Introduction
The key functions of military health services[1] include assessing military suitability for military service. This information is used by personnel managers, commanders and supervisors to minimise the impact of:
- medical condition(s) of members which affect their ability to undertake normal workplace duties, and
- the opposite, , i.e. normal workplace duties affecting their medical condition(s).
The process used for this function by the Australian Defence Force (ADF) is at Defence Instruction (General) – Personnel (DI(G) PERS) 16-15 ADF Medical Employment Classification (MEC) System, the latest version of which was released on 01 July 2011.[i]. The updated DI(G) necessitated the development and release of a training package for all uniformed and civilian Defence MOs.[ii].
Description of the ADF MEC System. DI(G) PERS 16-15 requires the medical suitability of every ADF member for employment and deployment to be summarised by:
- A Medical Employment Classification (MEC) alphanumeric code, related to their primary military occupation;
- A specific Specialist Employment Classification (SPEC) alphanumeric code for aircrew, divers, parachutists and submariners, and
- employment restriction or ‘R-codes’, which amplify the member’s allocated MEC/SPEC by highlighting specific employment limitations.
Local ADF health staff are responsible for managing ADF members with short-term employment restrictions (typically less than 28 days) in accordance with DI(G) PERS 16-21.[iii] These cases do not require MEC Review (MECR).
However, ADF members with medium- or long-term employment restrictions (typically more than 28 days), require MECR using a process described in accordance with DI(G) PERS 16-15. There are two types of MECR:
- Unit MECR (UMECR). As a general rule, UMECRs are required for personnel who are unable to deploy or be employed without restrictions in the medium term (typically 28 days to 12 months). UMECRs may be confirmed by local confirming authorities. These are Defence MOs who are credentialed for the role based on their experience and expertise with the ADF MEC System.
- Central MECR (CMECR). As a general rule, CMECRs are required for personnel who are unable to deploy or be employed without restrictions in the long term (typically more than 12 months). All CMECRs require review by Defence MOs at the MEC Advisory and Review Service (MECARS) in Canberra, pending confirmation by the relevant single-Service MEC Review Board (MECRB).
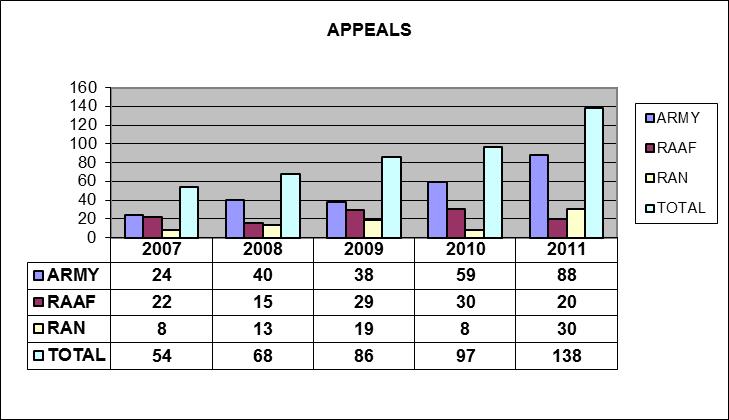
CMECR Quality. MECARS uses a Medical Administration System (MAS) database, to track MECARS taskings. The MAS database shows that, although the number of MECRBs increased by 6.8% per annum in the five years since 01 January 2007 (Figure 1), the number of MECRB appeals has increased by 31.1% per annum over the same period (Figure 2).
Figure 1 – CMECR’s Actioned by MECARS
Figure 2: MECRB Appeals Actioned by MECARS
The MAS database was upgraded in September 2012 to include an administrative and clinical quality tool, which was used on 1210 CMECRs received by MECARS between 01 February and 30 September 2012. This tool confirmed that there is considerable variation in the quality of the CMECR documentation received at MECARS (Figure 3).
|
|
Very Poor |
Poor |
Adequate |
Good |
Very Good |
| Number |
64 |
206 |
412 |
473 |
53 |
| Per Cent |
5.3% |
17.0% |
34.0% |
39.1% |
4.4% |
Figure 3: MECARS CMECR Quality Assessment, Feb-Sep 2012
Literature Review Summary – Wynne-Jones et al. (2010) [iv]. It was thought that the variations in the quality of CMECR documentation may be influenced by the attitude of the MOs who participate in the MECR process. Although time constraints precluded undertaking an extensive literature review, this premise is supported by several papers on the attitudes of general practitioners regarding civilian sickness certification, which were summarised by Wynne-Jones et al. (2010).
Wynne-Jones et al. (2010) is a review of 18 papers (predominantly from Scandinavia and the UK) regarding GP attitudes towards sickness certification. These papers include qualitative, quantitative and systematic reviews. They identified three themes in these 18 papers:
- Conflict. A third of GPs reported sickness certification to be problematic, with many GPs reporting that the handling of sickness certification was difficult on a weekly basis. Half of the GPs found handling disagreements with patients, decisions about the prolongation of certification, assessing patients’ work ability, and the optimum duration of sickness certification fairly or very problematic.
- Role responsibility. Many of the papers reported that GPs often found that their roles in the sickness certification process were unclear and conflicting. Responsibility towards the patients and the UK Department of Work and Pensions (DWP) and the Department of Social Security (DSS) generated some divergence when making the decision to issue a sickness certificate. However, the majority of participants in this study felt their responsibility to their patients outweighed that towards the DWP or DSS. This difficulty in handling the various roles that the GPs play leads to concerns about poor practice and despair in the process as a whole, and the role of the GP in particular.
- Barriers to good practice, both within and outside the healthcare system. Barriers within healthcare systems focused on the GPs own competence in certification decisions, in particular judging incapacity for work and the duration of absence required. It was suggested that although certification should be based on physical health, allowing certification on social grounds would improve practice and reduce some of the perceived conflict within the consultation. This was compounded by conflicting advice from other health professionals who suggest to patients that they need to be absent from work when the GP did not agree. Difficulties working with other colleagues were identified as barriers to practice, with GPs feeling undermined by hospital and other colleagues. Furthermore, a large number of GPs would prefer not to be part of the sickness certification system, suggesting the alternative of an authoritative individual to whom they could refer patients.
Wynne-Jones et al. (2010)4 concluded that any potential for changing the certification system needed to focus on reducing the potential for conflict, clarification of the roles of all stakeholders, and improving access to specialist occupational health and rehabilitation services.[v]
Garrison MO Attitude Survey. In consequence, it was decided to survey the attitudes of uniformed (Navy, Army and RAAF), Australian Public Servant (APS) and civilian Contract Health Practitioner (CHP) MOs regarding their attitude to the ADF MEC system. It is stressed that the purpose of the survey was not to produce a ‘scientific paper’, but to inform how the quality of the MEC documentation received at MECARS could be improved.
Aim
The aim of this paper is to report the results of a survey of the attitudes towards the ADF MEC system of uniformed and civilian Defence MOs who work in the Joint Health Command garrison setting.
Materials and Methods
A questionnaire (Figure 4) was developed and distributed to all participants at the 20th Australian Military Medicine Association (AMMA) Conference held in Melbourne in October 2011. Additional questionnaires were also distributed via email through the JHC garrison organisation. Recipients were requested to complete a hard copy of the survey and fax it to MECARS. The results were entered onto an Excel spreadsheet for analysis using SPSS Statistics Student Version 18.
The survey included demographic questions regarding Service / civilian status, full- or part-time status, location by garrison region, and amount of Defence experience. MOs were then asked to use a five point scale to rate their attitude to their MECR role, MECR training, and what were referred to as ‘tips and tricks’ to make writing MECRs easier. Other questions asked them to rate their attitude towards the intrinsic components of a MECR clinical summary, and the support provided by MECARS. Respondents were also provided with an opportunity to make comments.
Although the validity of the survey instrument was not assessed prior to its implementation, the questions reflect the information routinely required by MECARS MOs in order to perform their review function. As such these questions represent that which should be considered as a matter of course, by treating MOs and confirming authorities during the MECR clinical summary development process.
Ethics approval for the survey was not required, as it was anonymous and did not entail the provision of clinical or other personal information.
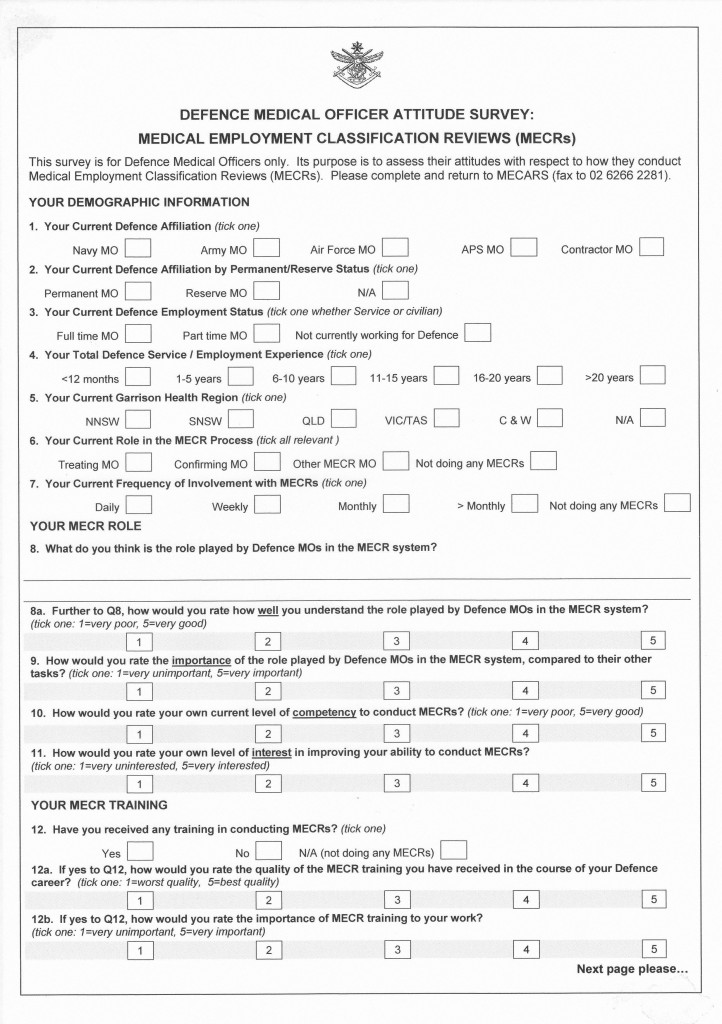 Figure 4 – Defence MO MECR Attitude Survey Instrument
Figure 4 – Defence MO MECR Attitude Survey Instrument
Results
Survey Response Rate. . MECARS received 82 useable questionnaires. Figures provided by garrison operations indicates that there were 520 MOs who provided garrison health care as of 03 November 2011 (15.8%) (Figure 5).
|
Region |
Navy |
Army |
RAAF |
Total ADF |
APS |
CHP |
Total Civilian |
Total |
Responses |
Per cent |
| QLD |
2 |
21 |
10 |
33 |
10 |
55 |
65 |
98 |
25 |
25.5% |
| NNSW |
5 |
16 |
18 |
39 |
13 |
50 |
63 |
102 |
14 |
13.7% |
| SNSW |
31 |
39 |
7 |
77 |
62 |
46 |
108 |
185 |
14 |
7.6% |
| VIC/TAS |
1 |
12 |
3 |
16 |
8 |
24 |
32 |
48 |
6 |
12.5% |
| C&W |
4 |
19 |
12 |
35 |
7 |
45 |
52 |
87 |
16 |
18.4% |
|
43 |
107 |
50 |
200 |
100 |
220 |
320 |
520 |
75 |
14.4% |
|
| Responses |
5 |
19 |
4 |
28 |
2 |
52 |
54 |
82 |
||
| Percent |
11.6% |
17.8% |
8.0% |
14.0% |
2.0% |
23.6% |
16.9% |
15.8% |
Figure 5: Defence MO MECR Attitude Survey – Response Rates[vi]
Demographics. Of the 82 responders, 19 (23.2%) were permanent ADF members, 21 (25.6%) were reservists, and 41 (51.2%) had no uniformed affiliation. In addition:
- 67.1% of valid responders (55) were full time.
- Seven responders (8.5%) had less than 12 months experience of working for Defence; 19 (23.2%) had 1-5 years, 19 (23.2%) had 6-10 years, 10 (12.2%) had 11-15 years, nine (11%) had 16-20 years and 18 (22%) had over 20 years.
- 68.3% of responders (56) undertook their MECR role at least daily, and another 24.4% (20) at least weekly.
- 46 responders (56.1%) did so as treating MOs and 22 (36.8%) as MECR confirming authorities.
MECR Role. The responders rated the following as either ‘good’ or ‘very good’:
- Personal understanding of the MECR process: 82.9%.
- Personal importance of their MECR role: 79.3%.
- Personal competence at conducting MECRs: 71.9%.
- Personal level of interest in their MECR role: 70.9%.
MECR Training. With respect to MECR training for garrison MOs:
- 18.3% had not undertaken any MECR training.
- 29.3% considered the quality of MECR training they had received as either ‘good’ or ‘’very good.
- 73.1% rated the importance of MECR training as either ‘important’ or ‘very important’.
MECR Clinical Summary Content. Garrison MOs rated the following as either ‘important’ or ‘very important’ with respect to MECR clinical summaries:
- providing a detailed description of how ADF members first present with a medical condition requiring MECR: 80%.
- providing a detailed description the relevant clinical history, examination and investigations at that presentation: 86.6%.
- providing a detailed description of the member’s subsequent medical progress with respect to that medical condition: 97.5%.
- providing this information for each of the member’s medical conditions requiring MECR: 90.3%.
- the Member’s Health Statement (MHS): 54.9%.
- the Workplace Disability Report (WDR): 58.5%.
- describing the member’s current prognosis and functional limitations: 91.4%.
- describing the rationale for the recommended MECR: 89.0%.
- providing a clinical summary as a standalone document: 79.3%.
Tips and Tricks. 22% of garrison MOs reported using tips and tricks to reduce the time required to write MECR clinical summaries. However, 83.1% also reported keeping copies of previous MECRs.
MECARS Support. 26.6% considered the support provided by MECARS to be either good or very good, while 37.4% considered MECARS support to be either poor or very poor.
Comments. 76.8% of responders provided comments regarding their MECR role; 28% commented on their MECR training, and 51.2% made general comments on the MECR process.
Discussion
As far as the author is aware, this study represents a first attempt to present information regarding the attitude towards their role of assessing medical suitability for military services of Australian and overseas medical practitioners who provide health services for a military workforce.
Figure 3 shows that 22.3% of CMECRs received at MECARS between February and September 2011 were assessed as either poor or very poor. This represents the provision of suboptimal medical advice with respect to the career management of over 250 ADF personnel – more than a Navy guided missile frigate crew, Army rifle company or RAAF squadron.
Furthermore, variations in CMECR quality has important implications regarding the consistency of UMECR decision-making by confirming authorities at the garrison health unit and regional level, noting that – unlike CMECRs – UMECRs are not subject to oversight by MECARS. This in turn has implications with respect to:
- Ensuring that members with medical condition(s) that do not prevent them from deploying, and are still able to do so. Doing so means more operational strain for other personnel and is likely to affect other personnel management decisions, such as eligibility for courses, posting, promotions, pay and other entitlements.
- Ensuring that people with medical condition(s) that preclude them from deploying are prevented from doing so. These personnel do not facilitate achieving the operational mission, and they can pose a threat to themselves if they are unable to receive the medical care they need, or if the operational setting makes their condition(s) worse.[vii] Less dramatically, preventing medically unfit personnel from deploying also facilitates their rehabilitation and compensation.
Study Limitations. The apparently poor response rate of only 15.8% (Figure 4) precluded the investigation of MO attitudes within the various garrison MO sub-populations (in particular by Service / APS / CHP status, and by garrison region).
Discussion with garrison health staff led to the conclusion that the response rate was affected by local MO workload and ‘survey fatigue’, as apparently indicated by poor response rates to other garrison MO surveys. However:
- There were significant difficulties ascertaining the number of garrison CHPs in particular, given they are provided through third parties, especially if they only work for Defence part-time.
- the number of garrison MOs (520) provided by garrison operations was clearly accurate, noting (for example) the 43 Navy ‘garrison’ MOs per Figure 5 does not reflect the total number of PN MOs (approximately 40), many of whom are not in fact undertaking garrison duties[viii].
This is confirmed by a review of the MECARS MAS database, which found only 264 garrison MOs who had contributed one or more CMECRs between 01 February and 28 September 2012. Although it is likely that there are additional garrison MOs who have not contributed any CMECRs during this period, eight months is considered an ample timeframe for them to have done so. The MECARS database figure is therefore probably more accurate than the number provided by garrison operations. Using the MECARS database number of garrison MOs results in a response rate of 31%, which is somewhat more respectable.
Even so, a 30% response rate to this survey is perhaps itself indicative that the overall attitude of garrison MOs towards the MECR process may not be particularly positive. Furthermore:
- A greater proportion of the garrison MO workforce are likely to have no uniformed (permanent or reserve) affiliation rather than the 51.2% of responders who so indicated.
- The overall level of Defence experience of garrison MOs is probably considerably less than that indicated.
It is therefore appears reasonable that survey responders may represent a ‘best case’ with respect to garrison MO attitudes to the MECR process. This premise is supported by the MECARS database review, which found that 180 of the 264 MOs therein participate in the CMECR process only as treating MOs (68.1%), compared to the proportion of survey responders who reported themselves as such (56.1%).
MECR Role. This conclusion is further supported by the proportion of responders who rated their understanding of the MECR process as ‘good’ or ‘very good’ (82%). The quality of MECRs and the nature of the queries received at MECARS, makes it very unlikely that the garrison MO workforce possesses anything like this level of understanding. Similar conclusions are drawn regarding the perceived importance of their MECR role, their MECR competence, and their level of MECR interest. This is further supported by many of the responder’s comments (see below).
MECR Training. The fact that 73.1% of responders rated the importance of MECR training as important or very important is encouraging. However, despite the MECR training being a mandated requirement prior to undertaking MECRs, 18.3% had still not undertaken such training. Furthermore, only 29.3% of responders characterised the MECR training they had received as good or better. This indicates the need to significantly improve the quality and reach of MECR training for garrison MOs. This conclusion is also supported by many of the responder’s comments (see below).
MECR Clinical Summary Content. The high ‘important or very important’ response rates (around 80% or more) to most of the survey questions related to MECR clinical summaries is also encouraging.
The lowest ‘important or very important’ response rates were for the MHS (54.9%) and WDR (58.5%). It is noted that, as they are completed by the member and commanding officer respectively, that obtaining them in a timely manner can be problematic. It is also accepted that treating MOs should be aware of the member’s attitudes regarding their workplace in any case, as part of the normal doctor-patient relationship.
However, it is unclear how treating MOs can properly assess the MEC status of their patients in the absence of documentation from both the member and the workplace regarding their (perceived) level of workplace disability. This in turn suggests that the level of understanding, importance, competence and interest with respect to the MECR is perhaps not as high in practice as was indicated elsewhere in the survey.
Reference is also made to the 22% who reported using tips and tricks to reduce the time required to write a MECR clinical summary. This is clearly far fewer than should be expected, given the level of experience, and frequency with which the responders undertake MECRs (63.3% at least daily).
This suggests that there is considerable wasted effort expended on duplicating clinical summary information that is already available on previous MECRs. This in turn suggests that the level of understanding, importance, competence and interest with the respect to the MECR is perhaps not as high in practice as was indicated elsewhere in the survey. It is also suggested that this highlights deficiencies with the current MECR information technology processes (in particular, access to MECRs done by other MOs). This conclusion is further supported by many of the responder’s comments (see below).
MECARS Support. Responders characterised the support provided by MECARS to be poor: the 26.6% who considered it to be either good or very good is exceeded by the 37.4% who considered MECARS support to be either poor or very poor. Furthermore, some of the comments indicated a lack of awareness of the existence of MECARS.
It is accepted that MECARS can be fairly demanding as to what is required from treating MOs and confirming authorities with respect to getting useable CMECRs. Follow up feedback was therefore sought via email regarding what treating MOs, confirming authorities and other stakeholders would like from MECARS in return. These responses indicated more frustration with the MECR process than with MECARS per se. Particular reference was made to the timeframes for MECRB determinations, and a new form was used for the MEC process for a short period before reverting to the previous version.
MECARS had previously made representations to undertake a travelling roadshow to address training and enhance communication, however this could not be supported because of resourcing issues. The MECARS website[ix] had also been substantially revised, with a dedicated resources page[x] including PowerPoint presentations, desktop information sheets, and a series of MECR training scenarios.
Respondent Comments. Main respondent comment highlights (good points) included:
- Many respondents are keeping copies of MECRs as a basis for writing the next one. Many comments referred to the need to improve how these are shared between treating MOs.
- There was one (but only one) reference to the improved flexibility of the new MEC system.
Main respondent comment highlights (room for improvement points) included:
- There appears to be a high level of understanding that the MECR process is important, but not actually why it is important.
- Furthermore, some of the ‘understanding’ is incorrect: particularly the fact that the purpose of the MECR process is to facilitate personnel – not clinical – management.
- There were multiple references to the need for enough time to conduct MECRs properly.
- There were, however, many more references to the need for better MECR training.
- There were also multiple (but fewer) references to the need for better information technology (IT) support.
- There were a few references to variations between the confirming authorities (which supports the view of MECARS staff regarding the variation in the quality of the CMECR documentation they receive, and which led to this study).
Conclusions
- Although the poor response rate significantly reduced the scope of this study, it was still possible to draw some valid conclusions based on the premise that the responders most likely represent a ‘best case’ with respect to MO attitudes to the MECR process.
- Although the understanding of the MECR process, the importance of the MECR role, their MECR competence, and the level of MECR interest appear generally good among the responders, it appears unlikely that they represent the garrison MO population as a whole.
- There is a need to significantly improve the quality and reach of MECR training for all garrison MOs.
- The lower ‘important or very important’ response rates for the MHS and WDR suggests that the level of understanding, importance, competence and interest with the respect to the MECR is perhaps not as high in practice, as indicated elsewhere in the survey.
- The low proportion of responders who reported using tips and tricks to reduce the time required to write a MECR clinical summary also suggests that the level of understanding, importance, competence and interest with the respect to the MECR process is perhaps not as high in practice, as indicated elsewhere in the survey. It also suggests that there is considerable wasted effort expended on duplicating MECR information that is already available on previous MECRs, and highlights deficiencies with MECR information technology processes.
- Followup regarding the perceived poor or very poor MECARS support indicated frustration with the MECR process, rather than MECARS per se. Particular reference was made to the timeframes for MECRB determinations, and the new form used for the MEC process that has since been withdrawn.
- Responder’s comments generally supported these conclusions (particularly with respect to training, and variations between confirming authorities). However, they also indicated that the actual level of understanding among responders regarding their MECR role is less than they perceive, while highlighting the need for better IT support, and time to conduct MECRs properly.
In short the attitude survey results suggest that at least 20% of Defence MOs have a ‘poor’ or ‘very poor’ attitude with respect to their participation on the ADF MEC system. This finding appears generally consistent with the review paper by Wynne-Jones et al (2010)4.
Issues related to CMECR quality should form the basis for further study. However the attitude survey results suggest they are generally consistent with the fact that about 20% of the CMECRs received by MECARS are assessed as either ‘poor’ or ‘very poor’. As an aside, there is a need to assess UMECR quality on comparable terms as the MAS quality assessment tool used by MECARS for CMECRs.
The survey findings suggest that consideration should be given to incorporating MECR quality as a performance indicator for all Defence MOs who participate in the ADF MEC system. Such a ‘MECR quality performance indicator’ should form part of the performance appraisal / contract renewal process for treating MOs and confirming authorities.
Respondent feedback reiterates the need to significantly improve the quality and reach of MECR training for all garrison MOs. Such training should highlight why the MEC process is important, and the need to effectively use the information provided in the WDR and MHS. MOs also need more time and improved MEC IT support in order to write better clinical summaries. Consideration should also be given to identifying where the MEC process can be simplified.
[1] The functions and roles of military health services include the following:
- Operational Health Support. The primary reason for the existence of military health services is to provide health support for military personnel wherever and whenever they operate.
- Medical Evacuation. The fact that military personnel could end up in isolated places means that they may need evacuation if they are ill or injured.
- Humanitarian Aid / Disaster Relief. This may be a primary role, or a subset of operational health support, possibly using different facilities according to the needs of the potential recipient(s). .
- Military Medicine Capabilities. These include aviation, underwater and CBR medicine.
- Assessing Medical Suitability for Military Service. Military health staff need to ensure that personnel managers, commanders and supervisors are aware of the health status of those for whom they are responsible r .
- Occupational and Environmental Health. There is a need to ensure that military workplaces are not permitting preventable illness or injury.
- Health Promotion. There is a need to ensure that processes are in place to maximise the general health and wellbeing of military personnel.
- Treatment Services. This refers to the provision of primary, secondary and tertiary level care, in both the deployed and non-deployed (garrison) setting.
These functions and roles are ranked such that, as one goes up this listing, so the level of military-specific expertise required to undertake them increases.
[i] Department of Defence, 2011, DI(G) PERS 16-15 ADF Medical Employment Classification System [online] https://intranet.defence.gov.au/home/documents/data/ADFPUBS/DIG/gp16_15.pdf, [2012, 26 Apr]
[ii] Joint Health Command, 2011, ‘Medical Employment Classification System: User / Exponent Training’, [CD-ROM], version 1. [2012, 28 Apr].
[iii] Department of Defence, 2011, DI(G) PERS 16-21 Sick Leave and Convalescence Leave—Defence Members [online] https://intranet.defence.gov.au/home/documents/DATA/ADFPUBS/DIG/gp16_21.PDF, [2012, 30 Apr]
[iv] Wynne-Jones G, Mallen C.D, Main, C.J. Dunn K.M. What do GPs feel about sickness certification? A systematic search and narrative review. Scand J Prim Health Care. 2010 Jun;28(2):67-75 [online] https://informahealthcare.com/doi/abs/10.3109/02813431003696189. [ 2012, 08 May].
[v] Wynne-Jones G, Mallen C.D, Main, C.J. Dunn K.M. What do GPs feel about sickness certification? A systematic search and narrative review. Scand J Prim Health Care. 2010 Jun;28(2):67-75 [online] https://informahealthcare.com/doi/abs/10.3109/02813431003696189. [ 2012, 08 May].
[vi] Email Jason Kerr to Neil Westphalen 3 Nov 11 16:59
[vii] Department of Defence, 2007, ‘Report of Board of Inquiry into the Death of CAPT Paul Lawton’, [online], https://www.defence.gov.au/coi/reports/Lawton_R.pdf, [2012, 02 May]
[viii] Review of the “Health Service Officer Spreadsheet Dec 10” at DNH found approximately 40 currently serving PN MOs, most of whom were engaged in staff duties, assigned to the Fleet Pool, or undergoing initial entry training. It is therefore estimated that only around ten PN MOs are engaged in garrison health roles at any one time, rather than the 43 per Figure 5.
[ix] Joint Health Command Directorate of Military Medicine, 2012, Medical Employment Classification Advisory and Review Service (MECARS) [online] https://intranet.defence.gov.au/vcdf/sites/MECSystem/comweb.asp?page=79004&Title=Functions, [2012, 30 Apr]
[x] Joint Health Command Directorate of Military Medicine , 2012, MECARS – Resources [online] https://intranet.defence.gov.au/vcdf/sites/MECSystem/comweb.asp?page=79013&Title=Resources, [2012, 30 Apr]