Introduction
Previous articles in this series describe the development of a cycle from prehistory to the end of the Elizabethan period, whereby increasing trade necessitated larger and more efficient ships to transport merchandise and better weapons to defend or attack them, thereby facilitating further trading opportunities. 1,2,3,4,5,6 However, it was not until the 18th century that Western medicine had developed sufficiently for its role as an enabler of this cycle to be recognised, thereby making possible—among other things—the European settlement of Australia6.
While the technical developments in ships, weapons and medicine often developed independently in multiple regions worldwide, they remained closely linked throughout Western history. This article continues this series by describing the developments in naval warfare, ships and medicine during the British Georgian period from 1714 to 1815. An article filling the gap in this series regarding the Stuart period (1603-1714) has been submitted for publishing in due course.
Georgian naval warfare
By 1714, England (Great Britain following its union with Scotland in 1707) had been at war with France more-or-less continuously for 25 years. These and the long and costly conflicts that followed were largely funded by Britain’s transoceanic maritime trade, which had begun with the establishment of the East India Company in 1600, followed by the acquisition of colonies in North America from 1607 and the Caribbean from 1655. English victories at sea during the 1690s limited French access to its own colonies from the Atlantic, while the capture of Gibraltar in 1704 did likewise from the Mediterranean. This meant Britain could further expand its trade, thereby funding its wartime armies and those of its European allies while simultaneously bankrupting their opponents. Despite losing its American colonies in 1783, Britain used this strategy to maintain its economic and maritime supremacy from 1815 until the early 1900s.7 However, this would not have been possible without finally controlling the occasionally universal rates of what would now be referred to as Disease and Non-Battle Injuries (DNBI) that had been experienced by the English and their Portuguese, Spanish, Dutch and French competitors since the mid-to-late 15th century.
Georgian naval warfare, therefore, usually entailed defending one’s own or attacking enemy merchant shipping, typically in single-ship actions that usually produced few wounded (what would now be termed Battle Casualties or BCas) among their crews. Meanwhile, the excessive formalisation of ‘line-of-battle’ tactics for major fleet actions after 1714 produced plenty of BCas but otherwise proved indecisive: it was not until the 1780s that it was realised that the key to victory lay in breaking their opponent’s battle line, which produced truly overwhelming BCas. This culminated at the Battle of Trafalgar in 1805, when the French and Spanish sustained over 5000 dead, 2700 wounded and at least 7000 taken prisoner from 26 000 men (56 per cent), while the British lost 458 killed and 1208 wounded from 17 000 men (10 per cent).8
Meanwhile, the peacetime demand to expand British trade while making it safer and more efficient led to various ostensibly non-medical scientific advances. The most important of these pertained to developing a means of ascertaining longitude, which began after a navigation error wrecked four out of five British warships on the Scilly Isles in 1707 (killing up to 2000 men), but did not achieve fruition until the first chronometers began to prove their worth during the 1770s.9
These demands also begat Britain’s scientific expeditions to the Pacific and elsewhere, beginning with HMS Dolphin’s circumnavigation in 1764–66. Her captain, John Byron, had narrowly survived the wreck of HMS Wager during Commodore George Anson’s 1740–44 circumnavigation, while his crew included master’s mate John Gore, who sailed with Captain Samuel Wallis on Dolphin’s next circumnavigation in 1766–68, and Captain James Cook on his first and third voyages in 1768-71 and 1776-80. In so doing, Byron and Gore provided continuity between the navigational shortfalls that had contributed to Anson’s medical disasters (see below), and Cook becoming the father of British hydrography: the latter’s subordinates William Bligh and George Vancouver were followed by their protégés and successors into the 1850s, including (among others) Matthew Flinders, John Franklin, Robert Fitzroy, Philip Parker King and Owen Stanley.10 Noting that their charts often remained in use beyond World War II, their achievements were only made possible once their surgeons could facilitate keeping some very small ships at sea in typically very remote areas, in addition to simply providing treatment services when people became ill or were injured. At the same time, the links between superiors and their protégés into the second and subsequent generations demonstrate the extent to which the 18th century Navy depended on the patronage system.11
Georgian Ships
The previous article in this series on the Tudor period described how the development of ‘line-of-battle’ tactics in the mid-17th century led to warships differentiating into those with two or more gun decks that could take their place therein (hence ‘ships-of-the-line’), and those with one gun deck known as ‘frigates’, which were fast enough to act as fleet scouts, and large enough to attack enemy and defend their own merchant shipping independently.12,13 In 1677, The Secretary of the Admiralty, Samuel Pepys, had further classified the RN’s warships into six ‘rates’ based on the number of guns they carried. Although the smallest deemed suitable for the ‘line-of-battle’ at that time were 40- to 50-gun ‘fourth rates’, by 1714 this had increased to 50 to 60 guns, thence to 60 to 70-gun ‘third rates’ by the 1750s, and then 70 to 80 guns during the Napoleonic Wars.14 During the same period, gun sizes likewise increased: for example, frigates typically carried nine-pounder guns in 1714, but 18- or even 24-pounders a century later. These increases in gun numbers and size necessitated larger crews, from around 300 men for 50-gun ships in the 1710s, to 550 men for 74-gun ships from the 1780s.15 Furthermore, as the Navy’s ships became larger, their wartime numbers also increased, from around 250 in 1714 to over 900 in 1815.16 These factors posed progressively greater challenges for the navy – including its medical services – in sustaining enough men to keep all these ships at sea during wartime (Figure 1).
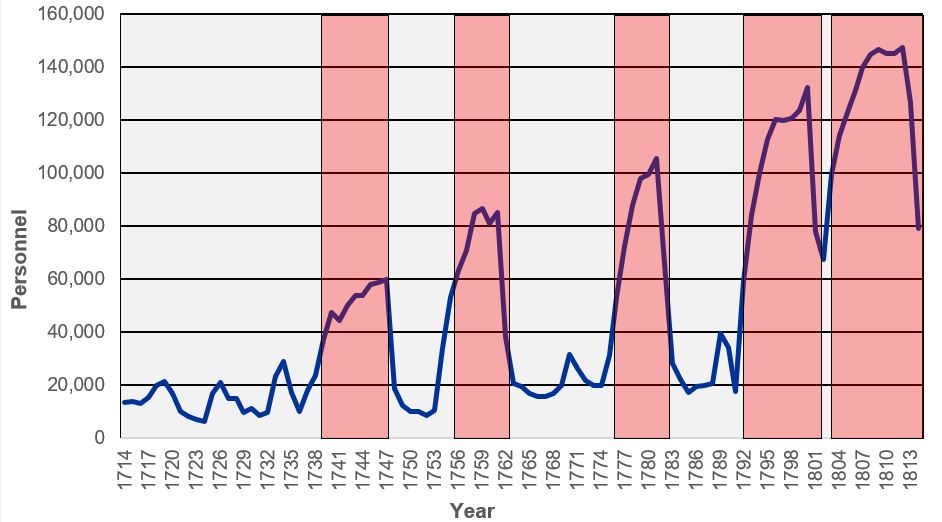
Figure 1: Royal Navy personnel, 1714-1815.17 The red bars indicate active wartime periods (but also note the peaks between, indicating minor conflicts and/or war scares).
It should also be noted that each ‘rate’ increased in size while maintaining their gun numbers, to improve overall seakeeping and better facilitate fighting their lower deck guns in bad weather.18 This also allowed them to remain at sea longer, which for the first time made it possible to blockade the French Atlantic ports more-or-less all year round from the 1750s. These advances increased the DNBI threat to their crews, in particular dysentery from the limitations inherent to their food and water preservation, typhus from their clothing and bedding, and scurvy from a lack of dietary Vitamin C. Furthermore, ships on foreign stations faced additional threats from vector-borne disease, in particular those in the East and West Indies.
Meanwhile, merchantmen likewise increased in size while keeping their crew sizes small to minimise expenses, with most still carrying small-calibre guns on their weather decks for self-defence. The only exceptions were the East India Company’s ‘Indiamen’ – big ships with warship-like gunports and large crews, but lightly-built and only armed with small-calibre guns.19,20Although they were not naval vessels, these ships remained crucial to British maritime power into the 19th century. Their size and armament allowed them defend themselves while extending their trade with India and China, if necessary by force. Furthermore, like the highly profitable triangular transatlantic trade to Africa and the West Indies (including the notorious ‘middle passage’ slave component until its abolition in 1807), the taxes on their cargoes paid for the navy that protected them from commerce raiders. In addition, their large crew sizes increased the pool of trained seamen during peacetime, who could be employed interchangeably – if not voluntarily – with the Navy in wartime. Even so, these crews and their passengers still faced the same DNBI threats as the Navy from their food and water, and from vector-borne disease during their port visits en route to and from India.
Georgian naval medicine
Naval medical administration
The future article in this series on the Stuart period will describe how the Laws (also Rules or Rolls) of Oléron, introduced in 1190, became overwhelmed by the number of naval BCas and DNBI during the First Dutch War (1652–54). This led to the first of five Commissions for Sick and Hurt from 1653, which were responsible for wartime medical services ashore and prisoners of war over the next 50 years. In 1714, the last Commission became a permanent Sick and Hurt Board, 80 years before its British Army counterpart was established in 1793.21 Even so, its primary role pertained less to advancing the naval medical art than managing the Navy’s medical finances: for example, although naval surgeons were first required to submit medical journals (including the details of each case) from 1704, this was only done to facilitate their per capita remuneration component rather than to collate and disseminate any lessons learned.22,23 Having proved ineffective even to this end, the Sick and Hurt Board’s prisoner-of-war functions were transferred to the Transport Board in 1796, followed by its remaining responsibilities 10 years later.24 This left the Navy without a dedicated medical department until the Admiralty underwent major reform in 1832.25
Hosier and Anson
Before explaining the 18th-century advances in naval medicine, it is necessary to describe the seminal events that instigated them, the first being Admiral Francis Hosier’s West Indies operations during a limited war with the Spanish in 1726–29.
Hosier’s mission entailed using 20 ships to blockade Spanish treasure ships in Portobello in modern Panama. In response, the Spanish landed their treasure and waited six months for the scurvy acquired by Hosier’s force while crossing the Atlantic, and the local vector-borne diseases on his arrival, to force his withdrawal. This having eventuated, Hosier replaced his losses in Jamaica, after which he continued to lose men in large numbers over the next six months while blockading Vera Cruz and Havana. By the time he and both his successors had died of yellow fever, up to 4000 men had succumbed without a shot fired, from a force that never exceeded 4600 at any one time.24,26 This disaster was immortalised by a ballad celebrating Admiral Edward Vernon’s victory at Portobello in 1739, with only six ships and 2300 men, at a cost of only three killed and seven wounded.27,28
Mention has already been made of Anson’s circumnavigation (Figure 2). Having received his orders in November 1739, manning shortfalls before his departure 10 months later were acute, accompanied by 20 or 30 sick at a time being crammed into private houses in Portsmouth ‘two or three in a Bed of different diseases, without proper Nurses or people to look after them’. Even so, Anson’s situation was not unusual until he received 500 ‘invalids’ to serve as marines. As they were usually only deemed suitable for garrison or reserve duties ashore, these men averaged 55 years of age, and had disabilities ranging from limb and back injuries to blindness, deafness and epilepsy. Only 259 joined their ships (none surviving the voyage) after those fit enough to desert did so.29 Anson then received 300 men to replace the deserters, whose lack of training led to their mortality being almost as high as the invalids.30,31

Figure 2. Admiral George Anson, c.1747.32
Having departed Portsmouth in September 1740 with eight ships and 1967 men, Anson’s passage to Cape Horn set the medical scene, with plagues of flies from rotting provisions resulting in dysentery outbreaks. In South America, the setting up of hospital tents for these cases in a mosquito-infested area led to malaria, while storms off Cape Horn led to dozens of injuries and exhaustion (Figure 3). The inability to wash left men swarming in lice, resulting in typhus, while freezing conditions led to frostbite. Even so, these proved mere harbingers to one of the worst scurvy outbreaks ever recorded, with 751 deaths in three months.33 As the weather had scattered his squadron, Anson proceeded to Juan Fernandez Island, whose misplacement on the chart in this pre-chronometer era cost 70 lives in nine days while he searched the wrong area (Figures 4 and 5).30
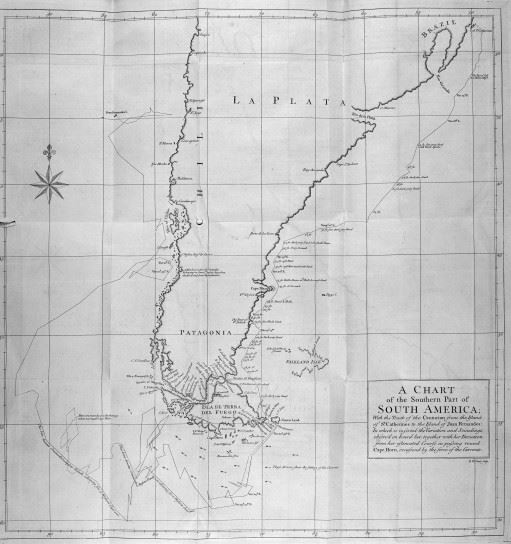
Figure 3. Anson’s track chart around Cape Horn, 7 March to 10 April 1741.34 Note the two tracks resulting from his inability to calculate longitude: one of his estimated route and the other of his actual route, with the former ultimately 300 nautical miles west of the latter. This chart demonstrates how the otherwise avoidable prolongation of sea time exacerbated the scurvy threat to Anson’s personnel.
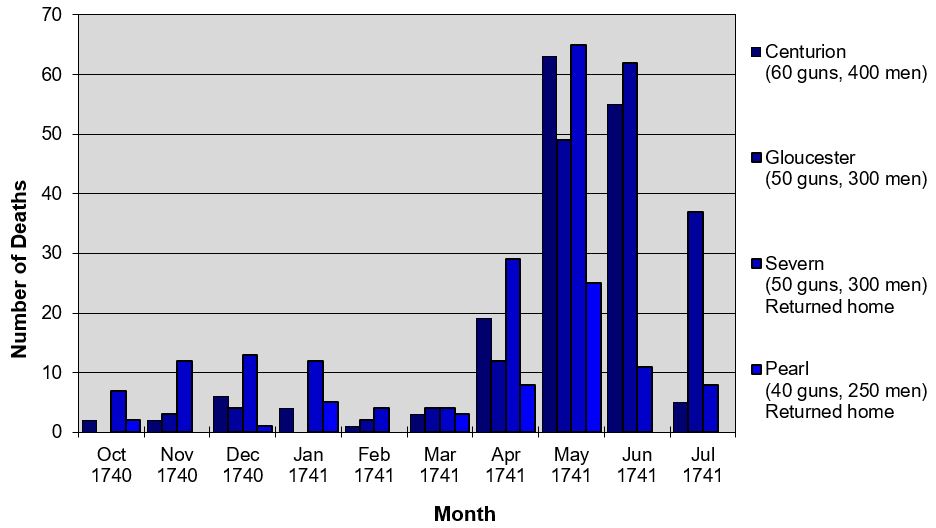
Figure 4. Total crew mortality, Anson circumnavigation, October 1740 to July 1741.35 This timeframe covers the period between the squadron leaving Britain and Gloucester’s arrival (six weeks after Centurion) at Juan Fernandez. Mortality figures for the other four ships during this time (Wager, Tryal and the storeships Anna and Industry) are unavailable.
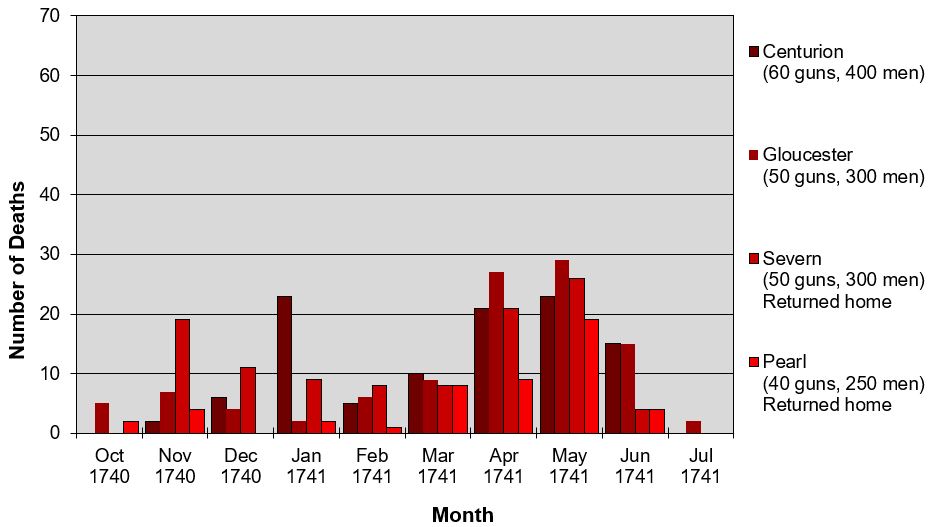
Figure 5. Invalid and marine mortality, Anson circumnavigation, October 1740 to July 1741.36 This timeframe covers the period between the squadron leaving Britain and Gloucester’s arrival (six weeks after Centurion) at Juan Fernandez. Mortality figures for the other four ships during this time (Wager, Tryal and the storeships Anna and Industry) are unavailable.
By September 1741, Anson was only left with Centurion, Gloucester and 335 men, the rest having either been shipwrecked, returned home or died. Having recovered with fresh vegetables, fish and sea lion meat, Anson successfully raided the South American west coast until May 1742, when he proceeded across the Pacific to intercept the Manila treasure galleon off the Philippines. Although this typically took two months at the right time of year, doing so two months late meant it took four. This resulted in more scurvy that forced Gloucester’s scuttling for lack of crew, and by the time Centurion reached Tinian in the modern Marianas, another 99 men had died ‘like rotten sheep’.37 Although fresh greens worked their usual cure, her crew took three months to recover enough to sail for modern Macau, China, to refit. Having made her capture in June 1743 off Samar in the Philippines, Centurion arrived home a year later, up to £400 000 richer but with only 188 survivors. Overall, Anson had lost 1240 men (63 per cent), of whom only four were killed in action.30
Despite the cost in lives, Anson’s mission success led to his becoming Admiralty First Lord from 1751 to 1756. Nevertheless, his tenure oversaw substantive reforms, including improved victualling quality; clean clothing for new entrants (although uniforms for the sailors were not provided for another century), and the modern divisional system, which, among other benefits, made individual officers specifically responsible for their division’s hygiene (rather like antimalarial chemoprophylaxis 150 years later).38,39,40 Perhaps more importantly, Anson’s patronage as First Lord led to many of his surviving officers achieving high rank, such as George Saunders, who became First Lord (albeit briefly) in 1766 and was followed by Augustus Keppel (1766 and 1782–83), Peircy Brett (1766–70) and Richard Howe (1783–88), the latter also winning the Battle of the Glorious First of June in 1794. Although the hard lessons they had learned first-hand were passed on to their protégés such as William Cornwallis, John Jervis, Cuthbert Collingwood and Horatio Nelson, it was only when these achieved high rank themselves from the mid-1790s that they were applied Navy-wide.
Anson’s circumnavigation, therefore, had profound effects on the Navy well beyond his death in 1762. As such, although far less well-known, its effects on the RN medical services can be considered analogous to how the better-known medical disasters during the Crimean War (1853–56) likewise affected the British Army medical services a century later—especially considering how in both cases, the ensuing reforms took around 50 years to be fully implemented.41
Subsequent medical advances
Notwithstanding the more egregious failures that followed Hosier and Anson into the 1790s (such as the Second and Third Fleets to Australia), most seamen had accepted the need for better shipboard hygiene by 1714. Some improvements were being made in the victualling to reduce food poisoning; therapeutics had somewhat improved, and—despite the ongoing split in the British medical profession between university-educated physicians and apprentice-trained surgeons—it was generally accepted that naval surgeons needed the skills to treat non-surgical conditions. However, acquiring these skills continued to be hampered by the humoral theory of disease, which remained extant in the face of mounting evidence otherwise into the 1840s..
In this regard, William Cockburn (1669–1739, Figure 6) became the last Navy physician whose medical advice was solely based on convincing yet fallacious theories that had not yet been discounted. To this end, he wrote several books, many in multiple editions; examples include The Nature and Cure of Distempers of Seafaring People, with Observations on the Diet of Seamen in H.M.’s Navy (1696) and Symptoms, Nature, and Cure of a Gonorrhoea (1713). Despite spending just two years at sea only in home waters, he provided the simplistic, inexpensive and therefore welcome advice that lazy sailors were more susceptible to scurvy and other maladies while advocating his own patient remedy for dysentery that the Navy used into the 1730s. Although ‘Jesuit’s bark’ (containing quinine and quinidine) was in general use for intermittent fevers, Cockburn continued to apply his own humoral theories by bleeding not only all his fever cases, but also those with respiratory, intestinal and cerebral conditions.42 Hence, notwithstanding his conscientious attention to the sick, Cockburn’s advice generally proved detrimental to Hosier’s, Anson’s and other’s crews into the 1750s.

Figure 6. Dr William Cockburn, 1697.43
Following Anson’s return, Surgeon James Lind (1716–94, Figure 7) performed the first known therapeutic controlled trial, in May 1747 aboard HMS Salisbury in the Bay of Biscay.44 He gave 12 scurvy cases the same diet, with two of each also receiving daily either a quart of cider, 25 drops of elixir of vitriol (dilute sulphuric acid), two spoonfuls of vinegar, 280 ml of salt water, a mixture of garlic, mustard and herbs or two oranges and a lemon. Of these, one of the last two returned to duty after six days while the other was almost ready to do when the fruit ran out.24 Even so, Lind’s 1753 Treatise of the Scurvy (dedicated to Anson) referred to citrus fruit as only one among other therapies and erred in recommending the juice be boiled into a concentrate or ‘rob’, which destroyed the vitamin C.45 In 1757 he wrote An Essay on the Most Effectual Means of Preserving the Health of Seaman in the Royal Navy, which referred to watercress (another useful if impracticable vitamin C source) as an antiscorbutic.46 On becoming physician to the Haslar Royal Naval Hospital the following year, Lind invented a still to produce fresh water from seawater, and demonstrated that typhus could be prevented by bathing patients and giving them clean clothing on arrival.24 In so doing, Lind founded his own naval medical dynasty, beginning with Gilbert Blane (1749–1834, Figure 8), Thomas Trotter (1760–1832) and William Burnett (1779–1861), the latter becoming the first Physician of the Navy in 1832 (Director-General of the Navy Medical Department from 1843).

Figure 7. Dr James Lind, c.1783.47

Figure 8. Sir Gilbert Blane, 1833.48
Much of the delay in implementing Lind’s findings was caused by his being only one of many voices to the Admiralty in its search for an effective, practical—and in particular, cheap—solution. Hence, when Cook sailed on his first voyage in 1768, he took several experimental antiscorbutics with him, including malt, mustard, vinegar, pickled cabbage (sauerkraut) and ‘portable soup’ (a dissolvable cake made from boiled-down beef offal—see Figure 9), but only a small amount of lemon juice. Rather than Lind’s advice, these items reflected that by Dr David McBride in his own treatise on scurvy in 1764, supported by Army physician Sir John Pringle, the anatomist John Hunter, Henry Tom from the Sick and Hurt Board, and Samuel Wallis’s surgeon John Hutchinson. Although none of the items they espoused have much vitamin C, their efficacy was not adequately tested because Cook never stayed at sea for more than 15 weeks at a time.24 On the other hand, his close attention to hygiene meant that Cook sustained very few non-scurvy DNBI fatalities, except for 31 deaths from dysentery during his first voyage on his way home from modern Djakarta.
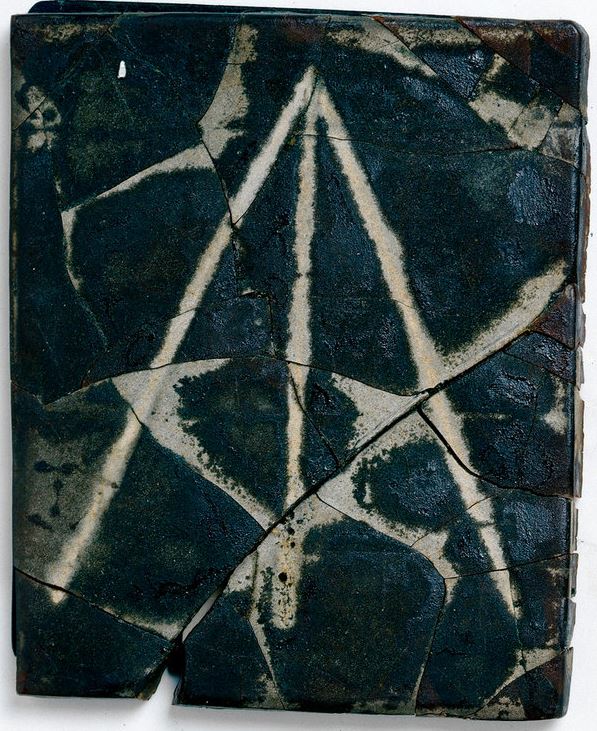
Figure 9. Original ‘portable soup’ slab, made between 1756 and 1779.49 The broad arrow or ‘crow’s foot’ indicates government ownership.
In the event, the final proof came when Blane’s appointment to the Sick and Hurt Board in 1795 coincided with his friendship with Rear Admiral Alan Gardner (a Howe protégé—see Figure 10), who was appointed to command the East Indies Station. Blane advised him to order a large quantity of lemon juice for his flagship Suffolk, which remained on board despite being Gardner’s replacement by Rear Admiral Peter Rainier (a Brett protégé—see Figure 11). Nevertheless, Rainer approved issuing 20 ml of juice to each man daily, mixed with 70 g sugar, 570 ml water and 280 ml rum, with the result that Suffolk remained at sea for 19 weeks without a single scurvy case. This news quickly spread such that by 1804, the Navy was consuming 230 000 litres of juice per annum, despite costing four shillings and five pence per litre.24
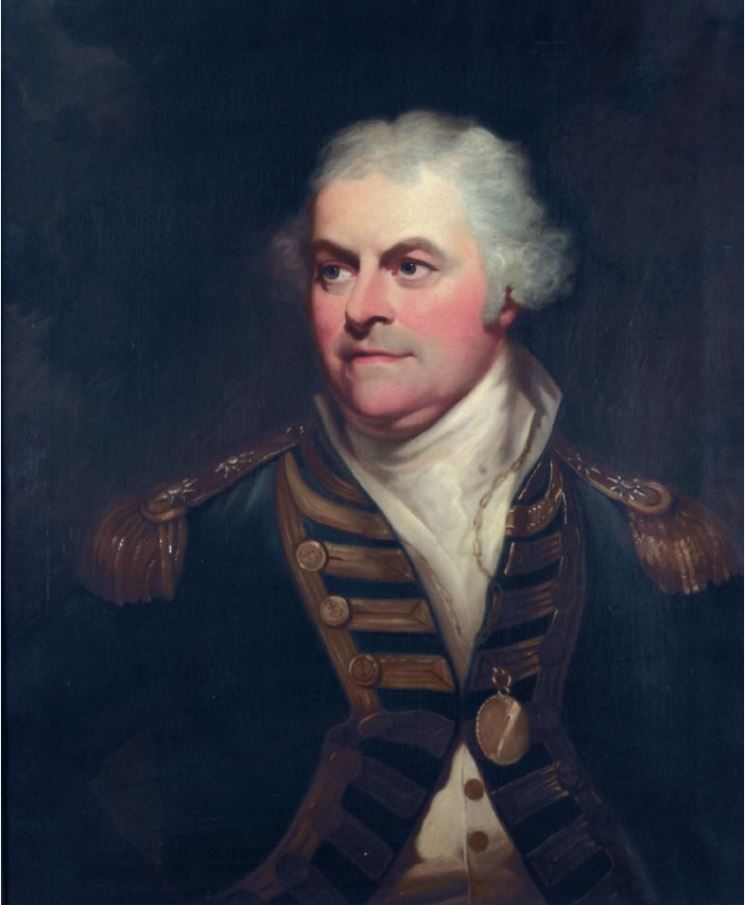
Figure 10. Vice Admiral Lord Alan Gardner (1742–1809), 1780-1809.50

Figure 11. Admiral Peter Rainier, (1741-1808) 1805.51 His glasses have tortoiseshell or horn rims or ‘Martin’s margins’ to reduce the amount of light reaching the eyes.
Meanwhile, Blane also persuaded the Commander of the Mediterranean Fleet, Vice Admiral John Jervis, to order the issue of soap from 1796, which likewise became Navy-wide shortly thereafter.24 Although the quantities proved inadequate until at least 1815, the ability to wash clothes at sea, combined with the issue of free clothing on entry and improved shipboard cleanliness, mostly eliminated typhus—unless it was introduced on board by non-naval embarkees.
Patient care afloat
Cockburn’s writings confirm that during his time, DNBI cases were not collected into a dedicated sickbay and that, as the surgeon and his mates had no attendants of their own (except in hospital ships from 1703—see Figure 12), each patient received their nursing care from their messmates.52 The ensuing lack of isolation would have precluded controlling infectious disease cases, especially given the limited berthing space (Figure 13).
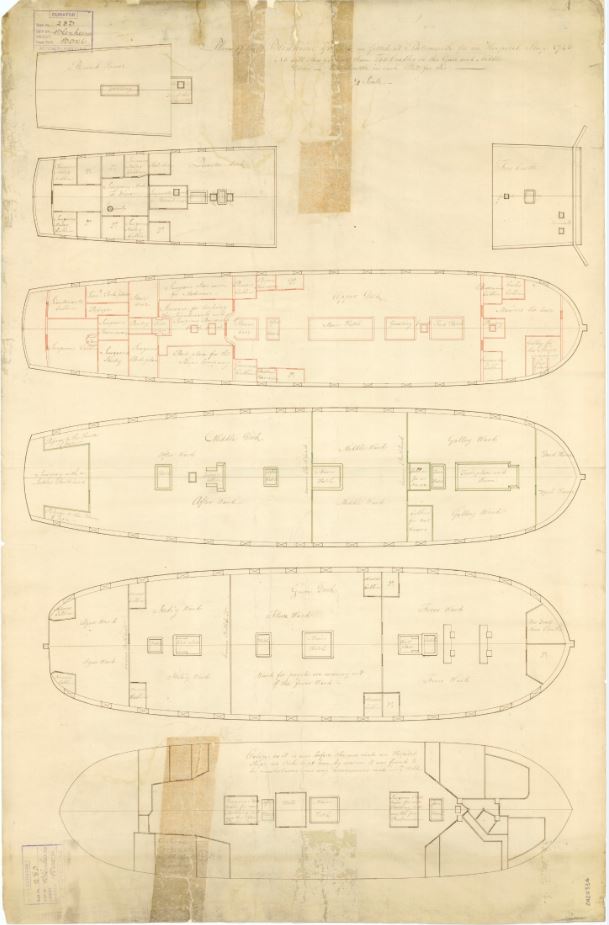
Figure 12. Hospital ship HMS Blenheim, 1743.53 Built in 1679 as the 96-gun three-deck second-rate HMS Duchess, she was rebuilt and renamed in 1709 and served as a hospital ship from 1740 until 1760.54 From top to bottom, note the quarterdeck cabins now used by surgeon’s mates that were previously for the ship’s officers. The upper deck has undergone considerable modifications (in red) to accommodate the senior surgeon, medical stores, the ship’s company and marines. The middle and lower decks form the hospital proper, while the orlop deck has been deemed unsuitable for patients. The middle deck is split into three wards and a mortuary forward; the lower deck forward to aft into ‘ague’ (malaria), ‘itchy’ (scabies) and ‘flux’ (dysentery) to port and convalescent fever cases to starboard, and ‘fever’ wards, with a store room for ‘dead men’s cloathes’ forward. Having previously had a ship’s company of about 570 officers and men, both decks now had cots for 255 patients.24

Figure 13. Berthing plan, lower deck HMS Bedford (74 guns), 1775.55 The blue hammocks are thought to represent seamen (321 men), and the red hammocks marines (96 men). The rest of her crew (totalling about 550 officers and men) either slept on the orlop deck below or had their own messes or cabins on the upper and quarter decks. Note the challenges for the whole ship if infectious DNBI cases (such as tuberculosis, dysentery, typhus and scabies) were not isolated, as had occurred during Anson’s circumnavigation 35 years previously.
However, by mid-century, most ship’s captains were allocating a dedicated space for accommodating DNBI cases, and by 1800, this became a standardised location on the upper gun deck forward, adjacent to the ship’s heads for dysentery cases, and the galley to facilitate special diets (Figures 14–16). Even so, the Admiralty did not mandate dedicated sick berth attendants until 1833, and these had no formal training or a career structure until 1883.24
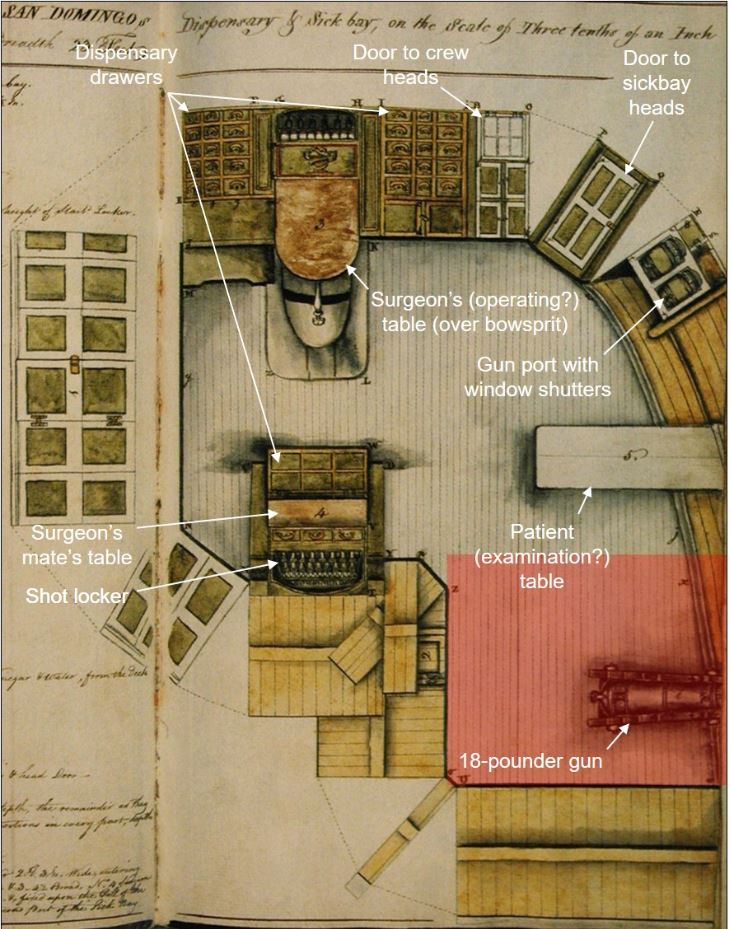
Figure 14. Sickbay plan, HMS San Domingo (74 guns), 1812.56 Sleeping arrangements for patients and staff (noting the latter were accommodated in the same space) are not shown, but at 15 inches (38 cm) per man, the shaded rectangular area aft around the gun would have been sufficient to sling nine cots, making a ward of sorts that left the rest of the sick bay clear for seeing patients. Otherwise, there was space for another seven or eight cots further forward over the patient table and another seven or eight (i.e., a total of 23–25) inboard above the bowsprit.

Figure 15. Sickbay HMS Victory, 2013. Note the cots used for patient bedding, the gun underneath, the poor lighting despite its upper deck location, and the overall lack of space. (Author)

Figure 16. View through the sickbay door to the crew heads, HMS Victory, 2013. The square box in the centre foreground has two of the ship’s six ‘seats of ease’ for over 600 junior sailors and marines. A separate ‘roundhouse’ was provided for about 100 senior sailors and marine non-commissioned officers, another for the sick, while officers had their own heads aft. (Author)
Meanwhile, BCas continued to be treated in the cockpit, on the orlop deck below the waterline, on a ‘first come–first served’ basis, without any first aid or triage. Their wounds comprised blunt and penetrating injuries from club and edged weapons and small arms during boarding actions, and contusions, fractures and amputations from crew-served guns or the splinters they produced (Figures 17-20). To these can be added ‘flash’ burns from ammunition accidents: these comprised up to 25 per cent of BCas in the 1780s until powder spillage was reduced by the introduction of wet rather than dry wads for loading guns, and goose-quill firing tubes and flintlock firing mechanisms.24 Besides the suffering induced by the absence of anaesthetics or analgesia, can be added the threats posed by post-operative infection, tetanus and delayed healing caused by scurvy, the latter leading to Blane recommending early rather than delayed amputation.
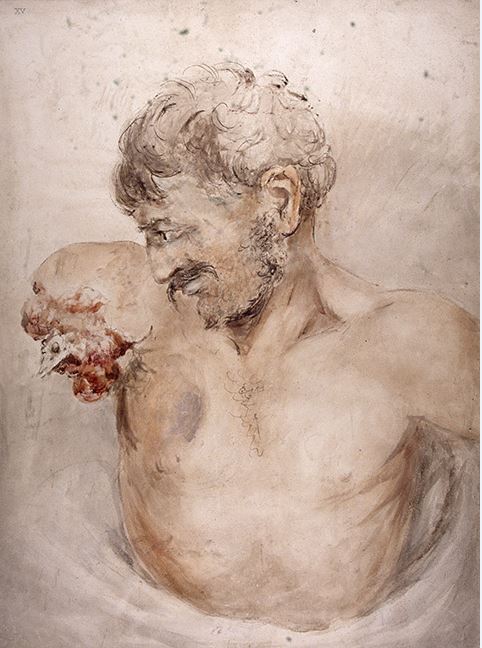
Figure 17. Traumatic amputation, Battle of Waterloo 1815.57 Although naval casualties with the same injuries received broadly similar initial treatment, the often-extended delays before they received definitive care ashore—assuming they survived that long—meant their surgeons had to be far more self-reliant.
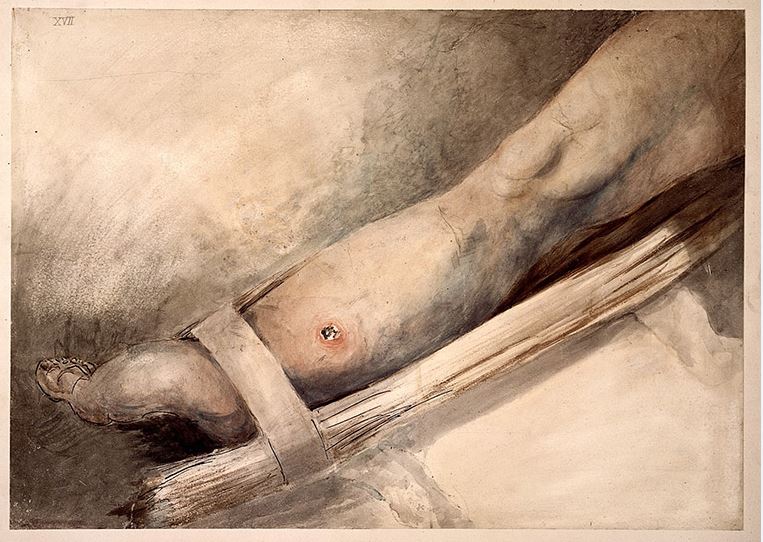
Figure 18. Bullet wound, Battle of Waterloo 1815.57 Wood splinters from naval actions could produce similar penetrating injuries. Neurovascular compromise (whether from trauma or the swelling seen here) and/or the presence of foreign bodies would have necessitated below-knee amputation. Note the relative lack of devitalised tissue produced by a heavy but low-velocity projectile and the extemporised splint.

Figure 19. Penetrating abdominal sabre wound, Battle of Waterloo 1815.57 These and penetrating chest injuries were generally deemed fatal.

Figure 20. Sabre wounds, Battle of Waterloo 1815.57 Similar injuries could be inflicted on naval personnel during boarding actions. Penetrating skull injuries were likewise generally fatal.
Patient care ashore
The future article in this series on the Stuart++- period will explain how the first two Commissions for Sick, Wounded and Prisoners relied on hired lodgings, and that this was fraught with problems regarding treatment, supervision, and regulation: the only thing in its favour was that it was cheaper than the initial outlay on naval hospitals. Even so, these difficulties were such that the subsequent two Commissions came to prefer using civilian hospitals. However, they faced increasing resistance to this solution for two reasons; the first was that Navy patients detracted the hospitals from providing medical services for the poor, anticipating similar concerns from the British (and Australian) public hospital systems 300 years later. Secondly, although cheaper for the Navy than private lodgings, naval patients cost the hospitals more than civilians because their treatment tended to be more complex and they more likely to be long-term or permanently disabled. Hence, in 1691, Queen Mary II donated Greenwich Palace to accommodate elderly and long-term disabled seamen, making more beds available for shorter-term cases elsewhere. Meanwhile, the Chatham Chest continued to provide for other disabled seamen until its merger with the Greenwich scheme in 1814.58,59,60 Although it ceased providing on-site accommodation in 1869, the Greenwich Hospital charity continues to support ex-RN personnel and their dependents to this day.61
Otherwise, insufficient hospital beds meant the last two Commissions and the Sick and Hurt Board that followed continued to rely on private lodgings. This entailed employing contract surgeons/agents to find and pay for suitable accommodation, victualling, and medical and nursing providers. Apart from ample opportunities for peculation, the lack of willing landlords led to overcrowding and poor-quality care (as experienced by Anson’s men), even by the standards of the time. Even so, the most significant problems came from the patients themselves, in particular drunkenness, fighting and desertion among the convalescents. By 1740, increasing sickness rates as the Navy expanded for its next war (Figure 1) meant the contract system could no longer cope.25
The future article in this series on the Stuart period will explain how the first steps had been taken towards naval hospitals for acute DNBI and BCas, with one at Plymouth from 1672 to 1713 (which did not prevent the rest of the town still being overwhelmed by naval patients) and wartime extemporisations at Lisbon and elsewhere. Although lack of lodger accommodation for the Mediterranean Fleet at its Minorca base resulted in the RN’s first purpose-built hospital from 1711 (albeit without Admiralty or Sick and Hurt Board approval), it was only in 1744 that the decision was made to build dedicated naval hospitals at Portsmouth, Plymouth and Chatham.24,62 Although the last would not be built until 1905, construction began at Haslar in 1746 (Figures 21-23), which began receiving patients in 1754 and had 1800 beds on its completion in 1762. The Royal Naval Hospital at Plymouth was finished the same year with 960 beds, having begun construction in 1758 while receiving its first patients in 1760 (Figures 24-26). Some measure of their importance may be found in the fact that on completion, Haslar was the largest brick-built building in Britain. Although the contract system never died out completely, its subsequent use was strongly discouraged: cases were retained on board whenever possible until their ship returned to Portsmouth or Plymouth. Meanwhile, those landed elsewhere were either returned to their ship or sent to Haslar or Plymouth at the first opportunity.24
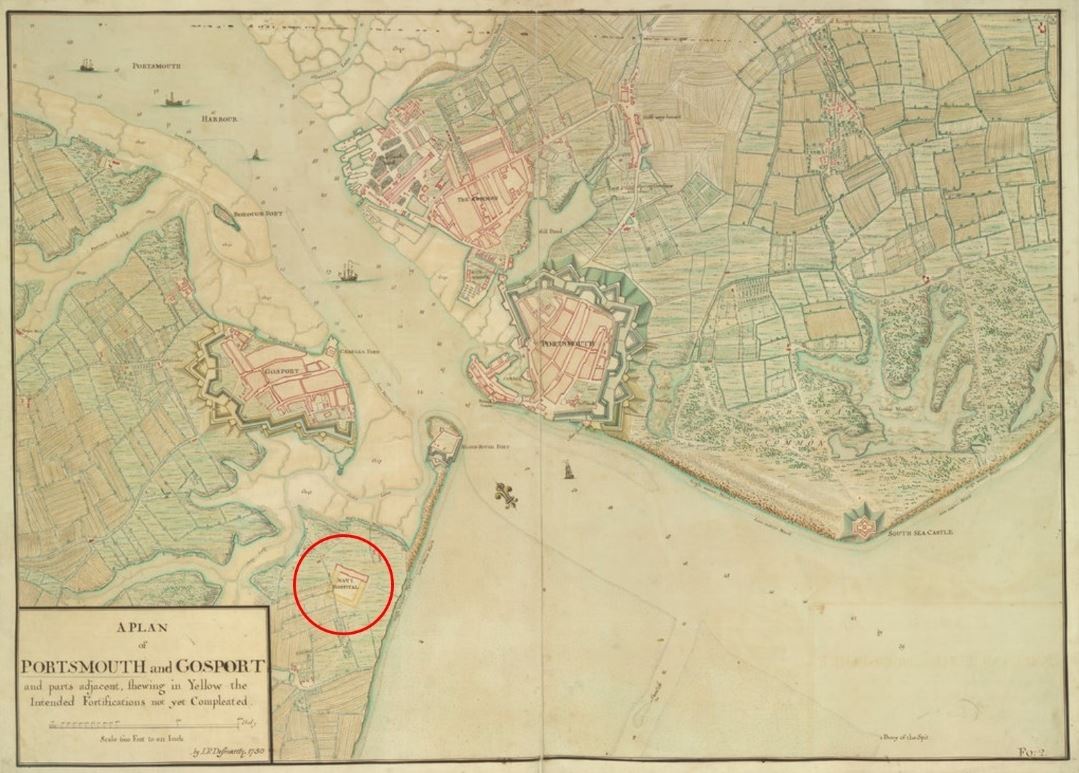
Figure 21. Plan of Portsmouth, 1750, showing Haslar Hospital under construction (circled).63 Note its location on the Gosport peninsula opposite the dockyard: this permitted direct boat access for the ships, limited the infectious disease risk to the local population, and made it harder for convalescents to desert.

Figure 22. Ground floor plan, Royal Naval Hospital Haslar.64 Note the open-sided quadrangle: this required a 3.7 m high iron fence to prevent desertion.

Figure 23. Façade, ex-RNH Haslar, 2009.65 Having been closed at that time, the site has since been redeveloped for retirement housing. The blue doorway of the main entrance seen here had a rail trolley-way to Haslar Creek (to the right) for receiving patients.

Figure 24. Plan of Plymouth, 1820, showing the naval hospital (circled).66 Note its location on Mill Lake (since been reclaimed), which permitted direct boat access for the ships. A surrounding high wall reduced the infectious disease risk for the local population and made it harder for convalescents to desert.

Figure 25. Plan, Royal Naval Hospital Plymouth, 1796.67 The buildings forming the quadrangle constituted the hospital proper; its multi-block design was one of the first in England. The area to the left of the quadrangle is staff accommodation; the large circle shows the boat landing stage and the small circle the water tower per Figure 26.

Figure 26. Water tower inside the wall surrounding ex-RNH Plymouth, 2022. The hospital was closed in 1995 to become the Millfields housing development, which is closed to the public. Note the daunting height of the wall for deserting convalescents. (Author)
Consistent with civilian practice, both hospitals were initially managed by their senior physician, who came to abuse their private practice rights and did not always demonstrate the greater administrative skills required to manage naval rather than civilian patients. Following a Board of Inquiry instigated by Trotter through Howe in 1794 (Figures 27 and 28), executive branch (i.e., non-medical) Captains were appointed Governor (later Superintendent) to command the Haslar and Plymouth hospitals from the following year. Naval hospital command was not returned to the medical branch until 1870.24,25

Figure 27. Dr Thomas Trotter, 1796.68
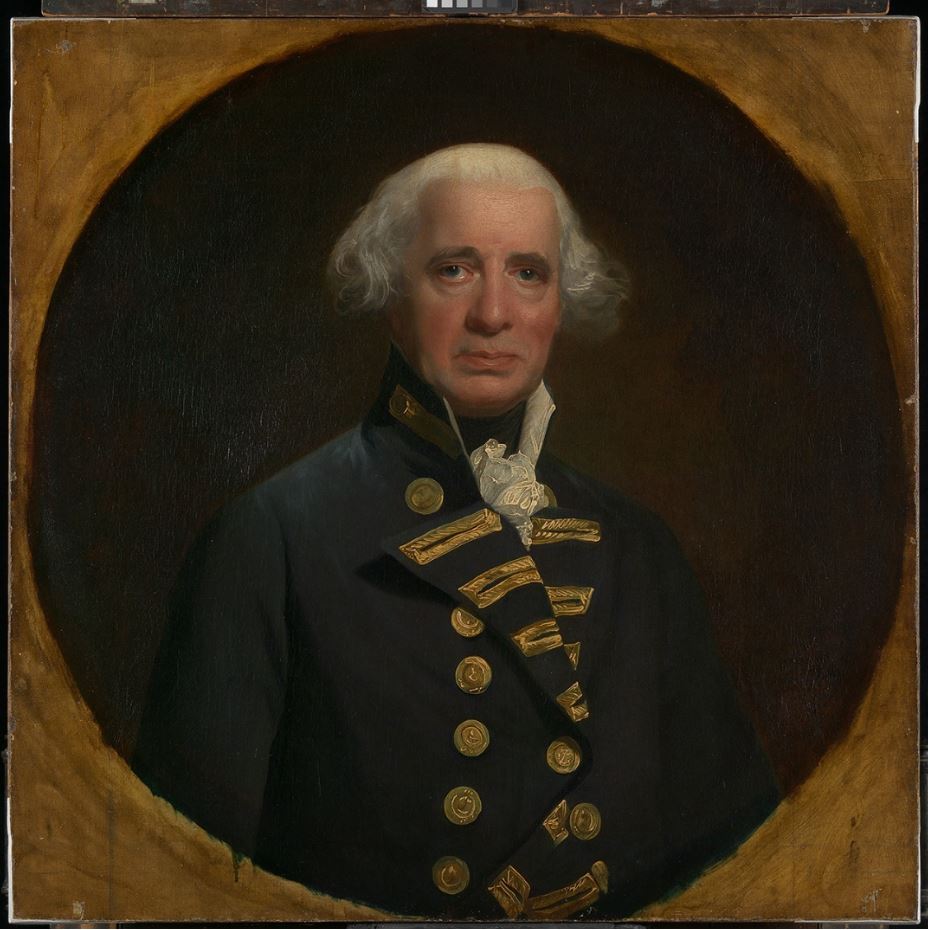
Figure 28. Admiral of the Fleet Earl Richard Howe (1726–1799), 1794.69
Besides improving discipline and administration, this decision immediately affected patients deemed medically unsuitable for naval service. Before 1795, these were ‘surveyed’ by a local board, which provided reports on those deemed to require invaliding to the Sick and Hurt Board. Each survey board comprised three Captains, the hospital physician and surgeon, and the surgeon of the patient’s ship. However, from 1795, their reports were forwarded to the Sick and Hurt Board via the hospital Governor, who acted as the survey board president. This change was most likely made in response to personnel shortfalls, combined with the view that too many men were being invalided unnecessarily. Hence, the Plymouth Hospital Governor, Captain Richard Creyke, chaired 26 survey boards between October 1795 and May 1798, at which—in contrast to previous invalidity acceptance rates of 100 percent—deemed 776 of the 2896 cases (27 per cent) fit for retention, with many fit enough to rejoin their ships.24 In so doing, Creyke demonstrated that although subject to medical advice, medical suitability determinations are ultimately a command responsibility based on service requirements.
Conclusion
By 1805, Nelson could tell Trotter, his Physician of the Fleet, ‘You taught us to keep the seaman healthy without going into port, and to stay at sea without a refit’.24 Statistical evidence to his words came from Blane, who estimated that 135 480 sailors’ lives had been saved between 1793 and 1814, a number equivalent to all RN personnel serving in 1814.70
These advances also made the European settlement of Australia possible without horrendous mortality rates. In a major contrast to Anson 48 years previously, the First Fleet had only 48 deaths from 1403 people (3.4 per cent) between departing Portsmouth in May 1787 and arriving at Botany Bay eight months later.71,72 Despite some egregious failures (notably the Second Fleet in 1790 and the Third the following year), 755 ships transported more than 160 000 convicts over the next 80 years, with an overall average mortality rate of less than two per cent.72
Even so, most solutions to the Navy’s high DNBI rates were not new. Indeed, the need for high-quality hygiene and victualling had been recognised since Tudor times, while lemon juice was first used to treat scurvy by James Lancaster when the East India Company was founded in 1600. Rather, the Navy’s medical successes had been driven by four factors, the first being recognition that the DNBI rates experienced by Hosier and Anson were non-sustainable, given the finite number of trained seamen for the Navy to defend Britain’s expanding maritime trade, and for the maritime trade that funded the Navy. Next came the realisation that most Navy DNBI was, in fact, preventable: Lind by experimentation and observation, and Cook by 10 years’ practical seagoing experience. These two factors contributed to the third: Anson, Lind and Cook each founded their own naval dynasties, whose first-, second- and subsequent generation protégés, at a time when the Navy was heavily dependent on the patronage system, eventually implemented the necessary measures to maintain seagoing health. Finally, none of these advances would have been possible without the necessary funding, which came from the expansion of Britain’s maritime trade that supported—and was supported by—the Navy. In combination, these factors explain why the Navy’s medical reforms began a century before the Army’s medical disasters during the Crimean War begat likewise.
However, it is essential to note that although Lind and his successors provided the ‘what’, Anson and his protégés facilitated the ‘how’. This mainly refers to the first sickbays that made it possible to isolate infectious disease cases at sea, and the divisional system to ensure better personnel hygiene. Furthermore, combatant officers such as Creyke ensured that medical suitability determinations remained a command responsibility based on service requirements, subject to medical advice.
Amid these reforms, the Sick and Hurt Board had a surprisingly limited role. Although the wartime Commissions had introduced the first rudimentary naval medical administrative systems for managing patients ashore from 1653, neither they nor the Board that followed did much more than manage contractors. Escalating costs, poor quality care and failing to manage convalescent cases effectively led to the Navy’s purpose-built hospitals at Haslar, Plymouth and eventually elsewhere. Following the Sick and Hurt Board’s demise in 1806, it was not until 1832 that the Navy had a bespoke medical department that truly centralised naval medical administration ashore and afloat for the first time. This provided the means to advance the naval medical art that supported its worldwide operations over the next century and beyond.
Disclaimer
The views expressed in this article are the author’s and do not necessarily reflect those of the RAN or any other organisations mentioned.






