Abstract
These days, the world’s healthcare systems are facing the SARS-COV-2 pandemic and its associated disease, named coronavirus or COVID-19. This virus is a new human pathogen, and although there are many innovative vaccines, there are currently no specific treatment options.
In this study, we report a case with ambiguous clinical manifestation for COVID-19 pneumonia. The patient is a 32-year-old male F-14 pilot who went to the emergency ward with a dry cough, substernal pain and dyspnoea. His vital signs included the following: oral temperature of 38°C, blood pressure of 110/60 mmHg, heart rate of 105 beats/min, respiratory rate of 23 breath/min, and pulse oximetry of 88% on room air. He was admitted, and routine RT-PCR and CBC test were obtained. CXR and chest CT scan demonstrated bilateral lower lobe subsegmental atelectasis. COVID-19 pneumonia was ruled out, and due to a history of exposure to sustained high levels of acceleration with breathing high oxygen concentrations, acceleration-induced atelectasis was considered. Finally, the patient satisfactorily recovered by respiratory rehabilitation and N-acetylcysteine administration. COVID-19 presentations are very similar to different diseases and disorders, which may be confusing and delay treatment. The authors believe that their colleagues will be more careful in identifying and treating patients.
Keywords: SARS-CoV-2, COVID-19 pneumonia, Acceleration-induced atelectasis, Military pilot
Conflict of interest: None
Background
Today, the world is experiencing the coronavirus 2019 (COVID-19) outbreak with rapid transmission, possible complications and a high level of morbidity and mortality. COVID-19 needs early accurate diagnosis, systematised quarantine and closed follow up to reduce the transmission chain and recovery.1 Military aviators’ health is essential because they are the future of military aviation. Preparation for them to enter pilot’s training courses and deliver desired services in the form of expert military aviators requires extreme monetary and spiritual costs.2
History
The patient is a previously healthy, 32-year- old male military F-14 pilot who performed a 35-minute air combat manoeuvring training (ACM) flight. A few hours after landing, he went to the emergency ward with a dry cough, substernal pain (exacerbated by deep inspiration) and dyspnoea. He denied other symptoms, tobacco or medication use, significant past medical history and has not experienced acceleration atelectasis so far. His vital signs included the following: oral temperature of 38°C, blood pressure of 110/60 mmHg, heart rate of 105 beats/min, respiratory rate of 23 breath/min, and pulse oximetry of 88% on room air. Due to the coronavirus pandemic and clinical suspicion of COVID-19 pneumonia, he was admitted, and necessary laboratory and radiographic assessments were ordered.
Examination findings
Necessary laboratory assessments (related to COVID-19 infection) were requested, and their results are described in Table 1.
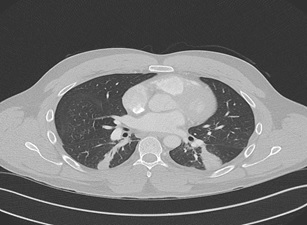
CXR and chest CT scan were ordered due to the pulmonary symptoms, which demonstrated bilateral lower lobe subsegmental atelectasis (Figure 1).
Table.1: Laboratory Findings
| Laboratory tests | Results | Reference range |
|---|---|---|
| RT-PCR test (nasopharyngeal specimen) |
Negative for SARS-CoV-2 (COVID-19) | – |
| Haematology | WBC = 7800/Cumm Lymphocyte = 35% RBC = 4.6 Mil/Cumm Hb = 13.8 gr/dl HCT = 41.9 % MCV = 91 fl MCH = 30.8 pg MCHC = 33.6 gr/dl RDW = 12.8 % Band = 3 % Platelet = 351000/Cumm TIBC = 428 g/dl Ferritin =178 ng/ml Iron (Fe) = 95 g/dl |
3500–10000 – 3.9–5.5 12–16 34.7–46.7 81–100 27–34 31.5–35.7 11.6–14.4 – 150000–450000 230–440 20–250 40–120 |
| Serology | CRP = 4.5 mg/L ESR = 13 mm FBS= 75 mg/dl |
Up to 8 2–20 70–99 |
| Biochemistry | Alk. Phosphatase = 55 U/L LDH = 246 U/L D-dimer = 100 ng/ml |
35–104 135–214 < 250 |
Figure.1: A) CXR represented symmetrical curvilinear opacities extending superolateral from the lower mediastinum bilaterally. They are separate to the oblique fissure on the lateral projection, most likely to be atelectasis. B) Axial chest CT scan shows bilateral lower lobe subsegmental atelectasis.
Special investigations
Laboratory and radiographic findings ruled out the clinical suspicion of COVID-19 pneumonia. However, due to his pulmonary symptoms, clinical and paraclinical findings and current history of exposure to sustained high levels of acceleration with breathing high concentrations of oxygen, acceleration (or G)- induced atelectasis was considered. The patient was encouraged to remain upright (to increase functional residual capacity [FRC]) and take as many deep breaths as possible. Administration of incentive spirometry, chest physiotherapy and N-acetylcysteine (600 mg orally every 6 hours for 3 rounds) greatly impacted recovery. Finally, after 48 hours of respiratory rehabilitation, the patient was discharged from hospital with a satisfactory clinical condition, but his return to flight education will be subject to further assessment by an air medical examiner (AME).
Discussion and conclusion
‘G-induced atelectasis’ is a resorptive and non- obstructive form of atelectasis produces during exposure to sustained acceleration (above about +3 Gz) when exposed to a high concentration of oxygen (for about 15 minutes) before using an anti-G suit. The condition can arise with an anti-G suit, but the severity of lung collapse is considerably less. As discussed above, the terminal airways of the basal alveoli close on exposure to +Gz acceleration so that ventilation of their alveoli ceases, although they continue to be well perfused. The closed airways will open again as soon as the exposure to acceleration ends and ventilation resumes. Since these non- ventilated alveoli are well perfused, gaseous exchange continues between the gas trapped in them and the mixed venous blood flowing through their septa. This blood absorbs the trapped gas from the alveoli at a rate limited by the rate at which the least soluble gas, usually nitrogen, is removed.4,5
There is a wide individual variation in susceptibility, both in the level and duration of acceleration required to produce atelectasis and the magnitude of the effect. The symptoms, which are usually not apparent until after exposure or even after the flight in which the exposure occurred, consist of a dry cough, with or without substernal discomfort or pain, exacerbated by deep inspiration. Chest radiographs reveal atelectatic bands at both lung bases (radiographic signs of collapse can occur in the absence of symptoms, but X-rays are not usually needed to manage the condition). Chest CT scan has a higher diagnostic sensitivity and often reveals dependent lung densities and loss of volume in the affected side of the chest. Atelectasis may also be directly visible with fibreoptic bronchoscopy and can be both diagnostic and therapeutic. The symptoms and radiographic signs are usually completely clear after changing position from supine to upright (increases FRC and decreases atelectasis), encouraging patients to take several deep breaths (which often provoke bouts of coughing), incentive spirometry, use of chest physiotherapy and a mucolytic agents (e.g. N-acetylcysteine). The mechanism behind all of these measures is a transient increase in transmural pressure that allows for the re-expansion of collapsed lung segments. In the absence of these interventions, however, basal collapse may persist for 24 hours or more.3,4
Based on the Federal Aviation Administration (FAA) guideline, civil pilots with a history of successful atelectasis treatment can return to flight with no signs or symptoms, normal pulmonary examination, and normal spirometry and radiography. However, according to the Royal Air Force (RAF) guideline, in addition to the above conditions, if the atelectasis and its underlying cause had been successfully treated without any recurrence, military pilots can also return to flight duties.4-6
COVID-19 presentations are very similar to different diseases and disorders (such as new-onset pulmonary sarcoidosis, acceleration atelectasis, etc.), which are themselves rare and worrying for military aviators. Subsequently, COVID-19 diagnosis can be confusing, leading to a delay in treatment.7 The authors believe that by studying this interesting rare case, their colleagues will be more careful in identifying and treating patients with COVID-19 presentations.
Ethical approval
The ethical approval of this study was issued by the Ethics Committee of the Aerospace and Sub- aquatic Medical Faculty in Aja University of Medical Sciences, with registration N# 10167121.
Abbreviations
Complete Blood Count —CBC
Reverse Transcription Polymerase Chain Reaction— RT-PCR
Functional Residual Capacity—FRC Air medical examiner—AME
Gravitational force from head to foot—+Gz
Contributors
1- Mohammad Darvishi, MD
The data collector and supervisor, statistical analyser and literary editor. (First Author)
2 – *Hamze Shahali, MPH. AME:
The main owner of the idea, scientific supervisor, executive author and editor. (*Corresponding Author)
Corresponding author: Hamze Shahali, hamze.shahali@ajaums.ac.ir
Authors: H Shahali1, M Darvishi1
Author Affiliations:
1 Aja University of Medical Sciences – Aerospace and Sub-Aquatic Medical Faculty