Introduction
Haemorrhage remains a leading cause of preventable deaths in conventional land warfare and, more recently, counterterrorism operations. From the Vietnam and Korean Wars to the contemporary battlefield in Iraq and Afghanistan with the Global War on Terrorism, haemorrhage accounts for 50–87% of potentially survivable casualties.1, 2 The implementation and ongoing development of Tactical Combat Casualty Care (TCCC), among other improvements in casualty care as part of a continuum of damage control resuscitation, has been shown to reduce preventable combat deaths significantly.3
The goals of damage control resuscitation in severely injured trauma patients are directed towards restoring intravascular volume and preventing or reversing acidosis, hypothermia and coagulopathy. This is understood to be a result of the combination of haemorrhage and austere environments associated with the battlefield and casualty evacuation. This is not limited to the tyranny of distance, logistics and communications constraints and enemy threat. Blood transfusion is an essential pillar of damage control resuscitation. Intravascular volume replacement with component blood products in casualties requiring massive transfusions is targeted in a 1:1:1 ratio of packed red blood cells (pRBC), plasma and platelets, with the addition of cryoprecipitate or fibrinogen concentrate to augment the fibrinogen content of plasma.4 Although this ratio attempts to replicate whole blood (WB), a massive transfusion of components cannot precisely replicate the physiologic ratios of WB with dilutions in haematocrit, platelet count and fibrinogen.5
While component blood products are preferred in civilian settings to maintain the sustainability of blood services and limit transfusion to identified needs when prompt laboratory services are available, WB transfusion has a long history in military medicine. WB has become the preferred product for resuscitation in severe traumatic haemorrhage in certain military contexts, especially in prehospital environments and early damage control resuscitation6 when diagnostic tests are unavailable or when waiting for results is inappropriate. Fresh whole blood (FWB) refers to the collection of WB on an emergency basis from a ‘walking blood bank’ (WBB). Resuscitation with FWB has been born of necessity to treat severe combat injuries and in potential mass casualty situations. In addition to overcoming the logistical constraints of blood component storage in forward environments, FWB reduces the reliance on diagnostic testing, delivering rapid lifesaving treatment without the reliance on sophisticated technology or personnel required for its operation. The Joint Trauma System Clinical Practice Guideline (JTS CPG) further discusses the use of autologous transfusion training sessions to build competency with a mechanism addressed in several journal articles and blogs.7-10
Autologous FWB transfusions are increasingly used in the training of many military units to prepare for effective WBB activation in combat operations, as well as other operations in which traumatic injuries are likely.8, 11 This narrative review summarises the published literature describing the potential opportunities and challenges of this training methodology, and compares this with our recent experience of autologous FWB transfusion training in a deployed US military Role 3 hospital.
Materials and methods
A literature review of relevant published studies was conducted using PubMed/Medline and EMBASE electronic database searches, and a Google Scholar internet search conducted in October 2021. A customised search strategy was built around the MeSH terms and the keywords for ‘autologous transfusion’, ‘walking blood bank’, ‘fresh whole blood’, ‘training’, ‘education’, ‘simulation’, ‘remote’, austere’, ‘military’, ‘battlefield’ and ‘deployed’. There were no language restrictions. An example of the PubMed electronic database search is: ‘(((walking blood bank) OR (autologous transfusion) OR (fresh whole blood)) AND (education OR training OR simulation)) AND (remote OR austere OR military OR battlefield OR deployed)’. Reference lists from identified full-text articles were hand searched for any additional references relevant to the review.
A description of program establishment, experiences and integration with other trauma training from a deployed multinational military hospital (US Army Role 3 Health Center) from February to October 2021 is presented. The autologous FWB transfusion training program aimed to train CPG-compliant FWB collection and transfusion without degrading our available WBB donor pool. The number of autologous FWB transfusions, both successful and unsuccessful, is recorded.
Results
Risk of adverse events
Autologous blood transfusion training has been safely utilised as a training tool for more than a decade in the US military, yet autologous transfusion training continues to be met with scepticism and reluctance.8 Concerns range from risk of iatrogenic hypocalcaemia to allergic reaction and acute haemolytic transfusion reaction due to inadvertent human error. Donham et al. reported an experience of 3408 autologous transfusions in training with no major adverse events.8 Their adverse events reported were a vasovagal episode in 14 volunteers (0.41%), ocular blood exposure in two participants (0.06%) and urticaria in one case (0.02%). Their series had no reported anaphylactic or major or minor haemolytic transfusion reactions. This compares favourably to FWB transfusion in a WBB context, with two (2.3%) transfusion reactions noted in a series of patients from the 31st Combat Support Hospital in Iraq, 2004.12 The reported reactions were one case each of febrile non-haemolytic transfusion reaction and transfusion-related acute lung injury, neither of which is theoretically possible with fresh autologous retransfusion.
Risk of blood-borne virus transmission
Infectious disease transmission (particularly of blood-borne viruses (BBV)) is a low but serious risk of blood product transfusion that is virtually absent in autologous transfusion training. Retrospective blood sample analysis of 2831 samples of FWB transfusion in Iraq and Afghanistan during 2003–06 indicated three cases (0.11%) of positive hepatitis C virus (HCV), two cases (0.07%) of human lymphotropic virus (HTLV) and no cases of either human immunodeficiency virus (HIV) 1/2 or hepatitis B virus (HBV).12 Comparatively, the rates of BBV in deployed military donors were lower than in non-deployed military and civilian donors in the US. There were no positive cases in any of the prescreened donor pool of 406 personnel in 2004. Australian blood supply is among the safest in the world, and BBV transmission risk is generally lower than the US and other international risk estimates. The residual risk is now so low that mathematical modelling is required to predict risk, estimated at 1 in 7 299 000 for human immunodeficiency virus.13
Repeated donation
Of interest, a Norwegian Special Operations study on the potential haematologic effects of repeated autologous FWB transfusion training demonstrated significant reductions in haemoglobin and ferritin over time.9 This reduction is attributed to cumulative blood loss through multiple blood samples and the transfusion process in volunteers with up to five autologous transfusions. This blood loss was estimated at 380 ml. The clinical relevance of this statistically significant reduction is unclear. An earlier Norwegian study did not find any significant decrease in combat readiness skills after donations of one unit of blood (450 ml).14 This volume of blood donation and statistically significant haemoglobin and ferritin reduction may prove clinically insignificant and therefore have little bearing on donor operational capability.
Observations of experience in a US-deployed Role 3 hospital training program
This program served as a high-fidelity ‘full-dress rehearsal’ for our WBB staff to learn and validate the screening of donors and collection of blood. To further capitalise on the autologous training sessions, the FWB transfusions were conducted by our Role 3 assigned combat medics who are likely to perform prehospital FWB transfusions and train non-medical personnel on the collection of FWB in future assignments. This training also served as a force multiplier to facilitate hyper-realistic, immersive trauma and mass casualty simulation training. Figure 4 shows an example of such a scenario with autologous FWB transfusion training embedded within a simulated night trauma scenario onboard a UH-60 Blackhawk aeromedical evacuation helicopter and, later, the Role 3 facility.
Program establishment
Volunteers for the autologous FWB training program were drawn from the existing WBB donor pool. This pool was established from almost 100 base-wide volunteers (both military and civilian contractors) who were prescreened for blood type and BBV (HIV, HBV, HCV and malaria). Volunteers were sought at an information and recruitment stall at the base-wide dining facility. There were no restrictions on the type of employment of personnel, and the robust size of the donor pool was facilitated by the Role 3 facility existing within an established military base.
We intentionally employed non-clinical personnel as our WBB collection team, including those without trauma resuscitation responsibilities in the hospital and with limited phlebotomy experience. This commitment was voluntary, and our WBB collection team included the physical therapist and dietician intrinsic to the health facility, and an extrinsic veterinarian and logistics officer. Collection team members received informal hands-on training through the laboratory and emergency medicine team staff.
Experience
During our deployment, we recorded 32/37 (86.5%) successful autologous transfusions for training over eight sessions. Five volunteers were unsuccessful, as the required minimum amount required for autologous transfusion was not achieved. This was generally due to venepuncture failure. Of these personnel, three returned for successful transfusions at a later session. There were a maximum of six volunteers in a single session. Blood collectors would collect from 1–2 personnel per session, with a total of 6–10 total personnel completed during the program (Figure 1).
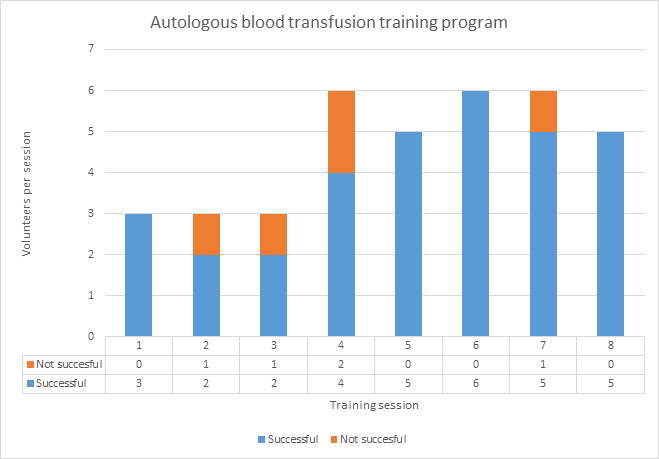
Figure 1 – Autologous blood transfusion volunteers per session
Our safety protocol included blood sampling, pre-donation, immediate post-transfusion and 2-day post-transfusion laboratory tests (including a full blood count and electrolyte panel) to ensure all volunteer participants remained available for donation. Standard equipment for the FWB collection is shown in Figure 2. Repeat autologous transfusion participation was generally avoided in our training due to a surplus volunteer donor pool.
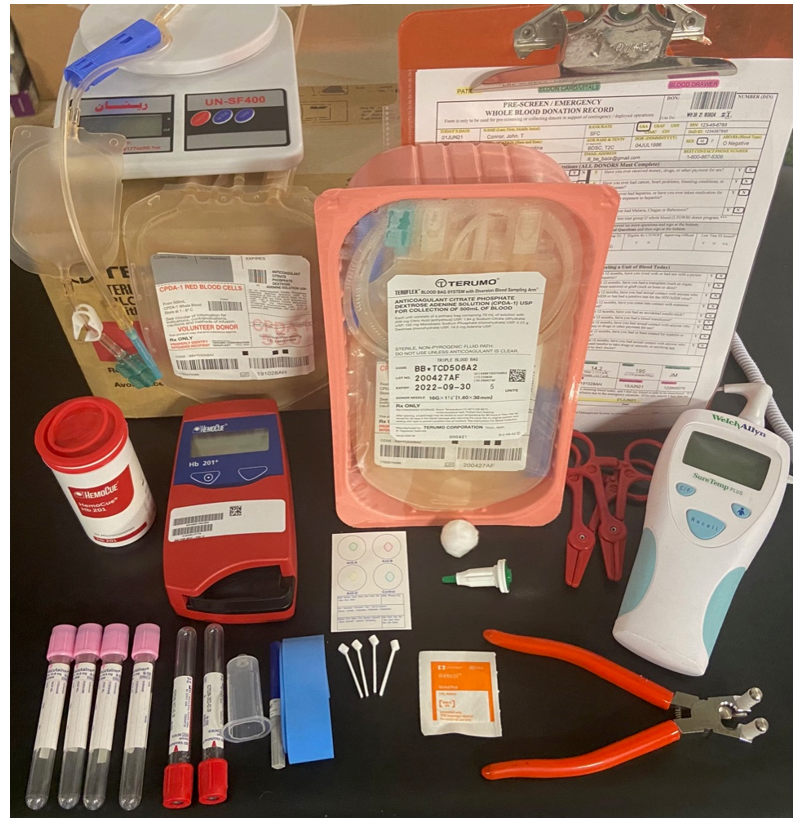
Figure 2 – Fresh whole blood collection equipment for autologous blood transfusion training
There were no adverse events reported in our series. In particular, there were no reported thrombophlebitis or deep vein thrombosis events. As mentioned, our autologous transfusion training volunteers were drawn from the WBB donor pool and were therefore prescreened for BBV. Additionally, given that the volunteers received their own FWB per JTS CPG, the risk of BBV or other infectious disease transmission was negligible.
The time from the volunteers’ activation to the first unit of FWB delivered to the emergency medicine team was recorded as a surrogate marker of the efficiency of the process. Over the program, the average time recorded was 55 minutes (range 38–75 minutes). As Figure 3 shows, there was an improvement from the initial session (75 minutes), to the mean time of 41 minutes in the last three sessions.
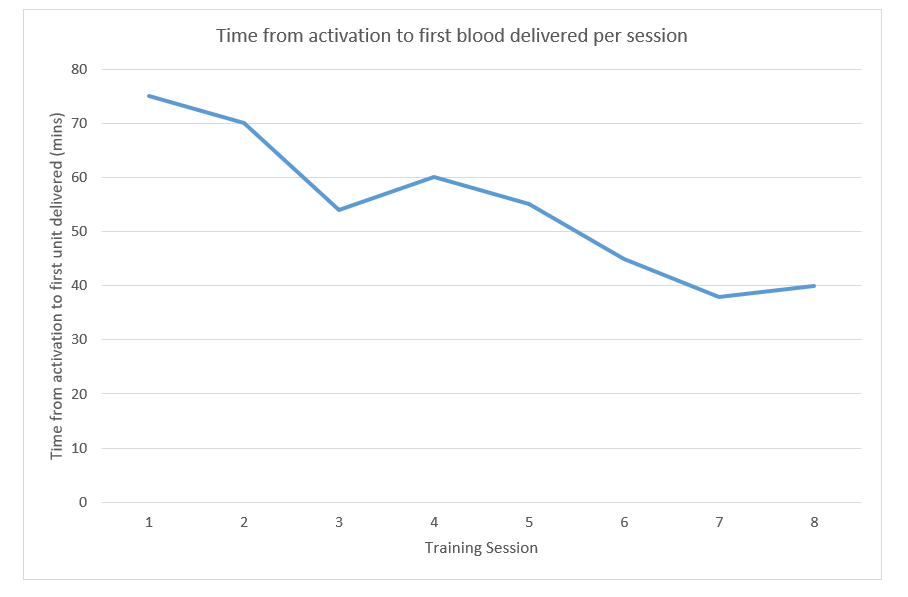
Figure 3 – Time from activation to first unit of blood delivered
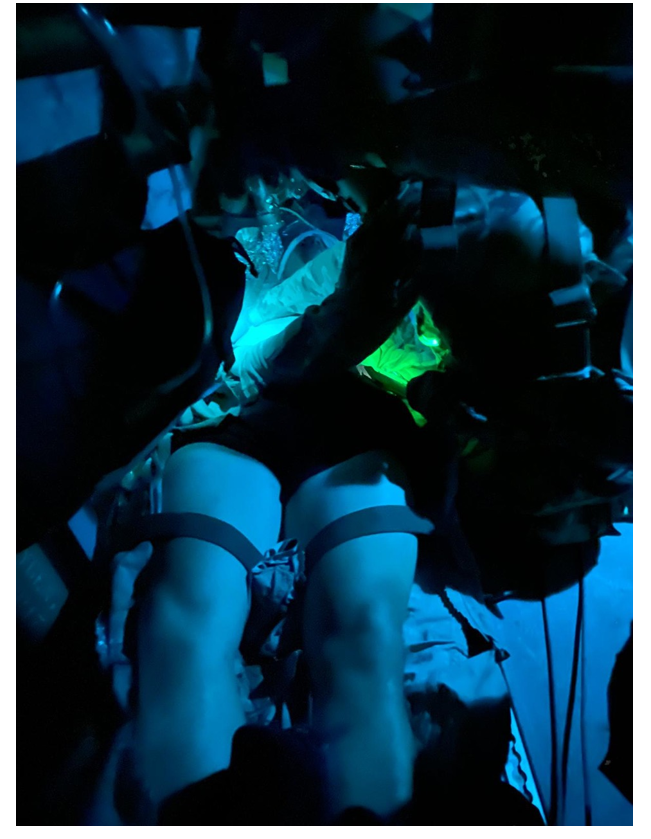
Figure 4 – Autologous blood transfusion training during simulated night trauma scenario onboard UH-60 Blackhawk aeromedical evacuation
Training opportunities and considerations
Our early training sessions utilised volunteers with high-titre O and A, B or AB blood types, as determined during the prior mentioned pre-screening. These volunteers were deemed less likely to be called for WBB donations to prevent the loss of low-titre O donors from the donation pool. Under logistical constraints, the preference for low-titre O donors for FWB transfusion in life-threatening haemorrhagic shock is acknowledged.15 Unsuccessful autologous transfusions, such as incomplete collection or incomplete transfusion, would potentially remove the volunteer from the WBB donor pool for 56 days. Once skills and processes were refined and our donor pool was optimal, we allowed low-titre O volunteers to participate in the autologous transfusion process.
Discussion
The use of FWB transfusions in prehospital resuscitation of trauma casualties as far forward as the point of injury (PoI) is recognised in the updated JTS CPG for Prehospital Blood Transfusion.11 Autologous FWB training is essential to achieve and maintain proficiency in FWB transfusion, which is expected to reach closer to the PoI of prehospital casualties. The utilisation of safe autologous blood donations for training competency can directly impact patient care where logistics and supply have limited or no ability to immediately respond to demand increases. At the PoI, medical personnel have limited ability to carry a small volume of cold-stored blood products, most likely cold-stored low-titre O WB at the time of this publication.
While this has been a common practice in US special operations forces to date, a FWB WBB is likely the only mechanism to resuscitate a trauma casualty at PoI or in the Role 1 facility of conventional forces. Once evacuated, subsequent treatment facilities have storage capability for WB and blood products, which are managed at the theatre blood service detachment level. Even in the most robustly supported environments, products can be rapidly consumed in treatment and outpace resupply. A reported common practice at minimally staffed Role 2 damage control surgery locations is to mobilise the WBB at the first notification of an inbound trauma casualty, decreasing the time between the order to collect FWB and its bedside delivery. This may also offer the ability to maintain somewhat lower blood supply levels by managing occasional spikes in consumption with the FWB WBB.
A proficient and well-rehearsed WBB can manage risk during interim periods of low supply volume while the resupply chain mobilises. The success rate of autologous transfusions completed also improved with later sessions in our experience (Figure 1). Though not a direct performance indicator, the average time recorded from activation to the first unit of blood delivered was reduced from 75 minutes in the first session to a mean time of 41 minutes in the last three sessions in our autologous training program. It should be noted that these timings were achieved in a controlled setting, emphasising safety and process and not an end goal of the training. These success rate and timing improvements reflect the WBB collection team gaining proficiency and maturity in the administrative process from activation to blood transfusion. Autologous FWB transfusion training allowed for high-fidelity simulation of the complexities of varied donor vascular anatomy and the effect of perspiration on securing vascular access devices, among other challenges. To our knowledge, no simulated training aid or mannequin currently exists to replicate this process.
There is limited literature on autologous FWB transfusion training, let alone the risks of such training. Although this literature exists within broader literature on FWB transfusion risks, and though the two are similar in concept, there are distinct differences in risk profiles due to the autologous nature of transfusions. In the most extensive case series to date, there were very few minor adverse events and no major anaphylactic or haemolytic transfusion reactions.8 This reflects our experience, with no adverse events noted in our small series. The autologous nature of transfusions may also explain the lower risk of transfusion reaction noted when compared to rates seen in FWB transfusion in a combat WBB context. In addition, BBV or other infectious disease transmissions from donor to recipient are eliminated. There are no case reports of BBV or other infectious disease transmissions in autologous FWB transfusion training. Our training also avoided repeat autologous transfusion due to a surplus volunteer donor pool. The intent was to continue avoiding repeat autologous transfusion at the US Role 3 hospital, given the literature on significant haemoglobin and ferritin reductions with repeated autologous FWB transfusion training,9 and the benefit of exposing the WBB collection team to the variability among the volunteers.
This narrative review article highlights the available literature and compares it to our recent deployed experience. With appropriate safety processes, autologous FWB transfusion training is feasible, high-fidelity, low-risk training. However, when there is not an excess of volunteer donors available for training, further prospective research is required to better define the clinical significance of any haemoglobin, ferritin and biochemistry changes with repeated donations or delayed transfusion.
Corresponding Author: D L Chan, daniel.l.chan@unsw.edu.au
Authors: D L. Chan1,2,3, D. Fritz4, T. Nessler5, L. Santoy6, W. Peterson7, M. Reade8
Author Affiliations:
1 Australian Army – 1/5 Health Support Company
2 Western Sydney University School of Medicine
3 University of New South Wales – Saint George Campus
4 Brooke Army Medical Center – Department of Emergency Medicine
5 Carl R Darnall Army Medical Center – Department of Emergency Medicine
6 Carl R Darnall Army Medical Center – Department of Rehabilitation
7 Brooke Army Medical Center – Department of General Surgery
8 Australian Army – Directorate of Army Health


