Abstract
Aortic trauma is often poorly recognised in a trauma setting and represents a significant cause of lethal injury. Most casualties will die at the scene. This article attempts to define the mechanisms and clinical features of aortic trauma. An understanding of aortic trauma may allow early recognition of such an injury in a trauma patient and therefore prompt immediate transfer to a level 4 or 5 facility with cardiothoracic support.
Introduction
Aortic trauma is often associated with severe blunt trauma. Vesalius made the first reference of aortic trauma in 1557; however, it has been in the last 50 years that further advancements in diagnosis and management of this condition have occurred. Around 85% of such victims will die at the scene of injury. It has a high mortality rate. This may be a result of the aortic injury itself but also may encompass other concomitant injuries the casualty may have sustained. Smith et al found aortic trauma to be the second most common cause of death behind head injury in a study of 387 blunt trauma deaths. Such trauma, once recognised, is time-consuming and takes up precious health resources. This is most challenging in a military setting with limited health personnel. Trauma of this scale implies a significant risk of loss of life resulting in a priority one status. Evacuation to a level 4 or 5 facility would be justified.
Aetiology
Traumatic aortic rupture is caused primarily by motor vehicle/ pedestrian collisions. Other important causes include falls from great heights, airplane accidents and landslide burials. All of these examples are classified as blunt aortic trauma and need to be recognised, especially in a military setting.
Penetrating aortic injuries result in a puncture or laceration of the aorta. It is usually caused by projectiles (e.g. high-velocity round) or knives. The consequence of such an injury depends on the site and severity of the injury and immediate surgical treatment is indicated.
Traumatic aortic rupture is rapidly lethal. 85-90% of casualties will die prior to a resuscitation facility. Most will succumb to rapid haemorrhage culminating in hypovolaemic shock and death. The natural history of an untreated aortic injury in those who will survive the next 24 hours is unknown.
The site of rupture can be categorised as:
- Aortic isthmus (90%)
- Right brachiocephalic artery origin (5%).
- Left subclavian origin (3%).
- Descending thoraric aorta
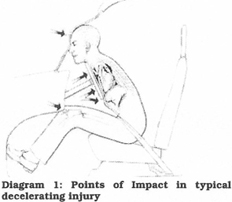
Mechanisms of Injury
There are 3 possible stresses that can be applied to the aortas:
- A horizontal deceleration with or without chest compression (e.g. MVA). The deceleration difference between the mobile aortic arch and the relatively immobile descending aorta exposes the aortic isthmus to tension. This leads to rupture opposite the site of fixation.
- Marked chest compression (e.g. landslide burial). This creates a bending stress when the heart exerts traction on the aortic arch, resulting in hyperflexion of the blood-filled aortic arch against the hilar structures of the left lung.
- Crushing injuries involving flexing of the spine.
These mechanisms produce stresses in the form of shearing, bending, and torsion respectively. Most tears are linear and may involve partial or complete transection of the aorta. Death is instantaneous if all the layers of the aorta, mediastinal tissues and parietal pleura are breached. Sudden uncontrolled blood loss thus ensues. However, a false aneurysm may occur if the mediastinal tissues remains intact producing a tamponade effect which reduces the amount of blood loss.
The reason why 10% of patients are alive that reach a resuscitation facility is because they have developed a false aneurysm.
Diagnosis
Aortic trauma is difficult to diagnose. A high index of suspicion is required, and this can be difficult when multiple injuries are present which can confound the resuscitation team’s minds. However, a history of a motor vehicle accident involving high speed with an acceleration /deceleration component should alert to the possibility of such an injury.
Symptoms may be non-existent or subtle. Retrostemal or interscapular pain may be secondary to stretching of the aortic adventitia. Other symptoms include cough, stridor, haemoptysis, and dyspnoeas. Examination of the patient may reveal acute onset of upper extremity hyperextension and a harsh systolic murmur over the praecordium. At this point, the collection of signs and symptoms may not herald a diagnosis of aortic trauma. If possible, a supine chest x-ray should be done as part of the trauma series.
Features suggestive of aortic trauma on a chest x-ray include:
- Increase in the width of the mediastinum.
- Loss of sharpness of the aortic outline.
- Depression of the left main bronchus.
- Deviation of the tranchea to the right.
- Obliteration of the aortopulmonary window.
- Left pleural effusion; fractures of the first rib, thoracic spine, sternum, clavicle; and a deviated nasogastric tube.

First 1- Chest X-ray
Given the many features that may be evident on the chest x-ray, the three most sensitive findings are mediastinal widening >8 em; mediastinal widening by a mediastinum to chest ratio >0.25; and opacification of the aortopulmonary window. According to Woodring et al., the negative predictive value of a normal chest x-ray ranges between 75- 94%8. Also, it is possible for a blunt aortic injury to be sustained in the presence of a normal chest x-ray9. However, many authors stress that no individual radiographic sign is sufficiently sensitive, specific, or predictive as a diagnostic finding.
Management
As with all trauma scenarios, the principles of resuscitation should be adhered to. Airway, breathing and circulation should be given utmost priority in stabilising the patient. Once the patient is stable, a thorough secondary survey is required to elucidate the extent of injuries present and to formulate possible diagnoses. If aortic trauma is thought to be present, the casualty should be classified as priority one and evacuated by aeromedical evacuation to a level 4/5 facility with cardiothoracic support. Such a facility may not be readily accessible due to distance or logistical reasons. If possible, the blood pressure should be kept below 120 mmHg systolic so as to decrease the shearing effect of the pulse on the aortic tissues. Controlled blood pressure via the use of beta-blockers is important when treatment is delayed or non-operative management is contemplated6. Prompt surgical repair of the aortic injury is the definitive step in the management of such patients. Therefore, aortic trauma not able to be managed expediently carries a poor prognosis. If multiple casualties are present, consideration must be given to those patients who can more positive prognosis versus those with a poor prognosis. These ethical considerations may arise in military settings, where resources are limited.
Conclusion
Aortic trauma represents one extreme of injuries that can be sustained in a military scenario. It cannot be further emphasised that prompt resuscitation of the casualty is the best management at a level 1 or 2 facility. Recognition of complex injuries, such as aortic trauma, is not only important, but necessitates the immediate evacuation to a higher-level facility. However, such injuries can a poor prognosis.






