may not have presented to Defence health services for treatment as they may fail to recognise the condition or may see hypomanic episodes as being a positive development in light of the increased energy and productivity they can experience, especially when following periods of depression.23,24 Furthermore, stigma-related beliefs, such as fears of reduced deployability, harm to career or that others would treat them differently, are common among ADF personnel.25 Nevertheless, the same study also found that about half of transitioned ADF personnel and current serving members in 2015 sought mental health reviews within 3 months of developing concerns. Similar results were found in a UK military and veterans’ study.26
Third, ADF members who presented to health services with BD symptoms that warranted a diagnosis may not have been diagnosed correctly during the audit period. Diagnosing BD can be difficult. Manning et al. (1999) found that failure to diagnose BD in primary care settings was related to a cross-sectional approach taken by practitioners and a lack of familiarity with the phenomenology of the condition.27 Smith et al. (2011) found that between 3.3% and 21.6% of primary care patients with unipolar depression may have had undiagnosed BD when screening tools were used.28 However, concerns were raised about the low positive predictive value of the two screening tools employed.29 Parker (2015) also argued that psychiatrists struggle to diagnose BD II because their largely hospital-based training meant they rarely see persons with hypomania before they graduate as they are seldom admitted to hospital.24 He also stressed the need for all patients presenting with depression to be routinely screened for BD, which does not always occur among psychiatrists. Notwithstanding these concerns, there was no evidence that the healthcare personnel employed by the ADF are any better or worse at diagnosing BD than others. However, they may be reluctant to make the diagnosis as it is likely to lead to a medical discharge.
Fourth, there may have been a coding bias that led to the under-reporting of BD in DeHS records. Members with BD may have their condition entered into DeHS under a less specific term, such as adjustment disorder, depression or anxiety. Consultation notes are entered into the DeHS by health services personnel who may initially use a less definitive heading than BD while awaiting either further review or confirmation from a clinical psychologist or psychiatrist. In addition, once the diagnosis is clarified or confirmed, a member of the treating team (which does not usually include the attending specialist; they are predominantly civilians who do not have access to DeHS) would then need to open a new encounter of care to record a BD diagnosis. These circumstances could lead to delays or failure to apply the correct coding. However, even if cases were missed (e.g., due to clinical errors or oversights in coding) it is unlikely that these errors would be of sufficient magnitude to have overcome the gap between our estimates and those of the TWRP study.
Finally, Defence personnel with BD may have left the military early and before receiving a diagnosis. As mentioned, the mean age of onset of BD symptoms has been reported as being the late teens,3 and the interval between the onset of BD symptoms and the start of management has been estimated at 5.8 years.4 However, this audit found the mean age of persons diagnosed with BD was 37 years in FY 2015–16 and 35 in FY 2016–17, both significantly older than found in the TWRP Mental Health Prevalence Study, where the largest cohort of transitioned personnel with BD was aged 18–27.1 This could possibly be explained by the majority of members of the ADF with BD in the younger age group leaving service soon after the emergence of symptoms without presentation to or recognition by Defence mental health services.
Based on our examination of the DeHS, we concluded that there was a low prevalence of BD diagnoses in ADF members.
Strengths and limitations
This study had the benefit of access to the DeHS, meaning that all health contacts for all serving members within the ADF during the study period were accessible to the investigators. The audit of records was undertaken by military psychiatrists experienced in the use of the DeHS and experienced in reviewing clinical material relevant to diagnosis. This benefit, along with the use of a panel of psychiatrists for resolving diagnosis through consensus, was a method likely to reduce error. This systematic approach to estimating diagnostic prevalence through clinical review eliminated problems associated with false positives that have been present in automated diagnostic assessment tools.30
One of the challenges of the DeHS is that it only records clinical information related to health contacts within Defence or health contacts in the community that are communicated with Defence health services. For example, members could have been diagnosed with BD through contact with community or private health services and not communicated to Defence health services. It is also possible that members did not present to health services when suffering BD symptoms or a diagnosis was not made.
Conclusion
Our findings based on electronic records indicate that the prevalence of clinically diagnosed BD among serving ADF members was low and substantially lower than prevalence estimates for the general population. This differs from previous findings that suggested BD rates among current and ex-serving ADF members were higher than estimates for the general population1 when using an earlier version of the CIDI module for BD. Therefore, the use of the subsequent revised Harvard version of the bipolar module is recommended in future studies.8 Notwithstanding this and other potential explanations for our finding, enhancing clinical practice with respect to the identification and management of BD among ADF members is warranted.
Corresponding Author: D. Wallace, d_wallace@ozemail.com.au
Authors: D. Wallace1,2, E. Heffernan1,3,4,5, C. Meurk5,6, McKay7,8,9, C. Nas Jones2,10
Author Affiliations:
1 Australian Defence Force Centre for Mental Health – Joint Health Command
2 University of New South Wales – School of Psychiatry
3 Queensland Government Department of Health and Ageing – QFMHS
4 Queensland Health – Queensland Forensic Mental Health Service
5 The University of Queensland – School of Public Health
6 Forensic Mental Health Group – Queensland Centre for Mental Health Research
7 Joint Health Unit – Central Australia – Joint Health Command
8 The University of Sydney – Discipline of Psychiatry, Sydney Medical School
9 Macquarie University – Faculty of Medicine, Health and Human Sciences
10 Kuttabul Health Centre – Joint Health Command


