ABSTRACT
THE AUSTRALIAN DEFENCE FORCE (ADF) has had an Aeromedical Evacuation (AME) capability in Dili, East Timor supporting INTERFET and UNTAET since September 1999. This unit, the Aeromedical Staging Facility (ASF), has provided excellent experience for military medical staff and has also provided excellent support to both the peace enforcing mission and the East Timorese people.
Analysis of cases from May 2000 to January 2002 demonstrates that ADF medical officers may not be adequately trained in various aspects of medicine to provide appropriate care to both ADF and civilian personnel and may not meet civilian standards. ADF Personnel are required to do several courses prior to deployment but often are deployed without these prerequisites. Permanent Medical Officers are also often not as clinically competent as their civilian counterparts.
The issue of competency and training needs to be addressed for current and future operations where the increased incidence of small-scale Operations Other Than War has reduced the ADF health support capability. The paucity of combat casualties since Vietnam has decreased the requirement for a first-class highly specialised aeromedical retrieval and resuscitation team.
INTRODUCTION
Aeromedical retrieval is an important component of ADF operations and doctrine.1 It allows rapid evacuation of casualties from the site of injury to a definitive resuscitation centre and, after stabilisation, transfer to a higher level of care if required. Aeromedical retrieval was first used effectively in Korea and extensively utilised in Vietnam where casualties could be transferred from site of wounding to definitive surgical and resuscitation centre in 20 minutes.2
The ADF has had an AME capability in Dili, East Timor since the start of INTERFET, which has continued on in support of the United Nations Peace Enforcing Mission UNTAET. Currently, the ASF consists of dedicated 6 people AME unit with two medical officers, two nursing officers and two medical assistants. The unit is located at the Heliport in Dili and provides fixed-wing (FWAME) and rotary wing (RWAME) AME for United Nations members and East Timorese locals. The ADF has a second AME capability in East Timor with the Australian Regular Army AME team in Moleana facilitated by 5 Aviation Regiment. This unit will not be discussed in this article.
This article will analyse the statistics of AME missions performed by the ASF team over a 21-month period and will aim to identify the capabilities required to perform these roles.
ANALYSIS OF MISSION DATA AME Numbers
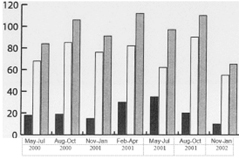
The ASF performed a total of 666 AME in the period between May 2000 and January 2002 (Table 1). Of these evacuations, 139 were fixed-wing and 527 were rotary wing. On average, the ASF was undertaking 32
AME’s a month with 7 fixed-wing and 25 rotary-wing. It is interesting that the current fixed-wing AME course is four weeks long, not including the Operational Health Support (OHS) phase of the course, and the rotary-wing course is one week long. The bulk of ADF AME’s are now rotary-wing and not fixed-wing.
Table 1: AME Numbers
C = J Fixed Wing
CJ Rotary Wing
TOTAL
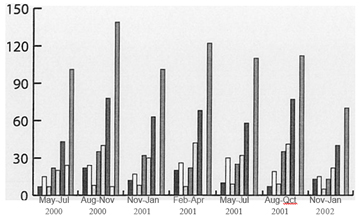
AME Patient Numbers
The patients retrieved by the ASF staff included ADF Personnel, other UN military personnel, UN civilians and East Timorese. Of the 757 patients retrieved by the ASF, 88 were ADF personnel compared with 431 East Timorese. 31 patients were not reported (Table 2). The East Timorese civilians were the most unwell patients with the prerequisite for transfer being only priority one or two cases. The East Timorese transferred were also of varied age including 17% of cases being aged 16 years or under.
EJ TOTAL c=J EM Female c=J uNMil
C=J other EM Male AUS
EM Total c=J UNCiv
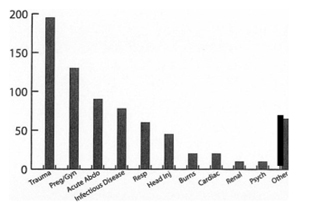
Illness Categories
Trauma with head injury was the bulk of the clinical cases with a total of 240 cases (45 head injuries) out of the 720 cases recorded (Table 3). These cases included a variety of presentations such as crocodile attack, machete injury, falls, motor vehicle accidents and gunshot wounds. Obstetric and gynaecological problems were also prevalent with 132 cases. This figure includes the 3 deliveries occurring in-flight. Other obstetric cases included antepartum haemorrhage, obstructed labour, twin pregnancies, arm or leg presentations and postpartum haemorrhage.
The remainder of cases include a variety of presentations such as a variety of infectious diseases, respiratory conditions and bums. The most unwell East Timorese patients were transported for care at the United Nations Military Hospital (UNMHET) with the others sent to the International Committee for the Red Cross Hospital (currently the Dili General). Severely ill infants were unable to be admitted for ventilation at the UNMHET due to the presence of only adult ventilators.
Table 3: Illness Categories
Aircraft Utilisation
Aircraft utilised were sourced from a variety of different countries (Table 4). The bulk of the rotary-wing AME were performed on CHC Australia Bell 212 and Super Puma aircraft. Other rotary-wing aircraft include the Russian Mi-8, the Chilean Army Puma and the New Zealand Iroquois. Fixed wing assets used were the SAFAIR C130 and the PEL AIR West Wind. Strategic AME’s were also performed by the ASF to Thailand and Portugal.
Table 4: Aircraft Used
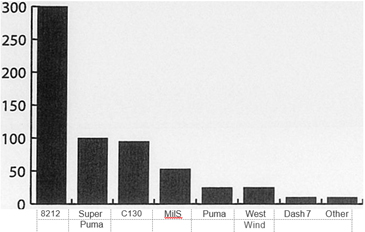

Figure 1- The patients positioned in the Chilean Army Puma. The female patient with the fractured mandible is positioned on the middle litter. The configuration within the Chilean Army Puma allows for rapid evacuation of up to six casualties with seating for up to four medical personnel.
The AME team received a call at 1405hrs on 04 February 2001, informing of two patients injured in a Motor Vehicle Accident (MVA), one with neck pain and the other with facial injuries. On arrival the AME team was escorted to the Regimental Aid Post (RAP) to assess the patients.
Patient A, a 20yr old female had suffered severe facial lacerations and disruption of the mandible as a result of the MVA. She was maintaining her own airway positioned on her side and was otherwise stable. The cervical spine had not been cleared but the patient was encouraged not to move her neck and transfers were conducted using inline C-spine care. Patient A had also suffered a suspected fractured left humerus but there was no other sign of injury. An 18-gauge intravenous cannula was sited, 12.5mg Stemetil and 10mg Morphine administered and Hartman’s solution infused.
Patient B had been struck across the chest by the roll bar of the vehicle. She had lower cervical spine pain but, on report from the NGO doctor at the scene, had no focal areas of tenderness. A hard-cervical spine collar had been placed prior to the arrival of the AME team. Airway, breathing and circulation were intact. The patient’s abdomen was firm and generally tender. An IVC was inserted, Hartman’s solution commenced and 12.5mg Stemetil administered IMI. Intravenous Morphine Smg was administered prior to transfer.
Patient C, a 7yr old male was placed on a stretcher for comfort. He had soft tissue loss from the right leg and was unable to weight bear. There was no other sign of injury.
The patients were loaded onto the Puma with Patient A in the middle tier. Patient A was positioned on her side with her head supported by pillows. In this position she was able to maintain her own airway and a small amount of blood drained away in flight. All patients remained stable throughout the twenty five-minute flight. On reaching Dili, all patients were transferred to the International Committee of the Red Cross (ICRC) Hospital.
AME CASE- DISCUSSION
This case highlights several important points for discussion. In particular, it highlights the need for pre-deployment clinical training. Optimum care for Patient B should probably have been inline cervical spine care with rapid sequence induction, intubation and ventilation. The patient could then have had a hard cervical collar placed and been transported with spinal precautions. On reaching Dili, the patient would have then been transferred to the United Nations Military Hospital (UNMHET) for definitive care.
This was not done for several reasons. The airway experience of the AME medical officer was not sufficient that he was confident to secure a definitive air way without complication. As such, the patient was transported on her side relying on her own ability to maintain an airway. If the patient had been intubated electively she then would have had to be transferred to the UNMHET, as the ICRC Hospital had no means for ventilating patients for a long period. The UNMHET was not geared to treat and care for East Timorese patients for longer than two to three days.
The question to be asked is what if this patient was an Australian Digger? Would the experience and clinical skill of the AME team be sufficient enough to provide care similar to that provided within Australia?
This case also highlights the need for training and exposure to aircraft other than those used within the ADF Our increased exposure to United Nations operations, peacekeeping and peace enforcing operations means that our personnel will be involved in AME on the airframes of other military or civilian organisations.
DISCUSSION
The Australian public expects a high standard of care of the deployed ADF soldier and it would seem ideal that the ADF AME team is trained to a similar civilian standard. This civilian standard is usually a dedicated retrieval service with a highly trained staff. The medical staff are usually specially trained senior emergency and anaesthetics registrars with specialised paramedics.
NRMA Care Flight employs this model and performs on average 1000 missions per year providing a retrieval service based out of Westmead and Orange. It also has a capacity for international retrieval’. Royal Flying Doctors Service (RFDS) operates 40 aircraft and the daily patient load is greater than 5004.
The ADF AME teams are junior medical officers with two years’ experience post-graduation and EMST and a one-week RWAME training course on aircraft safety and basic flight medicine. Helicopter Underwater Escape Training (HUET) training is not a requirement for the ADF teams though it is a legal requirement for civilian teams. There is no requirement for training or currency in resuscitation medicine. To put this in a military perspective, before deploying to East Timor all members are required to pass a weapons handling test and shoot within three months of deployment. This is again tested in the days before deployment. It is possible to deploy to East Timor with no proficiency in resuscitation and indeed definitive airway management.
The peacetime role of a military medical officer is that of a general practitioner with a very fit, predominantly male 18-55-year-old population. It involves a lot of administrative work and is not appropriate preparation for deployment. Current Anaesthetic and Emergency College guidelines outline minimum standards for transport of critically ill. The basic principle is that the transport improves patient care and management is equal or better than point of referral. The Royal Australasian College of Anaesthetists requires a trainee to have at least three months of accredited training to be left alone with a patient in the operating theatre or to transfer from operating theatre to another part of hospital5. Is ADF AME medicine legal when an AME team is tasked to retrieve an intubated patient from the field?
In considering the above, it is important to distinguish the differences between combat and peace enforcing AME. East Timor has seen a relatively low incidence of penetrating trauma with the majority of serious cases being Intensive Care Unit (ICU) type injuries. This closely matches the civilian experience in Australia. Experience in retrieval medicine would split AME missions into time-critical and non-time-critical. Time-critical AME are injuries such as penetrating trauma where an operating theatre is required for definitive management and an EMST current general duties medical officer and nursing officer are qualified for the mission. Interventions such as intubation, ICC and ventilation are required skills for this mission.
A study conducted out of NRMA Care Flight suggested that an appropriate critical care doctor on helicopter retrieval of trauma patients with blunt trauma improved mortality significantly (50% reduction of predicted deaths) compared to paramedics. This was thought to be to the enhanced procedural capabilities of physicians especially in airway and ventilatory control. Prehospital times, however, were prolonged. 6
Non-time critical AME patients are patients whose injuries require intensive care rather than an operating theatre for definitive management. These injuries include severe burns and sepsis, cerebral malaria and pneumonia, dengue haemorrhagic fever and reptile envenomation. Here the patient would benefit from the provision of intensive care from the moment the retrieval team reaches the patient. The team need to be skilled in advanced resuscitation skills plus both central and arterial line insertion and the use of infusions for sedation and inotropes. This is more closely aligned to Care Flight type service and possibly a more appropriate service for peace enforcing operations.
SOLUTIONS
Possible solutions to provide this level of care include co-location of the helipad with a level 3 hospital and further training of AME medical officers.
Co-location of the helipad with the level 3 hospital in Dili would allow specialists to be used on appropriate missions: For example, an Intensivist could be utilised for a head-injured patient or a trauma surgeon if a thoracotomy or amputation is possibly indicated. The current situation in Dili doesn’t allow specialists to be sourced and still meet launch times. There is also a considerable time delay in the transfer times. Future ADF hospitals should be co-located with the helipad.
AME medical officers should be trained to a higher level. The typical ADF medical officer only has two years of post-graduation experience with many having no anaesthesia or critical care exposure. A compulsory year as a senior critical care RMO would prepare the ADF medical officer for both peacetime and deployed role. This would need to be consolidated and maintained by three-month annual attachments to a retrieval service or trauma unit in a hospital. This will be difficult to achieve due to critical manning and poor retention of medical officers. Perhaps use of Simulation Centres such as the Royal North Shore in Sydney could provide combat and non-combat aeromedical retrieval scenario-based training to teams before deployment. Evidence suggests this is an invaluable tool in the preparation of ADF resuscitation teams for operational deployment’.
Currently, the ADF is exploring a doctrinal change of having a smaller medical footprint in the area of operations. A small highly qualified AME team would allow rapid evacuation and stabilisation of casualties. Is this the new role of the Emergency Consultant in the ADF? Could the Peace Enforcing mission in East Timor be supported by a level 2 facility in Dili with a more highly skilled AME team evacuating casualties to Darwin? We believe this should be a consideration given the fatigue starting to be demonstrated in the specialist reserve and the low workload often placed upon specialist reservists. The USAF has adopted this doctrine using CCAT (Critical Care Air Transport) teams with a focus of rapid evacuation and resuscitation with definitive treatment in the air’.
CONCLUSION
The ASF AME team provides a valuable service in support of the UN operation in East Timor and to the local people. It provides valuable experience and training to the ADF but attainment and maintenance of the skills required for the mission needs to be addressed. This is the perspective and experience of junior doctors and not ADF guidelines or doctrine. There is currently an AME Working Party chaired by the Director of Health Capability Development addressing these issues and planning the future capability of ADF AME.



