Introduction
Previous articles described the development of a cycle from prehistory to the end of the Napoleonic wars, whereby increasing seaborne trade necessitated larger and more efficient ships. This led to more and better weapons to defend or attack them, thereby creating further trading opportunities.1,2,3,4,5,6,7 While the technical developments in ships, weapons and medicine often developed independently in multiple regions worldwide, they remained especially closely linked throughout Western history. However, it was not until the 18th century that Western medicine had developed sufficiently for its role in facilitating this cycle to be recognised, thereby making possible the European colonisation of Australia.8
This article, chronologically the last of this series, describes the British developments in naval warfare, ships and medicine from 1815 to 1900.9
Victorian naval operations
By 1815, Britain had become the pre-eminent maritime power, dominating the world’s oceans over the next century. Strategically, this entailed a two-tiered navy, the first comprising battlefleets mainly operating in European waters. These were primarily based in Britain (in particular, Portsmouth, Plymouth and Chatham), which allowed them to blockade northern European ports or bring enemy battlefleets into action and attack their shipping, while defending their own. In addition, its bases at Gibraltar and Malta allowed Britain to likewise dominate the Mediterranean while also safeguarding the trade routes to its Indian, Far East and Australasian colonies (Figure 1).10
The second tier comprised a bevy of cruiser squadrons based worldwide, whose wartime role focused on attacking enemy and protecting British (including Australian) trade, the latter from commerce raiders that had evaded the battlefleet blockades or were themselves based overseas.11 Meanwhile, their peacetime role likewise entailed protecting merchant shipping, albeit through maritime law enforcement (especially against piracy) and hydrographic surveying. They also furthered British interests through ‘gunboat diplomacy’, such as suppressing the African slave trade and (less altruistically) using force to expand trade with China.12,13 These squadrons included an East Indies Station from 1744, which began detaching individual ships to Sydney from 1821, and a division thereof from 1848. This became a separate Australia Station from 1859 until the nascent Royal Australian Navy took over its warlike and peacetime functions in 1913. 14,15
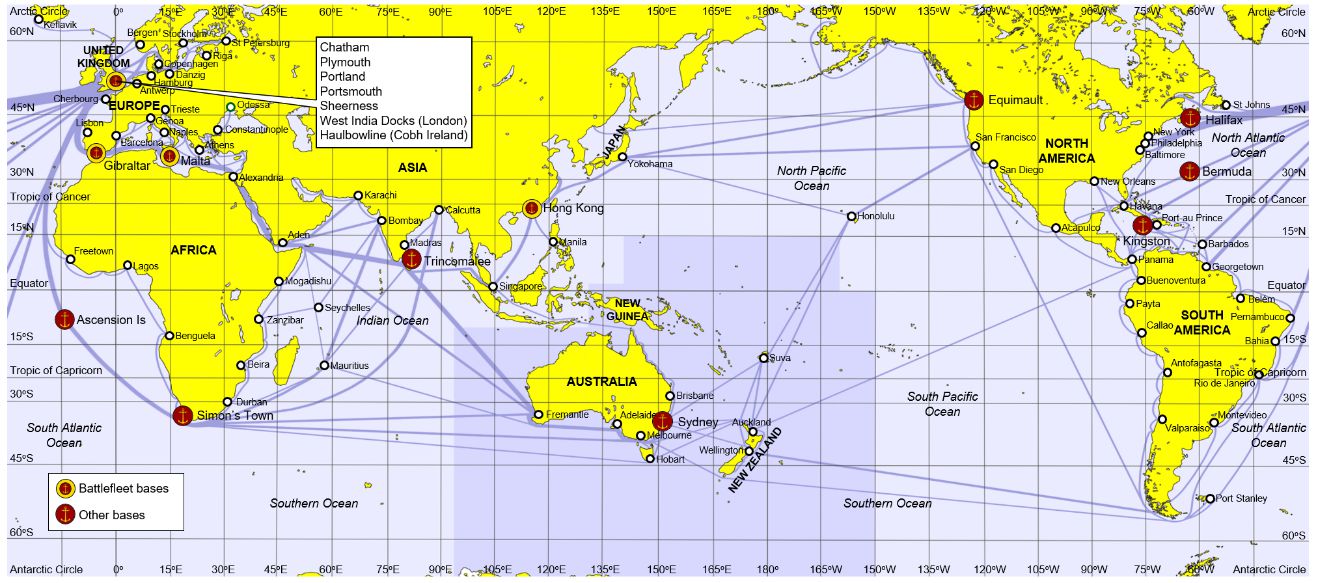
Figure 1. World shipping routes and RN bases, 1900.16,17 Note their general juxtaposition and the concentration of battlefleet bases in European waters (apart from Hong Kong, whose fleet was withdrawn after 1902). Also note the considerable size of the Australia Station (shaded), and the plethora of shipping routes requiring protection, either in wartime from commerce raiders or peacetime through maritime law enforcement and hydrographic surveying.
While the battlefleet bases each had large and comprehensive naval hospitals (Figures 2–10), the ships they supported had few opportunities to conduct major warlike operations. These were limited to a bombardment of Algiers in 1816 to suppress piracy and the Barbary slave trade; the Battle of Navarino in 1827 (the last to be fought exclusively under sail), which led to Greek independence from the Ottoman Empire; the 1853–56 Crimean War (which also entailed the RN conducting warlike if sometimes desultory operations in the Arctic, Baltic and Pacific); and the 1882 bombardment of Alexandria in Egypt, which ensured British control of the Suez Canal into the 1950s.18,19,20
Unlike the ships assigned to the battlefleets, those assigned to the overseas cruiser squadrons usually operated independently in remote locations for days or weeks at a time. This meant that they faced greater infectious disease risks and had more opportunities for combat, but with far less access to medical facilities ashore that could provide better care than on board.21 Furthermore, depending on each squadron’s size, their base medical facilities varied from small outpatient sickbays, inpatient sick quarters for low-acuity cases (as in Sydney, see Figure 11), to fully-fledged if still small naval hospitals supported by the local British Army or civilian medical services.
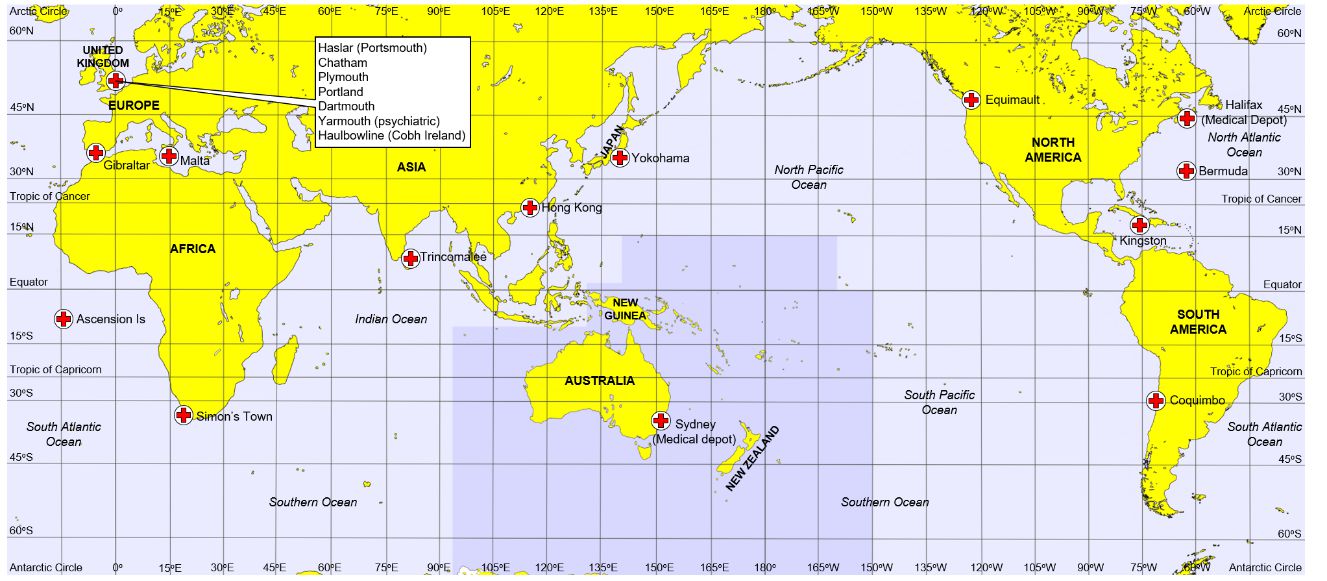
Figure 2. RN hospitals, sick quarters and medical depots, 1900. 22,23 Note their proximity to most (not all) RN bases (Figure 1), and (again) the considerable size of the Australia Station, especially regarding the absence of medical services ashore apart from the major Australasian urban centres. This explains why Sydney had a medical depot, in addition to its sick quarters, to fit out a hospital ship to accompany the local RN squadron in wartime.

Figure 3. Royal Naval Hospital Haslar looking east, undated (but probably 1960s); for orientation, see Figure 4.24 The largest brick-built building in Europe with 1800 beds on its completion in 1762; it was closed in 2008 and has since been converted into apartments.
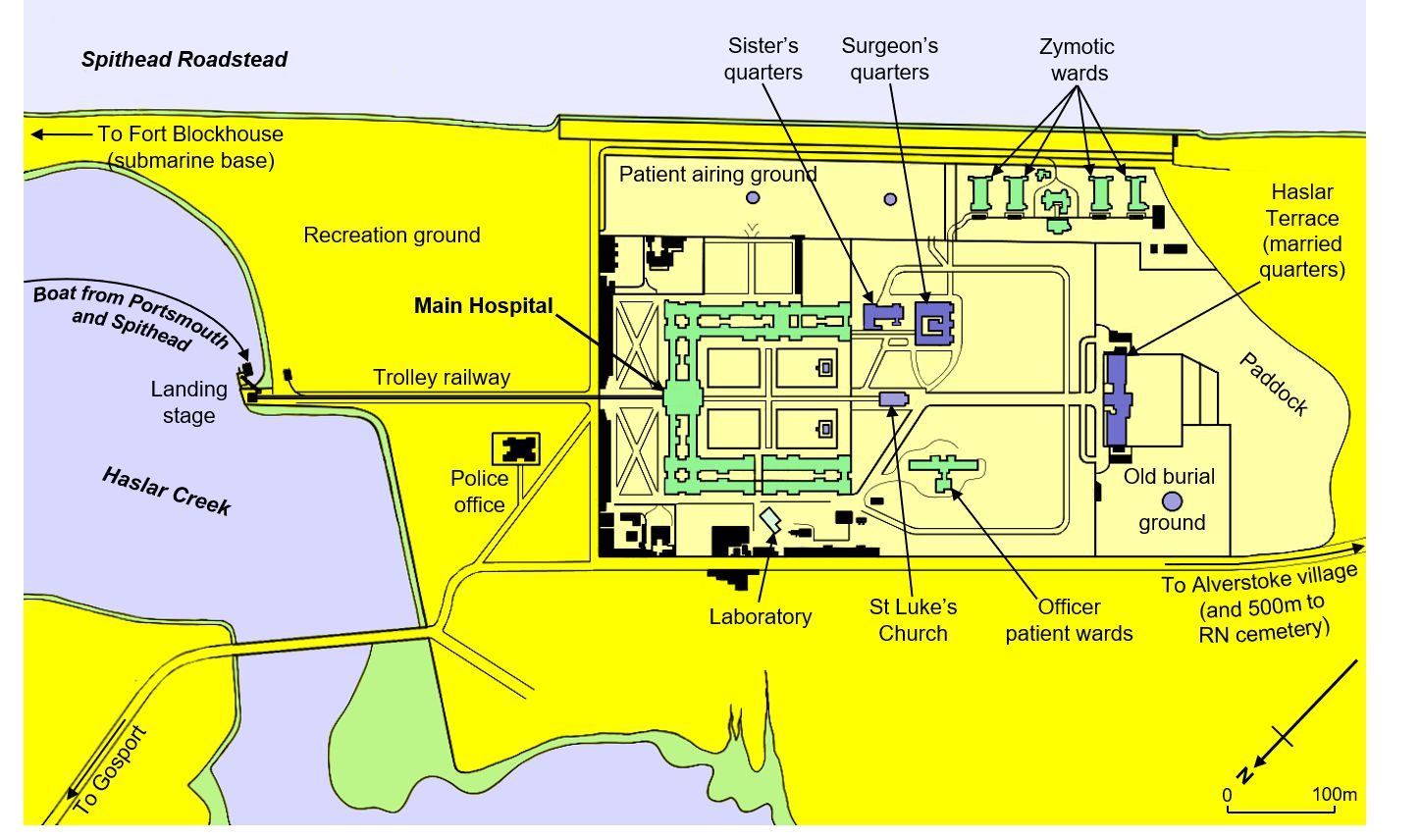
Figure 4. Plan, Royal Naval Hospital Haslar,1906.25 (see also Figure 3). Note its ready access to and from ships in Portsmouth Harbour and Spithead (but less so via overland); the trolley railway used to move casualties from the landing stage; the ‘zymotic’ (isolation) hospital … and the incredibly convenient on-site burial ground and paddock (together containing 8000–20 000 bodies, nearly all in unmarked graves) used from 1757 to 1826, and the proximity to the RN cemetery used thereafter.

Figure 5. Patients and staff, RN Hospital Haslar, pre-1905.26 Note the gas lighting, with all the ensuing risks from the alcohol, ether and other flammables used on the wards.

Figure 6. Operating theatre, RN Hospital Haslar, 1910.27 Until then, all surgery had been performed in the wards or side rooms. Note the bay windows to maximise lighting.
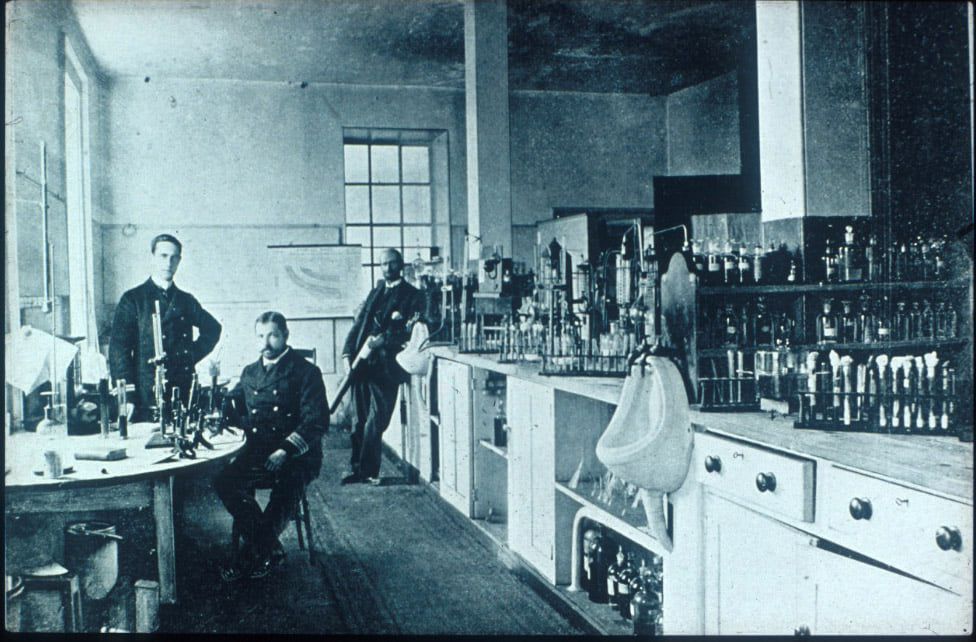
Figure 7. Laboratory, RN Hospital Haslar, pre-1896.28 Note the urinals: one hopes they were used for specimen disposal rather than collection.
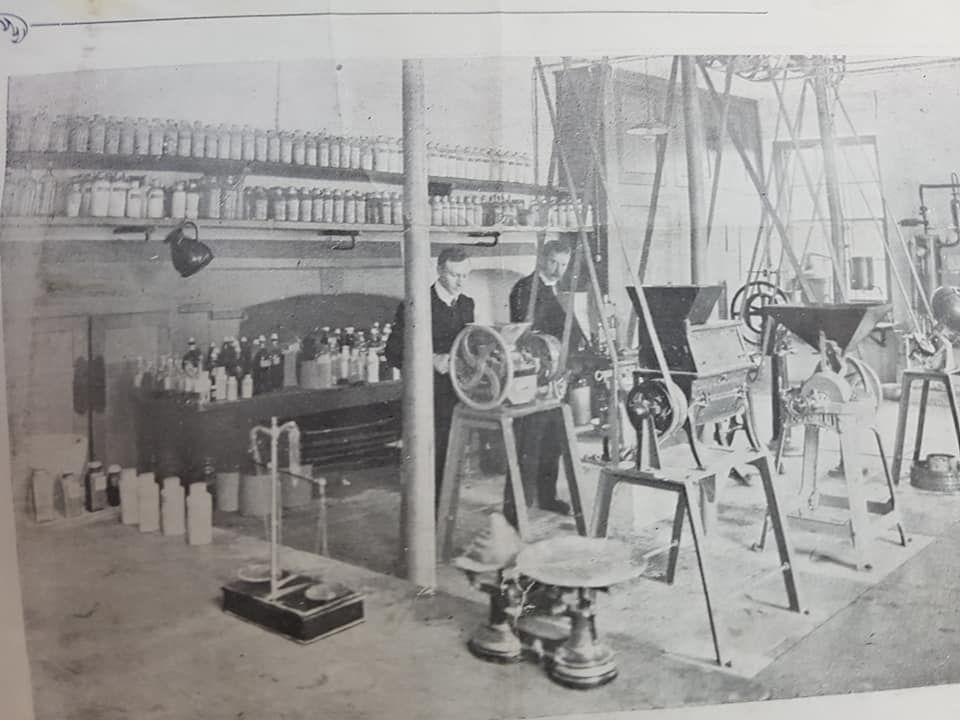
Figure 8. Pharmacy, RN Hospital Haslar, undated.29 Note the tablet-making machines and the absence of safety guards.
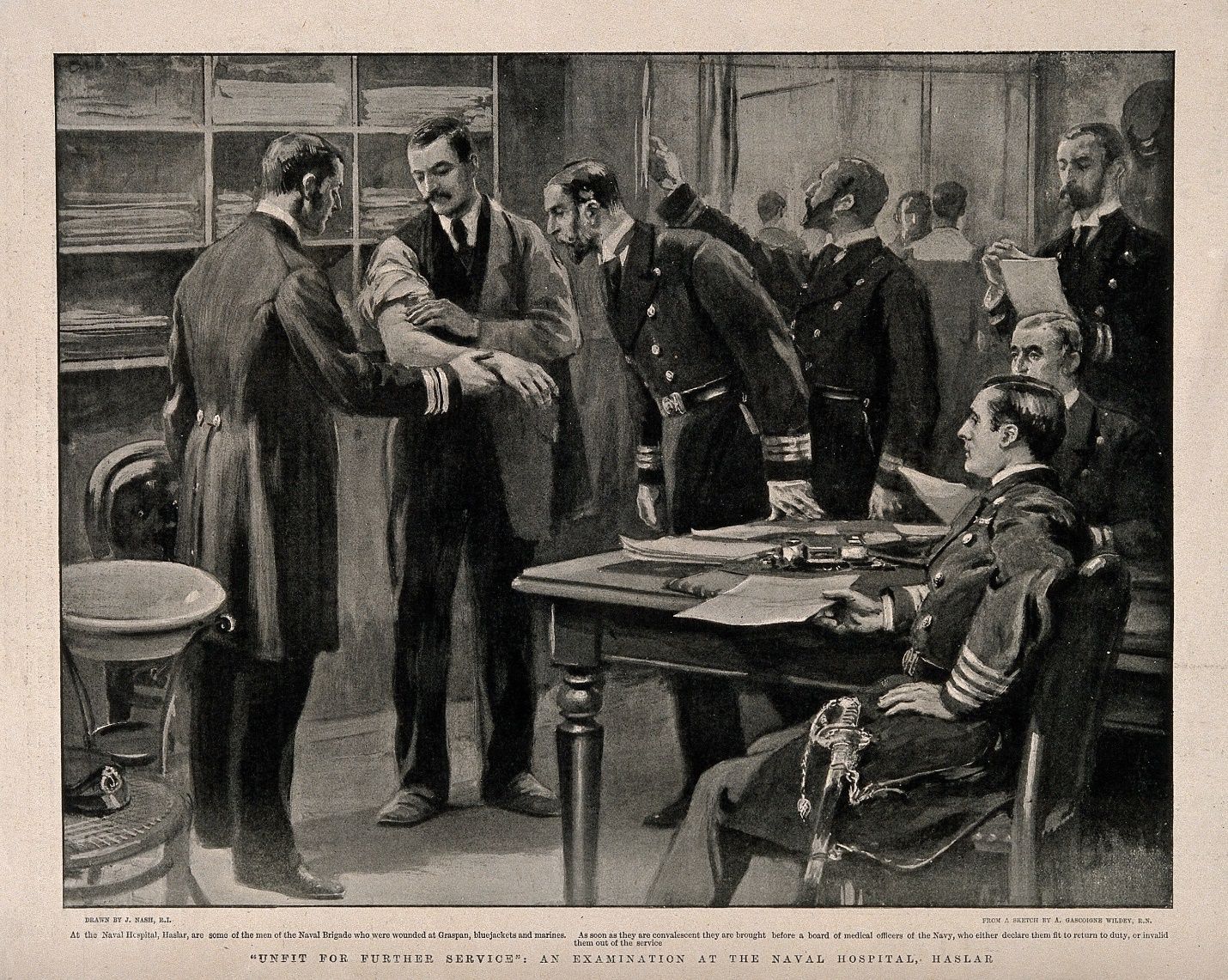
Figure 9. Patient (most likely a Royal Marine), undergoing a Board of Medical Survey (what would now in the ADF be called a Military Employment Classification Review), c.1900.30 Note the number of medical officers constituting the Board (and the mentoring opportunities created thereby); their level of clinical (not just administrative) engagement with the patient, and the formality of the process (as shown by their dress, and the sword worn by the Board President).

Figure 10. Ex-RN Hospital, Bighi Malta, c.2016.31 Built in 1832, this 260-bed hospital provided comprehensive health services for the RN’s Mediterranean Fleet until its closure in 1970. The site now houses the head office of Heritage Malta. For comparison with an overseas trade protection squadron base medical facility, see Figure 11.

Figure 11. View of the Garden Island Dockyard from the Sydney Domain, c.1900. This had a 13-bed sick quarters on half the top floor of the barracks building (circled), built in 1885.32 Note the contrast with Haslar and Bighi (Figures 2–10). This sick quarters was only used for xanthomatous and sexually transmitted disease cases, while higher-acuity patients were sent to local civilian hospitals (typically St Vincents or the Royal Prince Alfred). On taking over the dockyard in 1913, the RAN’s health services continued to use different parts of the building for various medical purposes until 1990.
Victorian ships
Other articles in this series describe how the development of ‘line-of-battle’ tactics in the mid-17th century led to warships differentiating into those with two or more gun decks that could take their place therein (hence ‘line-of-battle’ ships) and those with one gun deck known as ‘frigates’, which were fast enough to act as fleet scouts, and large enough to attack enemy merchant shipping or defend their own independently.33,34,35 By 1815, the smallest ‘line-of-battle’ ships carried 70 to 80 guns compared to 50 to 60 a century earlier, while their gun sizes had also increased; for example, frigates typically carried nine-pounder guns in 1714, but 18- or even 24-pounders a century later.36,37 These increases required larger ship crews, from around 300 men for 50-gun ships in the 1710s to 550 men for 74-gun ships after the 1780s. The overall number of ships also expanded from around 250 in 1714 to over 900 in 1815.38 Combined with their larger size allowing these ships to stay longer at sea, these considerations acted synergistically to pose progressively greater wartime challenges for the RN—including its medical services—in getting its ships to sea and keeping them there.
Even so, it is indicative of Britain’s peacetime maritime supremacy that it could be sustained with only 20 000 to 60 000 men for 250 to 300 commissioned ships between 1815 and 1889 (Figure 12), with a level of security that eventually even precluded merchantmen having to arm themselves. The ensuing absence of weaponry aboard the latter begat the differentiation between naval and merchant seamen, who heretofore had been generally interchangeable. This, among other factors, led to serious manning shortfalls during the Crimean War, which drove substantial changes to RN sailors’ conditions of service, such as the introduction of 12- and 10-year ‘continuous service’ engagements that finally gave them permanent naval careers.39 In addition, the RN Reserve was formed in 1859, comprising merchant seamen who had volunteered for periodic naval training, followed in 1902 by the RN Volunteer Reserve (RNVR) for personnel who volunteered for call-up but had no peacetime training liability. The RNVR included medical officers (and dental officers after WWI) and a separate Royal Naval Auxiliary Sick Berth Reserve based on the St John Ambulance.40,41
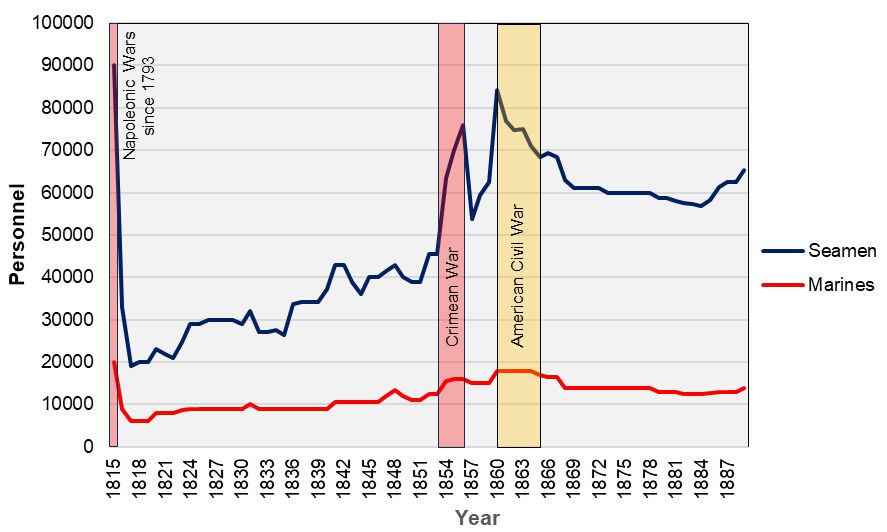
Figure 12. RN personnel requiring medical support, 1815–1889.42 The two main peaks coincided with the RN’s participation in the Crimean War (1853–56) and preparations for a potential conflict with the United States during the American Civil War (1861–65). The increase in seaman (including trainee) personnel most likely reflects the introduction of continuous service from 1853, which augmented the number ashore awaiting their next ship. It should also be noted that nearly all RN ships had a Royal Marine component for gunnery and infantry duties afloat and ashore as part of their complements. A naval arms race after 1889 led to an increase to about 133 000 RN seamen/trainees and marines by 1913.43
Although their primary roles remained unchanged, the RN’s ships underwent greater technological development during this period than in 300 years. Having further increased their size to 100 or even 120 guns, the first steam-powered wooden ‘line-of-battle’ ships began entering service during the 1850s (Figure 13), while the development of larger guns firing explosive shells led to the first British-built ironclad Warrior entering service in 1860 (Figure 14).44 Subsequent developments saw the abandonment of sail in lieu of increasingly efficient steam engines; the evolution from wooden to iron, then iron-backed steel ‘compound’ and finally all-steel armoured hulls; and progressively smaller numbers of increasing larger muzzle- and then breech-loading main-armament guns.45,46 By 1890, these developments had led to the first 16- to 18-knot reciprocating-engined multicalibre ‘pre-dreadnoughts’, followed in 1906 by the first 21-knot turbine-driven all-big-gun ‘dreadnought’ battleship (Figures 15–18).
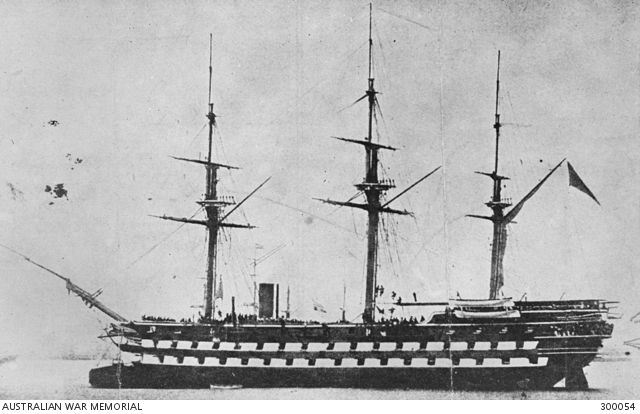
Figure 13. HMVS Nelson (2617 tons, c.820 crew, completed 1814) c.1870–1879.47,48Initially built as one of the last British ‘line-of-battle’ sailing ships, with 126 guns on three decks, she was cut down to two decks and given a steam engine in 1860. However, Nelson herself never entered RN service, instead being transferred in 1865 to the Victorian Naval Forces as a harbour training ship. Similar ships carried at least one surgeon, two surgeon’s mates and, from 1832, at least three ship’s company members to act as semi-trained sick berth ‘stewards’.49

Figure 14. HMS Warrior (9137 tons, 707 crew, completed 1861), 2009.50,51As the first British-built ironclad warship, she is the ancestor of all RN battleships that served over the next century. She likewise carried one surgeon, two surgeon’s mates and probably three ship’s company members to act as semi-trained sick berth ‘stewards’.52
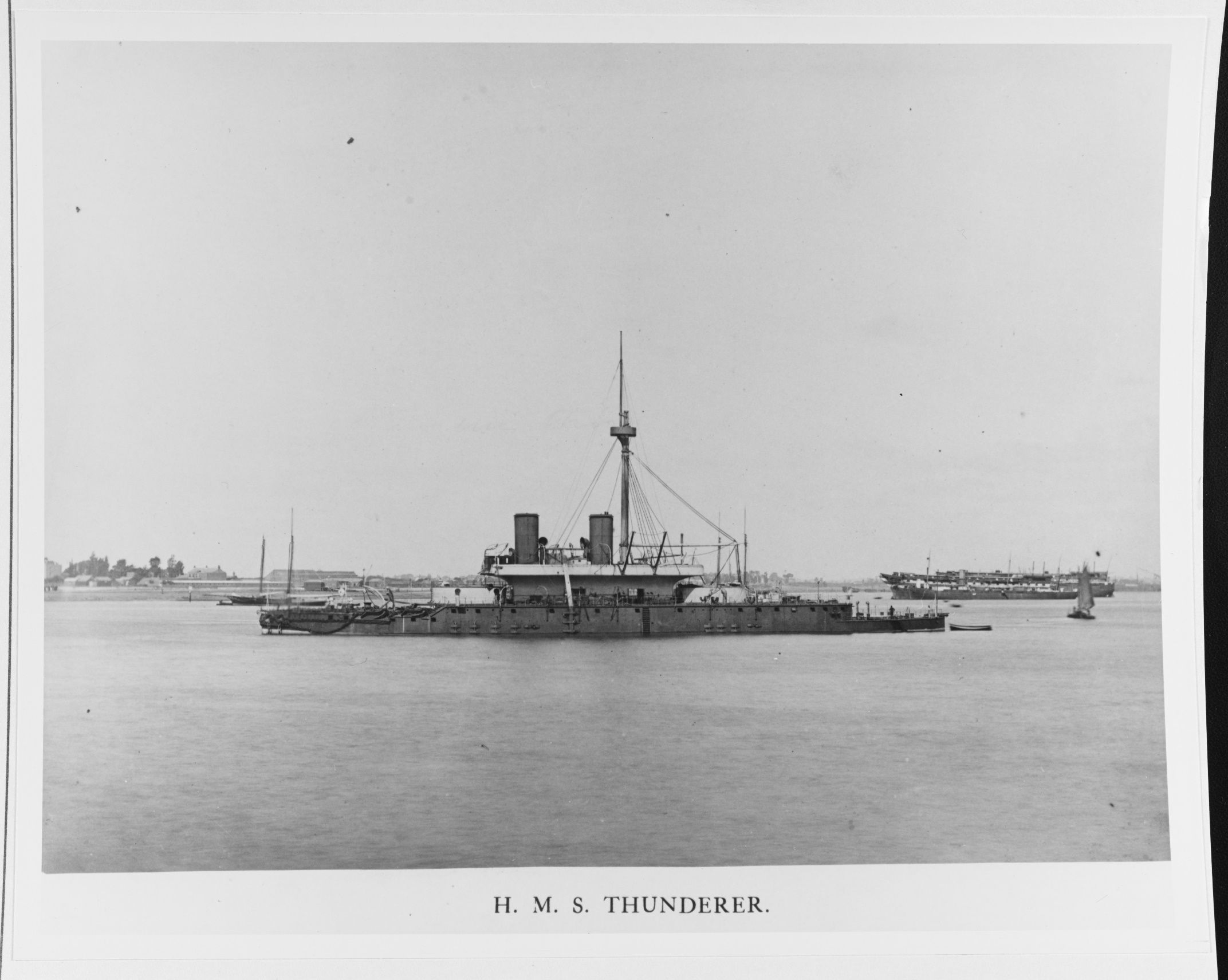
Figure 15. HMS Thunderer (9330 tons, 358 crew, completed 1877), c.1879.53,54 She and her sister Devastation were the first battleships designed to operate without sails, for which HMVS (later HMAS) Cerberus (3344 tons, 155 crew, completed 1870) had rather acted as a one-third-scale prototype.55 Both ships carried two surgeons and probably two ship’s company members to act as semi-trained sick berth ‘stewards’ (see also Figures 21 and 22).56

Figure 16. Ironclad battleship HMS Inflexible (11 880 tons, 440 crew, completed 1881), c.1881–1885.57,58 This ship represents the pace of technical development during this time, which often rendered ships obsolete on entering service – in Inflexible’s case, her sails (10 years after Cerberus), iron armour and muzzle-loading guns in en echelon midships turrets. Inflexible also carried two surgeons and, probably, up to three sick berth ‘stewards’.59

Figure 17. Majestic-class battleship HMS Magnificent (14 890 tons, 672 crew, completed 1895). 1899.60,61 These and her successors formed the backbone of the RN battlefleets (which precluded their service in Australian waters) from the early 1890s until HMS Dreadnought entered service in 1906 (Figure 18). These carried two surgeons (three in flagships) and three trained sick berth attendants.62,63
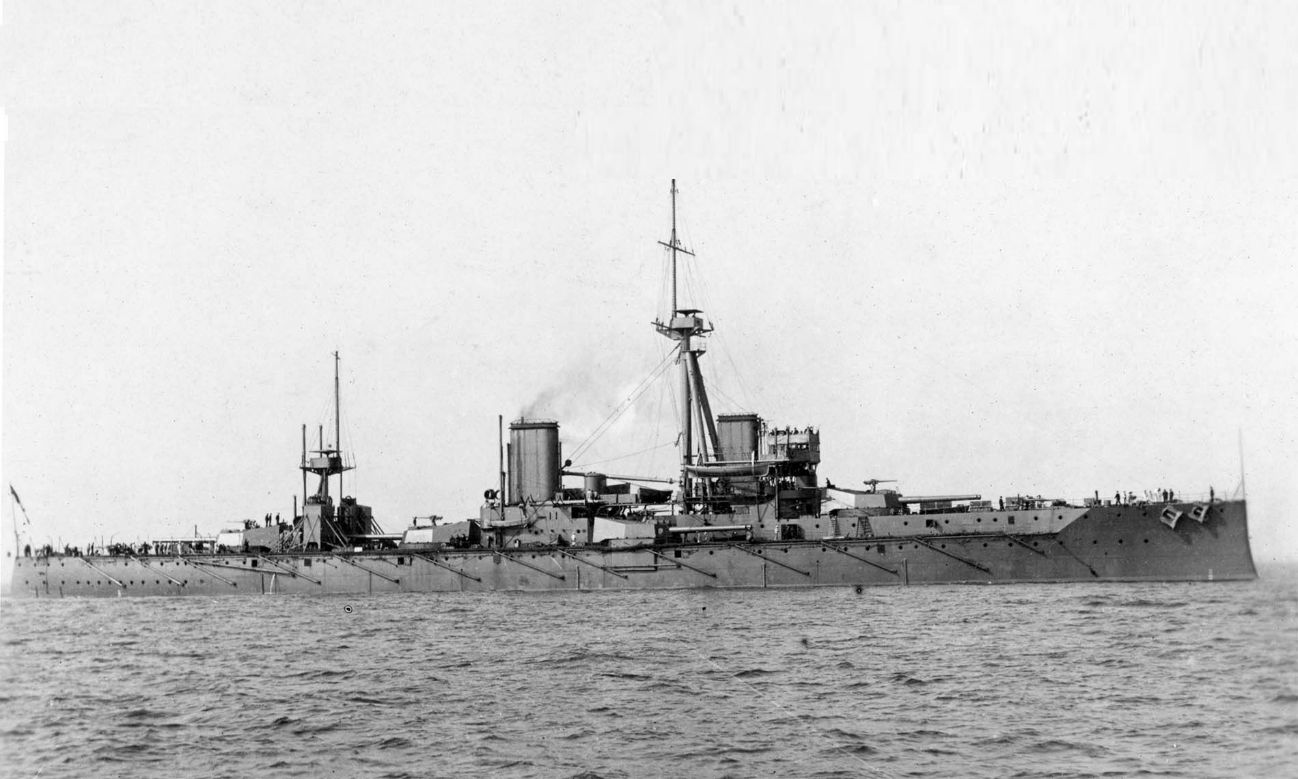
Figure 18. Battleship HMS Dreadnought (17 900 tons, 695 crew, completed 1906), c.1908–1911.64,65 She and her successors formed the backbone of the RN battlefleets until WWII, which also mostly precluded their service in Australian waters. These ships also carried two medical officers (three in flagships) and three sick berth attendants, with a civilian dentist from 1915, thence a RNVR dental officer from 1917.66,67,68
These developments also introduced new shipboard hazards (Figures 19–20); for example, electricity in the battleship Inflexible in 1881 (Figure 16) inevitably led to the RN’s first death by electrocution. These ships had comprehensive sickbays, typically with up to three medical officers and three sick berth staff (Figures 21–23).
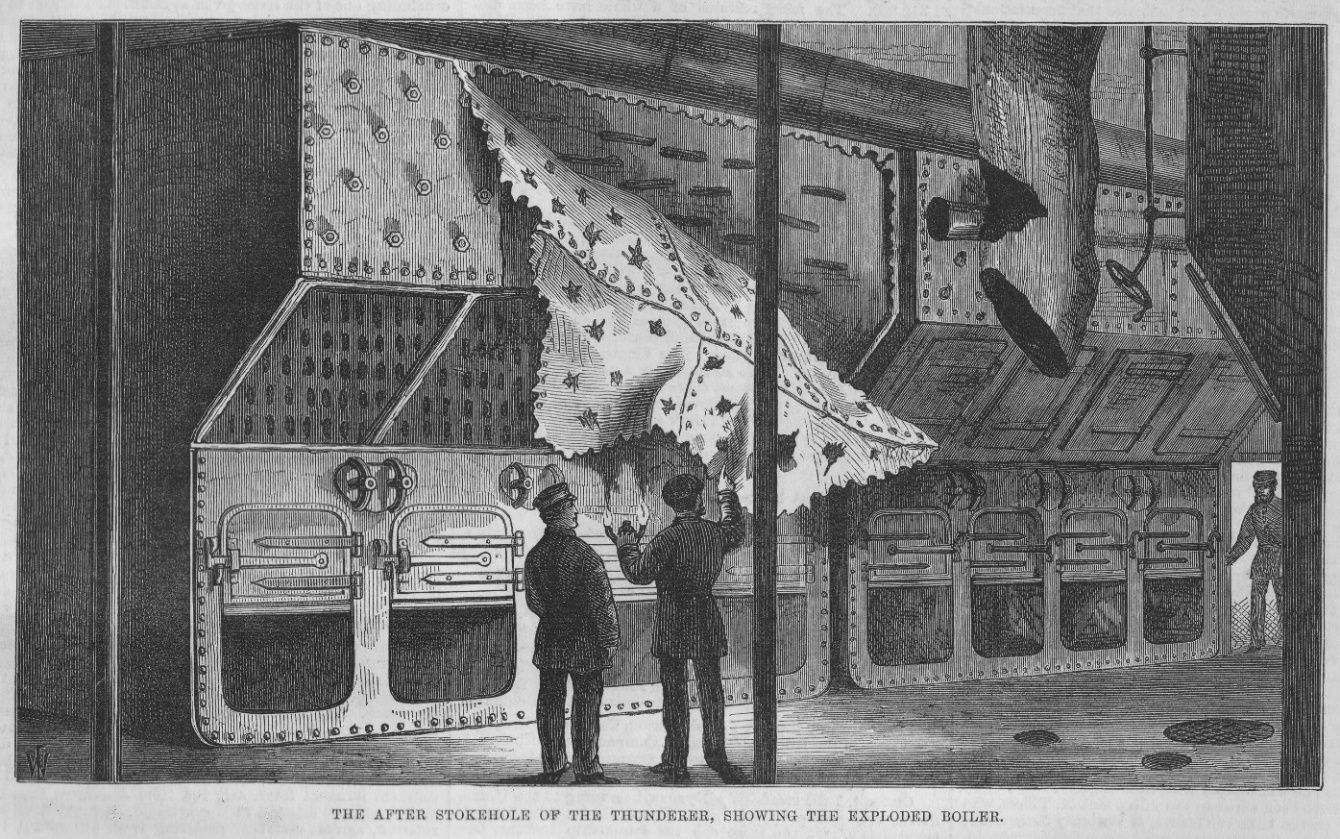
Figure 19. Boiler room damage, HMS Thunderer, July 1876. The accident was ascribed to a faulty safety valve, which killed 15 and injured 70 men, 30 of whom later died.69 Cerberus’s boilers were generally identical in design (see also Figure 32).
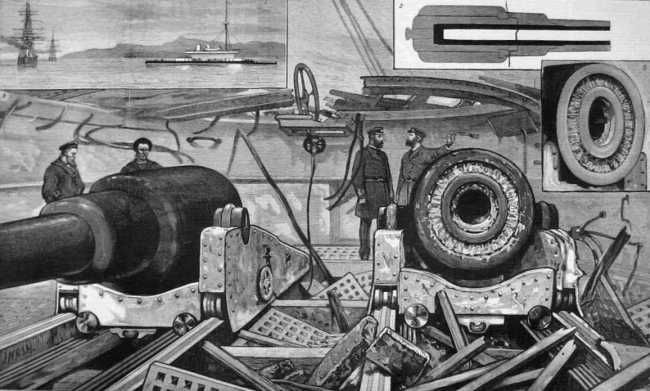
Figure 20. Gun explosion damage, HMS Thunderer, January 1879. This accident was ascribed to loading the gun (a muzzle-loader) twice, killing 11 men and injuring 35.70Apart from their smaller size (254 rather than 305 mm), Cerberus’s guns were generally identical (see also Figure 32).

Figure 21. Sickbay HMS Warrior (author, 2022). Note the glass topped operating table (easier to clean than wood before the use of stainless steel), the small stove used for heating and preparing special diets, and the swinging cots for patients. Also note the overhead black iron bars: these were used by the ship’s sick berth attendants to sling their hammocks, thereby sharing their living space with their patients at least into the 1940s.

Figure 22. Dispensary HMS Warrior, (author, 2022).

Figure 23. Surgical instrument set aboard HMAS Warrior, originally owned by Surgeon Adrien Forrester RN (author, 2022). Forrester served on the Australia Station aboard the survey schooner Dart from 1901 to 1904, followed by the third-class cruiser Pyramus from 1907 to 1911. He died while serving in the pre-dreadnought battleship HMS Implacable on 25 April 1915 off Gallipoli.
Meanwhile, the invention of the locomotive torpedo in 1866 led to small and fast ‘torpedo boats’ during the 1870s and 1880s, which were countered and then replaced by ‘torpedo-boat destroyers’ (later just ’destroyers’) from the 1890s (Figure 24). Their small crews and limited range meant they only needed medical support from their harbour depot ships or alongside until after WWI.71

Figure 24. One of the first ‘torpedo-boat destroyers’, HMS Daring (288 tons, 46 crew, completed 1895), 1897.72,73 Her small size and high speed (26 kts) reflected their primary role of making night torpedo attacks on enemy battlefleets or defending against them. Combined with their short range and limited seakeeping, these roles precluded their use in Australian waters until the 1910s.
The period from 1815 also began with the sail- (and later steam-) driven frigates continuing to be used interchangeably for battlefleet scouting and overseas trade protection. The latter typically entailed these ships acting as squadron flagships for the smaller, if rather eclectically-designated sloops, gunboats and other craft (Figure 25) that undertook surveying, law enforcement and other peacetime roles. By the 1880s, the steam frigate’s ‘cruizer’ trade protection role had been subsumed by three classes of steam-driven ‘cruisers’ (Figures 26–29), which had higher speed and longer range than battleships at the expense of thinner armour and smaller guns. The RN’s first-class ‘armoured’ cruisers were rendered obsolete in 1907 by the ‘battlecruiser’ HMS Invincible (Figure 30), and the third-class ‘protected’ cruisers likewise by their small size and limited speed and armament, leaving the second-class cruisers to evolve into the ‘light’ cruisers used during the World Wars. Their extended operations in remote areas meant that, like the battleships, cruisers had well-equipped sickbays, with up to three medical officers and three sick berth staff, depending on their size.
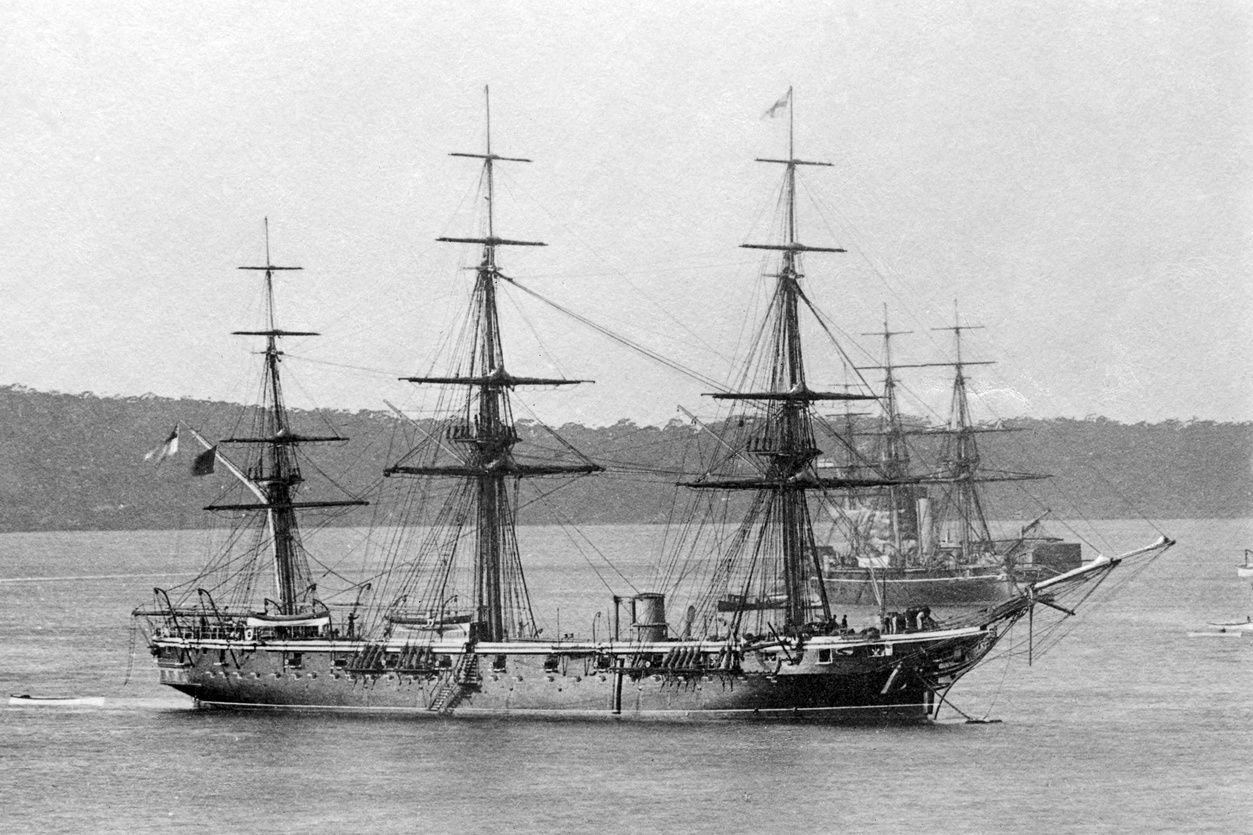
Figure 25. Jason-class wooden screw corvette HMS Wolverene (2424 tons, 240 crew, completed 1864) at Sydney, 1881.74,75 The RN used this type of ship in its smaller overseas squadrons as flagships, wartime commerce protection and peacetime maritime law enforcement, typically in remote areas without shore-based medical support. As the Australia Station flagship from 1875 to 1882, Wolverine had a sickbay with two medical officers and, probably, two semi-trained sick berth ‘stewards’.76 Her sister Orpheus was wrecked off Auckland while performing the same role in 1863, with the loss of c.166 lives, including the Commander Australia Station, Commodore Sir William Burnett.77

Figure 26. Iron armoured frigate HMS Nelson (7473 tons, 560 crew, completed 1881) undated.78,79The RN used this type of ship in its overseas squadrons as flagships, wartime commerce protection and peacetime maritime law enforcement, typically in remote areas for which Nelson still required sails. To these ends, as the Australia Station flagship from 1882 to 1889, she had a sickbay with two medical officers and, probably, up to three sick berth attendants.80
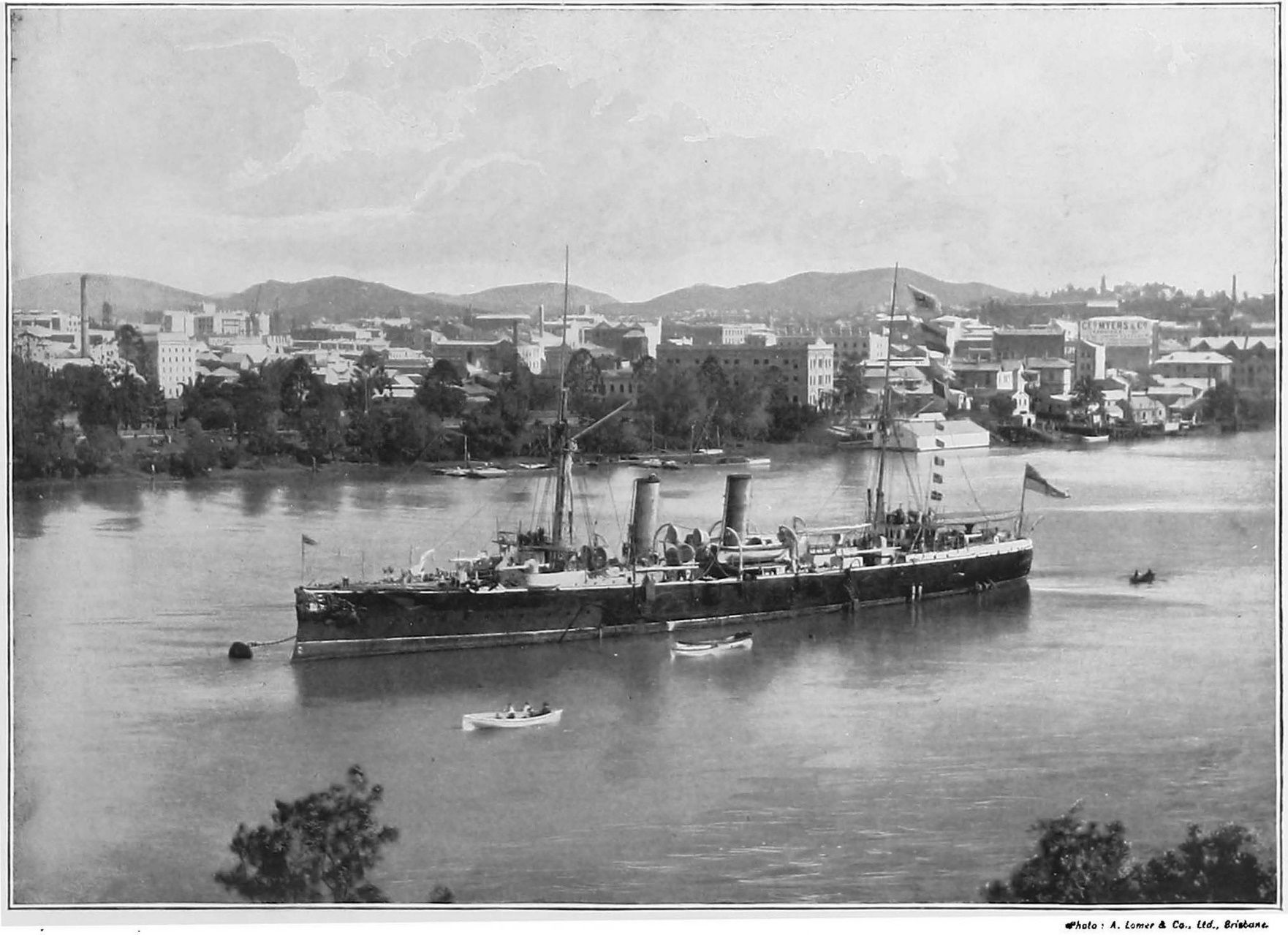
Figure 27. Third-class protected cruiser HMS Wallaroo (2575 tons, 217 crew, completed 1890) at Brisbane, c.1897–99.81,82 The RN used these smaller cruisers in its overseas squadrons for wartime commerce protection and peacetime maritime law enforcement, for which Wallaroo had a sickbay with a medical officer and a sick berth attendant.83,84

Figure 28. Second-class protected cruiser HMS Cambrian (4360 tons, 318 crew, completed c.1894), c.1894-1902.85,86Note her intermediate size compared to third- (Figure 27) and first- (Figure 29) class cruisers, which gave greater capability than the former at considerably less cost than the latter. The RN used this type of ship in wartime for battlefleet scouting and its overseas squadrons as flagships and/or wartime commerce protection, typically in remote areas without shore-based medical support. As the Australia Station flagship in 1912-13, Cambrian had a sickbay with two medical officers and two sick berth attendants.87,88

Figure 29. First-class protected cruiser HMS Powerful (14 200 tons, 894 crew, completed 1898), c.1898-1902.89,90 Note her size (comparable to a pre-dreadnought battleship, see Figure 17) to ensure high speed and long range at the expense of armour and armament. The RN used this type of ship in wartime for battlefleet scouting, and in its overseas squadrons as flagships and/or wartime commerce protection, typically in remote areas without shore-based medical support. As the Australia Station flagship from 1905 to 1912, Powerful had a sickbay with most likely three medical officers and three sick berth attendants.91,92
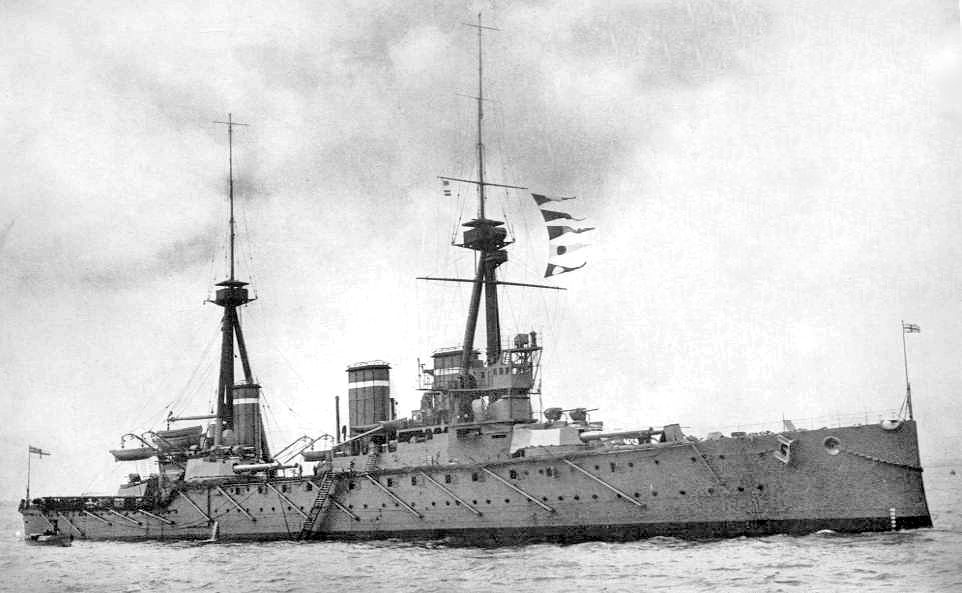
Figure 30. Battlecruiser HMS Invincible (17 250 tons, 784 crew, completed 1907), c.1907–1916.93,94 Note her similarity to Dreadnought apart from the same but fewer main-armament guns, the extra funnel indicating extra engine power and the hull scuttles (portholes) indicating less armour, all for greater speed. The RN used this type of ship for battlefleet scouting and commerce protection, resulting in HMAS Australia (based on the Invincible design) becoming the RAN’s first flagship from 1913. To these ends, she had a sickbay staffed in peacetime by two medical officers and four sick berth attendants, with a Permanent List dental officer from April 1918 (11 months before the RN followed suit).95,96
Meanwhile, although many of the smaller overseas squadron ships gained steam propulsion as early as the 1840s, their extended periods at sea in remote locations meant that they often retained sails into the 1890s and beyond (Figure 31). Unlike the battlefleet’s torpedo-boat destroyers, it was their remote operations rather than crew numbers that necessitated small sickbays for a medical officer and perhaps at least one attendant.

Figure 31. Steel sloop HMS Torch (960 tons, c.106 crew, completed 1894), c.1900.97,98 Note the sail rig (despite her construction 30 years after Wolverine, see Figure 25), giving her long range in remote areas. The RN used this type of ship in its overseas squadrons for peacetime maritime law enforcement and hydrographic surveying. Torch had a small sickbay with a medical officer and (one would hope) a sick berth attendant.
Victorian naval medicine
Medical advances
As for the RN’s ships, the Victorian period saw the greatest changes in medical and surgical practice, albeit over the previous 1600 years rather than 300.
Previous articles in this series explained how Western medicine before the 1850s was based on a ‘humoural’ disease theory first described in the Greek Corpus Hippocraticum between 323 and 31 BCE.99 This was expanded by Galen of Pergamon (129–c216 CE), whose pre-eminence impeded further meaningful medical research for the next 1300 years.100,101 Although effective surgical treatments for uncomplicated cuts, abrasions and limb fractures had been developed by the Egyptians as early as c2000 BCE, further surgical progress was impeded by Galen’s anatomical and physiological errors, and the absence of effective analgesia and anaesthesia. As a result, even minor wound complications had high morbidity and mortality rates, while penetrating head, spinal, chest and abdominal injuries remained almost universally fatal.102
The first cracks in humoural medicine began with the 16th-century studies by Ambroise Paré, Andreas Vesalius and William Harvey, who, among others, were aided by fewer restrictions on cadaver dissection and the ability to publicise their findings by the invention of moveable-type printing.103,104,105,106,107However, progress remained slow until 1847, when, in response to disparate mortality rates between two maternity wards at the Vienna General Hospital, Ignaz Semmelweis directed his medical students to wash their hands between their autopsy studies and ward duties. Six years later, John Snow demonstrated that a cholera outbreak in Soho, London, emanated from a Broad Street water pump. By the 1860s, Louis Pasteur had identified bacteria as the causative agents which initiated the current ‘germ’ theory of disease.108
Examples of subsequent militarily-relevant research include the identification of the gonorrhoea diplococcus by Albert Neisser in 1879, the tuberculosis bacillus by Robert Koch in 1882, the syphilis spirochaete by Fritz Schaudinn and Erich Hoffmann in 1905, and the rickettsia (typhus) bacillus by Henrique da Rocha Lima in 1916. These discoveries extended beyond bacterial infections when Charles Laveran identified the malaria parasite in 1880, while Ronald Ross ascertained its lifecycle and transmission via the Anopheles mosquito in 1897. Although infectious diseases such as yellow fever had first been labelled as ‘viral’ in 1892, Edward Jenner had already used the cowpox virus to prevent smallpox in 1796 (a discovery quickly taken up by the RN from 1800), while Pasteur had developed the first vaccine to contain an attenuated live version of a previously dangerous virus in 1885, to prevent rabies. From an RN perspective, perhaps the most dramatic advance pertained to identifying the cause of ‘Malta fever’ (brucellosis), which reduced incidence rates in the Mediterranean Fleet from 1.89% in 1903 to 0.07% in 1907.109,110,111,112,113
Pasteur’s research also quickly led to the surgeon Joseph Lister using carbolic acid to disinfect surgical instruments and clean dirty wounds, while further work by Lawson Tait and William Halstead led to the realisation that the key to effective surgical wound care entailed preventing them from becoming infected in the first instance.114 However, it was not until 1901 that it began to be understood that this meant all dead tissue—as found in gunshot and shrapnel wounds—had to be debrided rather than simply disinfected; even then, it only entered mainstream surgical practice after three years of what Arthur Graham Butler called an ‘orgy of human vivisection’ during WWI.115
This realisation became particularly important for treating burns, which had been based on various salves of dubious efficacy since Egyptian times (Figure 32). However, although Guillaume Dupuytren first recognised deaths from the fluid loss associated with large burns in the 1830s, it was only in 1897 that Pierleone Tommasoli used intravenous saline for fluid replacement, while skin grafting did not become accepted practice until after WWI.116
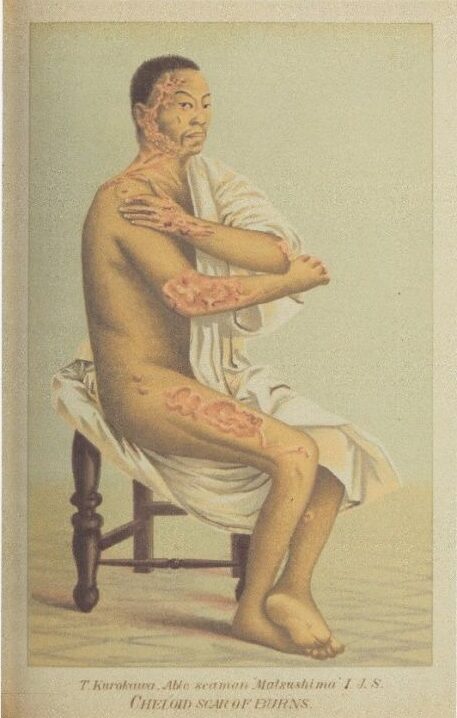
Figure 32. Burns case from a shell hit on the Imperial Japanese Navy (IJN) Ship Matsushima, during the Battle of Yalu River with the Imperial Chinese Navy on 17 September 1894.117 Following its formation in 1871, the IJN based itself on the RN (including its medical services) until after WWI. Note the extensive keloid formation, reflecting the contemporary state of burns treatment. See also Figures 19 and 20.
Throughout the Galenic period, patients had been tormented at least as much by their treatment as by their illness or injury. Although opium poppies had been used since antiquity as an analgesic, cough suppressant and anti-diarrhoeal agent, their active agent, morphine, was not isolated until 1804, while the anti-inflammatory agent in willow bark was first synthesised in the form of aspirin in 1899. Following their use as party drugs since the 1790s, ether and nitrous oxide were widely publicised as general anaesthetic agents in 1846, followed by chloroform in 1847. After its isolation from the Peruvian coca plant in 1855, cocaine was first used as a topical anaesthetic for eye surgery from 1884 and as a spinal anaesthetic from 1898. Together, these developments alleviated the more egregious forms of patient suffering and, combined with effective post-operative wound care, led to a surgical revolution that was further enhanced when Wilhelm Röntgen discovered X-rays in 1895.118,119,120,121,122,123
The most important medical advances for the RN pertained to naval hygiene, which reduced mortality rates from 2.58% in 1858 to 0.32% in 1913 (Figure 33). To this end, steam power was instrumental, first and foremost by facilitating better ventilation via powered fans to supply trunked ‘punkah louvre’ forced drafts into engine and boiler rooms and other spaces lacking open-air access.124 However, although this also facilitated heating the ship’s accommodation in cold climates, it was not until after WWII that the RN gave comparable attention to cooling the same spaces in hot climates through air conditioning. Furthermore, the residual role of ‘miasma’ as part of the humoural theory of disease led to considerably detailed yet medically nugatory meteorological reporting in ship’s medical journals into the 1890s.
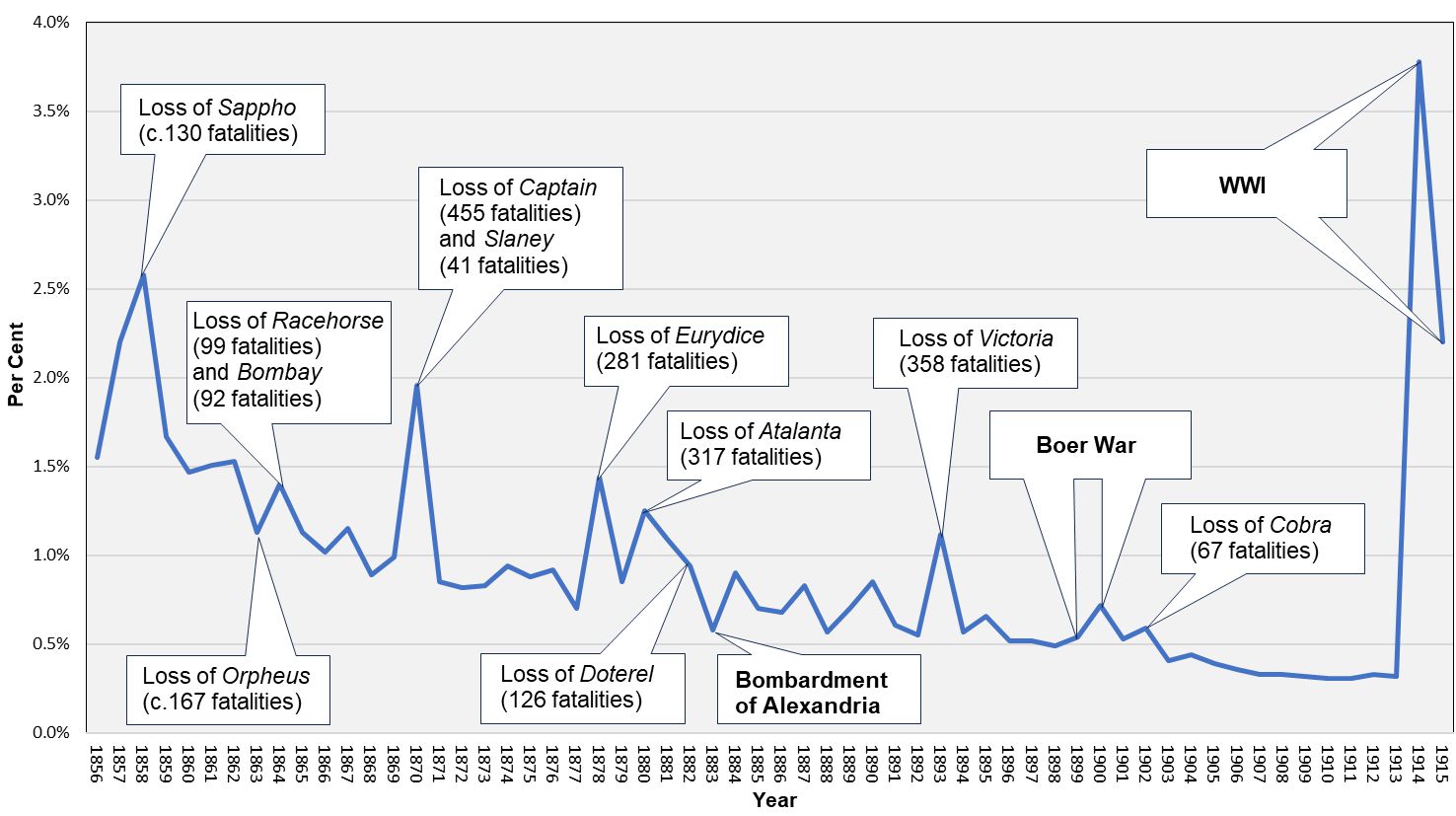
Figure 33. RN mortality rates, 1856–1915.125,126,127 Note the gradual decline during this period, with the larger peaks often (but not always) reflecting ship losses with large fatality numbers (Sappho and Atalanta were lost with all hands while Eurydice had only two survivors). This graph, therefore, illustrates how RN mortality rates reflected the improvements in naval hygiene and the extent to which the sea posed a greater perennial threat than any human enemy. The smoothing out of the graph from 1904 coincides with the identification and prevention of Malta fever (brucellosis).
Steam power also allowed ships to distil their own (albeit still highly rationed) fresh water, which could be stored in the iron tanks that replaced wooden casks after 1815. Besides reducing their reliance on at times dubious sources ashore, readily-available hot water improved personal hygiene through hip- and then plumbed baths for senior officers and ‘bird-bath’ washbasins for the rest of the ship’s company (Figures 34 and 35).128 However, it was not until after the 1930s that RN ships had showers, and even then, limited fresh water supplies led to 90-second ‘wet-and-soap on / wash / rinse-and-soap-off’ ablutions into the 1990s (and sometimes beyond). Meanwhile, although Warrior had the first seagoing laundry (Figure 36), this was only for engineering sailors and others with dirty jobs, with the rest of the crew using individual ‘dhoby buckets’ into the 1950s (Figure 37).


Figures 34 and 35. Officer’s cabin washbasin unit, ex-battleship Iron Duke (commissioned 1914) Lyness Museum (author, 2022). RN ships had surprisingly elementary piped freshwater systems even as late as WWI. This led stewards to carry cans of hot water every morning to each officer’s cabin to fill the basin seen here. On completing their ablutions, the officer closed the cabinet, thereby emptying the basin into the tank below for removal by the steward. Meanwhile, the crew shared multiple such basins, which may or may not have had piped outlets. Although an improvement for the latter compared to the sailing ship era, these somewhat sketchy hygiene arrangements often endured into WWII.

Figure 36. Laundry, HMS Warrior (author, 2022). Dirty clothes and soap were put in the hexagonal boxes and rotated using the hand crank on the right. The clothes were then wrung out using the mangles above, and the process was repeated sans soap to rinse them. They were then hung in a drying room adjacent to the funnel uptakes, ready for the engineers’ next watch in the boiler or engine rooms.
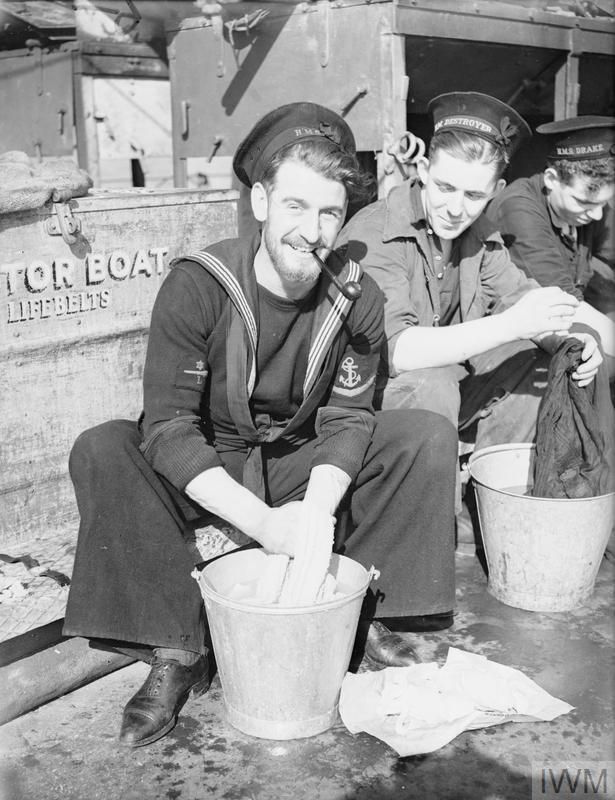
Figure 37. Laundry day, destroyer HMS Vanity, October 1940.129 Notwithstanding Vanity’s age (having been commissioned in 1918), this scene would not have looked out of place in Warrior 80 years earlier.
This period also saw the development of tinned food in the 1810s (Figures 38 and 39), followed by refrigeration (again made possible by steam power), which was first applied at sea in purpose-built ‘reefer’ merchant ships during the 1870s. 130,131 Although these developments did not completely preclude the use of lime juice or prevent other vitamin deficiencies, they substantially improved shipboard food preservation, nutrition and dietary variety.

Figure 38 (left). Replica tin of soup, as supplied to the 1845 Franklin Arctic expedition.132Although its loss with all hands has been at least partly ascribed to the lead used to seal these tins or to food poisoning from insufficient sterilisation, more recent research (based on morbidity and mortality data from other RN Arctic expeditions during the same period from 1848 to 1854), suggests this is less likely.133

Figure 39 (right). Leopold McClintock found this tinned meat while searching for Franklin in 1857–59.134 Opened in 1926, this is the world’s oldest (putatively) edible piece of meat.
While RN personnel were entitled to an alcohol ration since its inception, it was only from 1740 that this became standardised on one gill (142 ml) of up to 97 proof (55.4% abv) rum, diluted 1:3 with water to make ‘grog’, issued twice daily at 1000–1200 (Figure 40) and 1600–1800. The ensuing high rates of alcohol-related morbidity and disciplinary problems led to the ration being halved in 1825, followed by the afternoon issue being abolished in 1850. While the RAN never had the ‘tot’ (in place of beer), the RN kept it until 1970, the RCN until 1972 and the RNZN until 1990.135
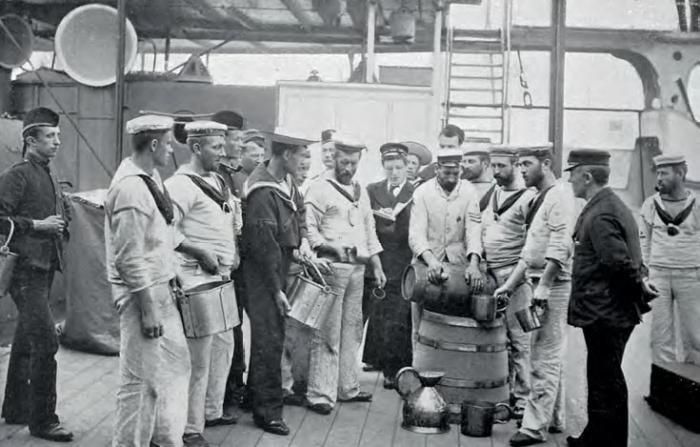
Figure 40. Rum issue, HMS Royal Sovereign, 1896.136 The neat rum was poured from the small cask into the large tub and diluted with water, thereby spoiling it if not consumed immediately . It was then carefully measured into the metal ‘fannies’ carried by each mess representative, who divided it among their messmates (typically eight men). Despite a high level of accounting and supervision (note the officer on the right), the at times highly creative circumvention and/or illicit use of the ‘tot’ for bartering purposes led to abuse.
Naval medical administration
A yet-to-be-published article explained how the 17th-century Anglo-Dutch wars led to a series of wartime Sick and Hurt Commissions to fund treatment services ashore, the last of which became a permanent Board in 1714 (80 years before its Army counterpart).137 Having done surprisingly little to advance the naval medical art, its functions were transferred to the Transport Board in 1806, which was in turn folded into the Victualling Board in 1817.138,139 This left the RN without a dedicated medical authority ashore until the Admiralty underwent a major reorganisation in 1832. This included a bespoke Medical Department, which had responsibility for the RN’s seagoing medical services and ashore for the first time, 64 years before the Royal Army Medical Corps likewise had regarding the British Army’s field and base health services.140 The first Physician of the Navy was Sir William Burnett (Figure 41), who introduced libraries and museums at Haslar and Plymouth (Figure 42), implemented more humane treatment for ‘lunatics’, and instigated the parliamentary Health of the Navy statistical reports from 1830–36, 1837–43 and annually from 1856 into the late 1960s.141

Figure 41. Sir William Burnett (1771–1861) c.1841.142 He joined the RN in 1795 and served at sea in the battles of St Vincent, the Nile and Trafalgar before becoming Physician to the Mediterranean Fleet in 1810. Following a period in private practice, he returned to the RN in 1822 as the Medical Commissioner to the Victualling Board, from which he became the first Physician of the Navy (Medical Director-General from 1843) from 1832 to 1855.143
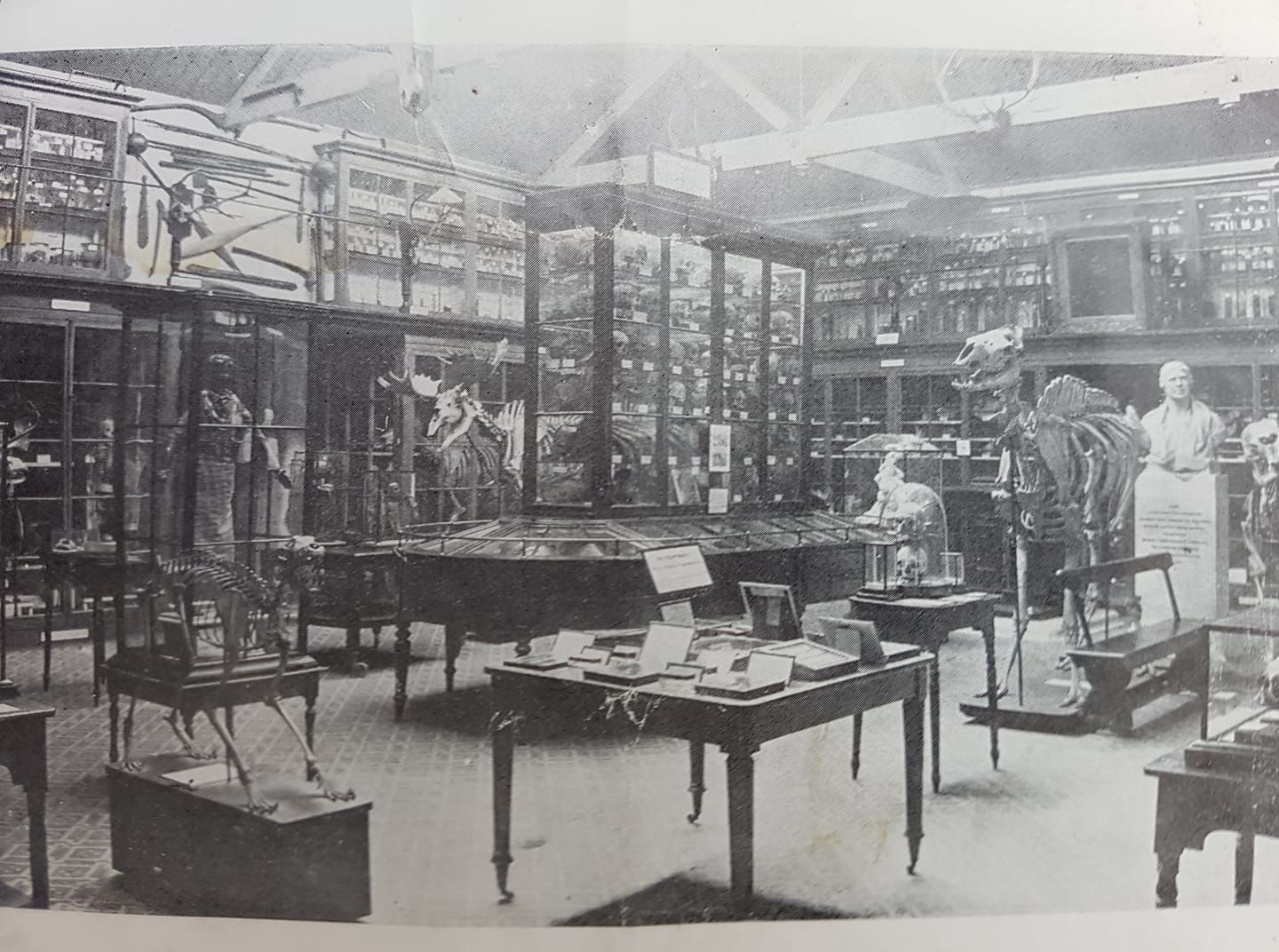
Figure 42. RN Hospital Haslar Museum, undated.144 Established in 1837 for teaching purposes, the collection was mostly destroyed by German bombing in October 1941.
However, Burnett was less successful regarding surgeon recruiting and retention. Besides considerably lower pay than their Army counterparts, new entrants joined the RN as warrant rather than commissioned Assistant Surgeons until 1843; even then, they continued to be accommodated afloat with the midshipmen and other warrant officers until 1855. Having waited up to 20 years for promotion to surgeon (which gave them commissioned status with wardroom privileges and a cabin (if available) from 1805), they were still ranked behind every executive branch officer with minimal opportunities for further advancement. Furthermore, the absence of aged-based retirement throughout the RN meant that in 1840, 63% of all RN surgeons were on half-pay (and hence putatively liable for sea) despite being appointed as far back as 1778.145
As a result, Burnett had only 201 surgeons for 328 billets in 227 ships at the outbreak of the Crimean War. The generally less-than-successful expedients that followed resulted in a committee chaired by Vice Admiral Sir Alexander Milne RN in 1866 (Figure 43), which led to surgeons receiving equivalent ranks to executive branch officers (although their titles continued to evolve over the next half-century), and improved pay parity with their Army peers. Even so, recruiting remained problematic (seven candidates for 64 vacancies in 1881) until an 1883 committee chaired by Rear Admiral Sir Anthony Hoskins RN (Figures 44 and 45) fully aligned RN surgeon’s pay with Army’s and established a separate medical school at Haslar in lieu of sharing the Army’s at Netley.146,147

Figure 43. Admiral Sir Anthony Milne GBC KBC RN (1808-1896), 1879.148 Milne entered the RN in 1817 and served on fisheries protection and anti-slavery duties on the North American and West Indies Stations. He moved to the Admiralty in 1847, where his responsibility for transport shipping during the Crimean War gave him a comprehensive understanding of the RN’s personnel difficulties. He returned to the North America Station as Commander-in-Chief in 1860 amid diplomatic complications from the American Civil War. Milne first became First Naval Lord in 1866-68 and returned to sea as Commander-in-Chief Mediterranean Fleet from 1869 to 1872, followed by another tenure as First Naval Lord until he retired in 1876.149

Figure 44. Rear Admiral Sir Anthony Hiley Hoskins (1828–1901), 1883.150 Hoskins entered the RN in 1842 and had extensive service, including anti-slavery patrols off West Africa, the Crimean War, the 1860 China War and the 1882 Egyptian campaign. He also served on the North American Station and was appointed Commander Australia Station from 1875 to 1878 after his predecessor, Commodore Sir James Goodenough, died from tetanus after being shot by an arrow in the Santa Cruz Islands. While at the Admiralty in 1880–82, he chaired several personnel inquiries, two of which formed the basis of the RN (hence RAN) medical officer and sick berth attendant career structures over the next century. Hoskins later served at the Admiralty as Superintendent of Naval Reserves and as Commander-in-Chief Mediterranean Fleet in 1889–91, followed by First Naval Lord at the Admiralty, before retiring in 1893.151

Figure 45. Medical officers, RN Hospital Haslar, 1890.152
Although the sick and injured at sea had been nursed for centuries by their messmates or whoever else was available (including women), by 1800, most ship’s captains were allocating bespoke personnel by 1800. Even so, these typically comprised sailors or marines who were either inclined to care for the sick or injured or deemed useless for anything else. In 1833, the Admiralty formalised these arrangements, adding that these ‘sick berth attendants’ had to be over 18 years old, physically fit and literate with a good understanding of accounts. This reflected their duties, which (besides omnipresent cleaning), included dispensing, preparing sick diets and assisting with sick mess, medical stores and surgical instrument accounting. However, they had no clinical training apart from whatever their surgeon(s) chose to provide; furthermore, the absence of continuous service meant that their sick berth attendant roles only lasted for their ship’s commission (typically three years), with no guarantee of naval employment on coming ashore or even having the same job in their next ship. Meanwhile, the naval hospitals continued to employ untrained women for nursing duties, assisted by casual civilian male pensioners or labourers.153
While the introduction of continuous service in 1853 gave ‘sickbaymen’ the same long-term careers as other sailors, they were still not necessarily employed on medical duties when ashore, while those who typically only undertook ‘scrubber’ or ‘labourer’s duties’ rather than gaining clinical experience. It was not until 1883 that another committee chaired by Hoskins instituted a formal career structure (based, perhaps rather tellingly, on the steward’s branch) for alternating periods of service ashore as well as afloat. Their training entailed 17-year-olds undergoing 18 months of training at Haslar, with their further advancement depending on their satisfactory reporting and examination performance (Figure 46). In 1900, selected ‘Chief Sick Berth Stewards’ became eligible to become ‘Head Wardwasters’ (initially one each at Haslar, Plymouth and Chatham), which led to the current RAN Maritime Health Support Officer branch.154,155

Figure 46. Sick berth attendants (possibly a class with their instructors), RN Hospital Haslar, c.1910s.156
Having also eliminated male pensioners/labourers ashore in place of sickbaymen, the Hoskins Committee also introduced a female-trained women’s nursing naval service based on an Army counterpart established in 1881 (Figure 47).157 This reflected three requirements: the need for better nursing care commensurate with the advances in medical and surgical practice, using nurses to train the sickbaymen, and providing naval continuity should additional female nurses be required to backfill the sickbaymen drawn to sea during wartime. Having begun with 15 members at Haslar and Plymouth in 1884, the RN Nursing Service was renamed the Queen Alexandra’s Royal Naval Nursing Service (QARNNS) in 1902. However, they were not liable for overseas service until 1890, did not serve aboard RN hospital ships until 1898, and were not subject to RN discipline until 1977.158,159

Figure 47. RN Nursing Service personnel, c.1885.160 The Red Cross on the right arm was replaced by the QARNNS rank insignia on the right side of the cape after 1902.161
Conclusion
This series of articles has explained the connections between warfare, ships and medicine, from prehistory through the Egyptian and Greek, Roman, Viking and medieval periods, and then English (later British) Tudor, Stuart, Georgian and Victorian history. The key common feature relates to maritime trade; the easier and far more cost-effective transport of goods by water compared to land created opportunities to seize them by force, and hence the need to protect them. As humanity advanced from hunter-gatherer tribes to the first settlements, villages, towns, cities and eventually nation-states, these considerations led to escalating competition for the waterborne trade routes on rivers, lakes, estuaries, bays and eventually regional seas, which the Portuguese, Spanish, Dutch, French and English extended to the world’s oceans from the 15th century. Over the next 300 years, the last two powers became dominant, with Britain gaining supremacy from 1815. This entailed Britain using its geographic location and overseas bases to control its rivals’ trade routes and establish a positive feedback loop whereby its naval power extended the economic power that funded it.
Initially, the role of Western medicine in supporting these developments had a minor role for three reasons. It was only after Europe began to extend its maritime reach into the world’s oceans that its ships spent enough time at sea to cause bespoke medical conditions, an effective response to which was impeded by the 1300-year-old dead hand of Galen for another 300 years. The only exception pertained to ships being recognised as disease vectors, for which the bubonic plague or ‘Black Death’ (1346–53) led to the introduction of quarantine, albeit only to protect those ashore rather than afloat.162
Secondly, their separate origins in the 12th century led to a split medical profession between physicians and surgeons, which endured in Britain for over 600 years. The physicians’ university training in humoural medicine gave them considerable influence but often limited and even adverse clinical effectiveness, while the surgeons’ apprentice-based training produced practical, if at times variable, skills in a subordinate capacity. Hence, although the first English ‘sea-surgeons’ went to sea after 1512, they could legally only treat injuries and battle casualties, yet were confronted with at times overwhelming numbers of medical cases while the physicians pontificated from ashore.
Thirdly, the absence of differentiation between warships and merchantmen extended to their crews, whose need to defend the latter meant they were essentially interchangeable. Furthermore, as the RN only operated in European waters during the summer months well into the 17th century, the East India Company became the centre of English maritime medicine, which, unlike the RN, was properly funded. Although these considerations created fewer crewing problems for the RN during peacetime, the influx of warships entering service at the beginning and during a conflict, requiring far more seamen than most merchantmen to crew their guns, led to increasingly intense competition for the same scarce trained workforce. Furthermore, gross overcrowding in the warships created high rates of infectious disease, such as typhus, while poorly-preserved victualling and doubtful water supplies led to dysentery. As the RN’s ships began operating in the tropics, their crews were also exposed to conditions such as malaria and yellow fever. Meanwhile, as they spent more time at sea, lack of fresh food resulted in vitamin deficiencies such as scurvy.
By the 1740s, the impact of the ensuing losses of scarce trained seamen on the RN’s operations had finally become apparent, over a century before the Crimean War led the British Army to a similar conclusion. Even so, it took 50 years for both services to implement the relevant preventive measures. For the RN, this entailed formally implementing the hygiene measures that had been readily apparent for decades, initially via patronage given the lack of other means. For the physicians, this began with James Lind, his disciples Gibert Blane, Thomas Trotter and William Burnett, and thence their respective acolytes. Even so, their efforts regarding what measures had to be done would have been for nothing were it not for the executive officers with the authority to direct how to implement them. This began with George Anson and his protégés Byron, Howe and Keppel (and their successors such as Cornwallis, Jervis, Collingwood and Nelson), along with James Cook and his followers, including Vancouver and Bligh (and their followers such as Flinders, Franklin, Fitzroy, King and Stanley). Although the hard-won lessons learned were passed on first-, second- and third-hand via this means into the 1850s, subsequent developments reflected the demise of humoural medicine in lieu of the scientific medical advances that followed and an effective naval health administrative system afloat and ashore to promulgate them.
To this end, one of the key features throughout the later period covered by this series relates to the absence of a single agency for the RN’s seagoing and shore-based health services. This partly reflected the interchangeable nature of the English seaman’s employment between civilian shipowners and the monarch, for which Eleanor of Aquitaine introduced the Laws of Oléron in 1189. Although this made all ships’ masters liable for the lodging and treatment of their ill and injured crew members, meeting this obligation was perennially impaired by a lack of accommodation. This mainly occurred when that which was available was swamped by non-battle casualties, as occurred after the 1588 Spanish Armada and during Charles I’s 1626–29 war with Spain. It was not until the First Anglo-Dutch War (1652–54) that overwhelming battle casualties resulted in this responsibility being assumed by a succession of wartime Sick and Hurt Commissions, with the last becoming a permanent peacetime Board in 1714.
Although these Commissions had introduced the first rudimentary naval medical administrative processes for managing patients ashore, neither they nor the peacetime Board that followed did much more than manage contractors. Escalating costs, poor quality care, and the failure to effectively manage convalescent cases ashore led to the RN’s purpose-built hospitals at its battlefleet bases from the 1750s and eventually elsewhere. Following the Sick and Hurt Board’s demise in 1806, it was not until 1832 that the RN had a bespoke department that centralised its medical administration ashore and afloat for the first time. This provided the means to advance the naval medical art that supported the RN’s worldwide peacetime and warlike operations into and beyond WWII.
The views expressed in this article are the author’s and do not necessarily reflect those of the RAN or any other organisations mentioned.
Corresponding Author: Neil Westphalen, neil.westphalen@bigpond.com
Authors: N Westphalen1,2
Author Affiliations:
1 Royal Australian Navy – Directorate of Navy Health
2 University of New South Wales Canberra at ADFA






