Abstract
Background: Pelvic floor dysfunction (PFD), encompassing urinary incontinence (UI), anal incontinence (AI), pelvic organ prolapse (POP) and various other conditions associated with pelvic floor muscles, is prevalent in military women and female elite athletes. Thus, it is important to consider specific prevention and management strategies that these women are currently using, and their safety and effectiveness.
Purpose: To determine specific prevention and management interventions for UI, AI and POP used by female military personnel and elite athletes, and their safety and effectiveness.
Materials and methods: Eight databases were searched for studies on prevention and management of UI, AI and POP using keywords such as ‘female’, ‘military’, ‘athlete’ and ‘pelvic floor dysfunction’. Studies were selected and appraised by two independent reviewers. Data were extracted, and a critical narrative synthesis approach was implemented.
Results: The systematic search identified 581 studies; eight were eligible for inclusion in the review. Seven studies focused on UI and one on AI. Pelvic floor muscle training (PFMT) was common and effective in studies of military women and female athletes experiencing UI symptoms. Education was beneficial in female athletes. Concerningly, fluid restriction and pad use were key self-management strategies.
Conclusion: PFMT was the most widely used intervention for prevention and management of UI in female military and athlete populations and was found to be safe and effective.
Introduction
Pelvic floor dysfunction (PFD) in women encompasses a variety of conditions affecting the bladder, bowel and sexual function, such as incontinence and pelvic organ prolapse (POP).1 Urinary incontinence (UI) is the most prevalent type of PFD and involves involuntary urine leakage.2 Anal incontinence (AI) is the involuntary leakage of gas, liquid or solid stool.2 POP refers to the descent of the bladder, uterus and/ or rectum within the pelvis.3 UI, AI and POP together affect approximately 46% of Australian women and so, collectively, are common.4 Further to this, there is an 80% chance that women involved in running and jumping activities will experience one or more of these conditions.5 Together, UI, AI and POP may be considered a significant risk for women in this context.3 Additionally, women who experience these conditions may have to alter their involvement in occupational tasks due to the impacts of the condition on their health and physical performance.6
Female elite athletes with high levels of training, as opposed to generally active women, may be at an increased risk of UI, AI and POP; however, prevalence rates vary across studies. One systematic review reported that 19–76% of female elite athletes experience UI symptoms,7 whereas a primary study reported a specific prevalence of 47%.8 Remarkably, female athletes are nearly three times more likely to experience UI symptoms than women who live a sedentary lifestyle.7 One proposed reason for the higher prevalence of UI in female athletes is that repetitive increases in intraabdominal pressure experienced during exertion lead to downward stress on the structures of the pelvic floor.9 As UI, AI and POP together have a relatively high prevalence in the female athlete context, it is important to determine prevention and management strategies to reduce their impacts. From an extensive search of the literature, only one systematic review explored prevention and management strategies for these conditions in female elite athletes, focusing specifically on UI.10 While moderate evidence for pelvic floor muscle training (PFMT) was found, the systematic review was published several years ago and based its findings on studies published earlier still. In addition, it did not consider AI or POP. As a result, an updated synthesis of studies examining how female elite athletes can prevent and manage UI, AI and POP is required.
As part of their daily occupational tasks, military women may be required to participate in intense physical training and lifting or carrying items such as equipment or heavy backpacks.11,12 This may also place them at risk of developing incontinence or POP,12,13 potentially impacting their occupational performance.3 Approximately one-third of military women are reported to experience symptoms of these conditions.14,15,16,17 Therefore, it is valuable to determine specific interventions used by female military personnel and understand how effective and safe these have been shown to prevent or reduce the effects of UI, AI and POP.
Aside from the systematic review focused on female athletes previously discussed, a preliminary search of eight databases identified no other published systematic reviews focused on prevention and management strategies for female athletes or military personnel. Therefore, this systematic review aimed to determine the current extent to which specific prevention and management interventions for UI, AI and POP have been studied in female military and athlete populations and how effective and safe these have been found to be.
The specific research questions to be investigated in this review are:
- What interventions are currently used to prevent UI, AI and POP in female military personnel and elite athletes?
- What interventions are currently used to manage existing UI, AI and POP in female military personnel and elite athletes?
- How effective and safe are these interventions in preventing and managing UI, AI and POP in military women and female elite athletes?
Methods
This systematic review was conducted in accordance with a protocol preregistered with PROSPERO18 (www.crd.york.ac.uk/prospero/display_record. php?RecordID=161062). The Joanna Briggs Institute (JBI) SUMARI platform was used in its development.19 This platform supported sequential progress through each step of the systematic review, particularly data management.
Information sources
A systematic search of literature databases was conducted on the 6 December 2019, including CINAHL, the Cochrane database, the Defence Technical Information Centre, the Nursing and Allied Health Database, ProQuest Dissertations & Theses Global, PubMed, SportsDiscus and WorldCat. In order to ensure a comprehensive search, the reference lists of studies selected for inclusion were reviewed to identify any further potentially eligible articles.
Search strategy
The key terms for which searches were conducted in the title, abstract and keyword fields of indexed articles in each database were: woman, women, female, pelvic floor dysfunction, incontinence, prolapse, military, soldier and athlete. Variations of the search strategy, adapted to the respective database, were employed. For example, the search strategies used in CINAHL to identify studies involving military women and female athletes, respectively, were (female OR wom*n) AND (pelvic floor dysfunction OR incontinence OR prolapse) AND (militar* OR soldier*) as well as (female OR wom*n) AND (pelvic floor dysfunction OR incontinence OR prolapse) AND (athlet*). Search strategies employed in the different clinical literature databases are provided in Appendix C.
Study screening and selection
Two independent reviewers assessed articles to determine their eligibility for inclusion in the review. First, the titles and abstracts of articles were screened to remove duplicates. Second, the titles and abstracts of retained articles were screened to exclude clearly ineligible articles. Lastly, the full texts of the remaining articles were obtained and examined to determine eligibility. If disparities or differences in opinion arose between the reviewers, they were resolved by discussion and consensus. A third reviewer was available to moderate but was not required during this stage.
Studies were considered for inclusion in the review if they:
- included women over the age of 18 years currently serving in the military; and/or
- included female veterans over the age of 18 years who were previously in the military; and/ or
- included female elite athletes over the age of 18 years; and
- investigated interventions for prevention or management of UI, AI and/or POP; and
- were published in English; and
- were published between 1994 and 2019.
Studies were excluded from the review if they:
- involved male participants only or data for women could not be readily extracted in studies involving participants of both sexes
- involved only participants under the age of 18 years or data for participants over 18 years of age could not be readily extracted in studies of mixed age groups
- involved participants who were not in the military, not veterans and not elite athletes
- did not document ethics approval to conduct the study
- constituted literature reviews or other secondary research
- were not published in English
- were published prior to
Reports of primary research with any type of design were included to ensure that any relevant evidence was considered. The ethics approval criterion listed above assumed that documented ethics approval meant the respective study had taken steps approved by a properly constituted ethics committee to manage any significant risk of potential harm to participants.2 The decision to extend inclusion to all studies published between 1994 and 2019 rather than a shorter period was made to increase the volume of studies eligible to be included, as it was apparent that a relatively small number of studies had been published in this topic area. Furthermore, including studies from a longer period allowed for a longitudinal aspect of the review, as PFD prevention and management interventions may have changed over time and differ now to 25 years ago.
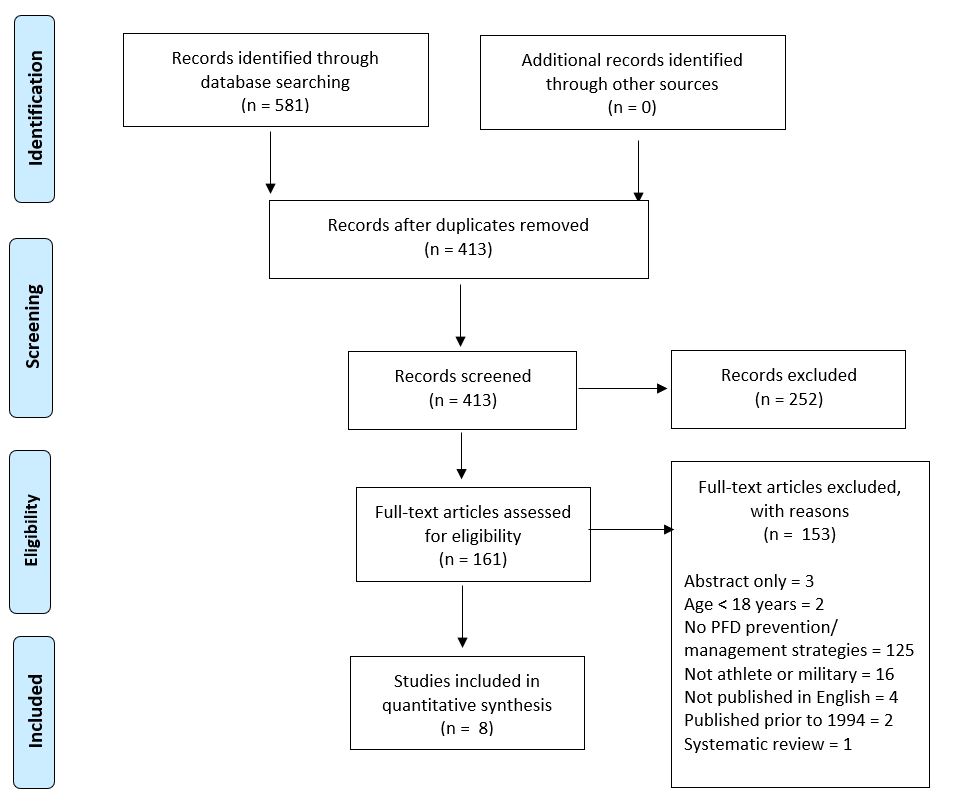
The search, screening and selection processes results were documented in a Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) diagram.21 This type of flow chart depicts the number of research articles found, how many were excluded and for what reasons at each stage of the screening and selection process, and numbers ultimately included in the review.22
Assessment of methodological quality
The Mixed Methods Appraisal Tool (MMAT) was primarily used to appraise the methodological quality of most of the included studies (but not the included case studies).23 This tool was selected because it can be used to appraise qualitative research, randomised controlled trials, non-randomised studies, quantitative descriptive studies and mixed methods studies23. The advantage of using the MMAT is that it is easy to use while providing a large amount of guidance on how to apply it to different study designs. The MMAT involves using a checklist to screen articles, which varies with the study design.23 This checklist incorporates questions with ‘yes’, ‘no’, ‘unclear’, or ‘can’t tell’ responses. It also provides in- depth notes to guide researchers in how to respond to the questions. The JBI critical appraisal tool was used to assess methodological quality for the three case studies included in the review.19 Due to the nature of these studies, they did not fit with the categories in the MMAT. Therefore, it was determined that the use of the JBI tool would be beneficial to ensure objectivity and limit bias in appraisal.
Data extraction
The initial data extracted from each of the included articles included the title, authors, year the study was published and study design. Next, types of prevention and management strategies used by military women or elite athletes to address UI, AI and POP, as well as any findings regarding the effectiveness of these strategies, were extracted. Further data extracted from the studies included age of participants, what branch of the military participants served in, and, if participants were athletes, their levels of participation. Outcome measures and a description of any other relevant results of the studies were also recorded, along with details of participant attrition, adherence to experimental protocols and adverse outcomes, as well as treatment effects.
Data synthesis
The findings of the included studies were synthesised using a critical narrative approach. Narrative synthesis involves the use of text, tables and figures to condense and validate the results of a research process.24 In the analysis of the results, greater weight was given to findings from studies of higher methodological quality and limitations of the included studies, together with possible biases, were considered, thus providing a critical perspective in the review. A statistical synthesis or meta-analysis approach was not suitable for this study as there was a limited number of relevant studies. A variety of interventions, research designs and outcome measures were also used, creating considerable heterogeneity across the included studies.
Results
A total of 581 articles were identified via database searching, from which 161 full-text articles were assessed for eligibility following initial screening and removal of duplicates. A total of 153 full-text articles were excluded leaving eight studies in the review, six involving military personnel and two involving athletes. Results of the search, screening and selection processes are documented in the PRISMA diagram in Figure 1.
Figure 1. PRISMA flow diagram depicting outcomes of the literature search, screening and selection processes
The methodological quality of the included studies was deemed to be moderate to good overall and findings in this regard for each study are detailed in Tables 1 and 2. However, the majority (six of the eight included studies) were not published within the last 10 years and so did not constitute recent evidence.8,14,25,26,27,28
Tables 3, 4 and 5 present an overview of data from the eight studies in the review, along with their key findings. Table 3 encapsulates the key information from the three military studies included in the systematic review that used survey or quasi- experimental designs. All of these studies involved US Army women experiencing UI. Table 4 summarises the key information from the three military case studies included in the systematic review. Each of these reported a case study of one female from the US Army and, of these, two focused on UI and one on AI. Table 5 presents key information from the two athlete studies included in the systematic review. Both studies were focused on UI.
Table 1. Quantitative studies: quality appraisal results based on the MMAT22
| Quantitative randomised controlled trials | Ferreira et al. (2014) | |
|---|---|---|
| Screening questions (for all types) S1. Are there clear research questions? |
Yes | |
| S2. Do the collected data allow to address the research questions? | Yes | |
| 2.1. Is randomization appropriately performed? | Yes | |
| 2.2. Are the groups comparable at baseline? | Yes | |
| 2.3. Are there complete outcome data? | Yes | |
| 2.4. Are outcome assessors blinded to the intervention provided? | No | |
| 2.5 Did the participants adhere to the assigned intervention? | Can’t tell | |
| Quantitative nonrandomized | Davis et al. (1998) Sherman et al. (1997) | Davis et al. (1998) Sherman et al. (1997) |
| Screening questions (for all types) S1. Are there clear research questions? |
No | Yes |
| S2. Do the collected data allow to address the research questions? | Yes | Yes |
| 3.1. Are the participants representative of the target population? | Yes | Yes |
| 3.2. Are measurements appropriate regarding both the outcome and intervention (or exposure)? | Yes | Unclear |
| 3.3. Are there complete outcome data? | Yes | Yes |
| 3.4. Are the confounders accounted for in the design and analysis? | Yes | No |
| 3.5. During the study period, is the intervention administered (or exposure occurred) as intended? | Yes | Unclear |
| Quantitative descriptive | Criner (2008) | Dockter et al. (2005) |
| Screening questions (for all types) S1. Are there clear research questions? |
Yes | Yes |
| S2. Do the collected data allow to address the research questions? | Yes | Yes |
| 4.1. Is the sampling strategy relevant to address the research question? | Yes | Can’t tell |
| 4.2. Is the sample representative of the target population? | Yes | Can’t tell |
| 4.3. Are the measurements appropriate? | Yes | Yes |
| 4.4. Is the risk of nonresponse bias low? | Yes | N/A |
| 4.5. Is the statistical analysis appropriate to answer the research question? | Yes | Yes |
Table 2. Case reports: quality appraisal results based on the JBI critical appraisal tool
| Questions | O’Boyle et al. (2004) | Painter et al. (2007) | Seward (2013) |
|---|---|---|---|
| Were patient’s demographic characteristics clearly described? | Unclear | Yes | Unclear |
| Was the patient’s history clearly described and presented as a timeline? | Yes | Yes | Yes |
| Was the current clinical condition of the patient on presentation clearly described? | Yes | Yes | Yes |
| Were diagnostic tests or assessment methods and the results clearly described? | Yes | Yes | Unclear |
| Was the intervention(s) or treatment procedure(s) clearly described? | Unclear | Yes | Yes |
| Was the post-intervention clinical condition clearly described? | Unclear | Yes | Yes |
| Were adverse events (harms) or unanticipated events identified and described? | Unclear | N/A | N/A |
| Does the case report provide takeaway lessons? | Yes | Yes | Yes |
Synthesis
The included studies provided evidence regarding a narrow range of PFD prevention and management strategies for UI and AI used by military women and female elite athletes. Seven studies focused specifically on strategies for prevention or management of UI,8,14,25,26,28,29,30 with the other being a military case study on surgery as a treatment option for AI.27 None of the studies investigated prevention and management strategies for POP. All six military studies were limited to Army women, with women from other Services (for example, Air Force or Navy) not included in any published studies. The two athlete studies both investigated UI in college8 and volleyball29 athletes. Seven of the included studies were conducted in the USA, while the remaining study was conducted in Portugal. Of note, none of the included studies were conducted on Australian military women or athletes.
One study, by Ferreira and colleagues29 was a randomised controlled trial of pelvic floor muscle (PFM) education, with and without the addition of PFMT, to manage stress UI in female volleyballers. It was deemed to be of satisfactory methodological quality and on that basis provided level II evidence that education in conjunction with PFMT was more effective than education alone.31 The remainder of included studies were determined to provide evidence designated level III and lower.31 Risk of bias in most of the included studies was significant due to lack of control groups, assessors not being blinded to the interventions investigated, and attrition. Further study limitations determined during the critical appraisal stage of the review are presented in Tables 1 and 2. Nevertheless, the evidence provided by the included studies on PFMT as a key intervention for incontinence symptoms exhibited good consistency and potential for good clinical impact, particularly as the populations investigated in the studies were of high relevance for the review questions.31 The study settings were similar to military, athlete and healthcare contexts within Australia; however, the results may not be entirely generalisable to contemporary military women, particularly those in the Navy or Air Force.31
PFMT was investigated in all seven of the UI studies as both a prevention and management option for UI and was reported to improve UI symptoms. However, PFMT was interpreted, implemented and assessed differently across the included studies. PFMT was the most frequently reported self-management strategy for UI utilised by deployed Army women in a survey reported by Criner (78%).25 Despite this, no information regarding the definition of PFMT, exercise dosage, technique, frequency of training or level of instruction was reported in that study.25 In four other studies included in this review, women were instructed on the importance of PFMT and were guided on incorporating exercises into home exercise programs.14,26,28,30 The findings of this review suggest that to be effective, PFMT should be performed by Army women and female athletes at least three times per day for 10–15 repetitions,28,30 and should include sustained contraction and relaxation for 10 seconds.14,26,29 Two single case studies, each involving a female Army soldier reported no UI symptoms at 6 and 12 months following 6- and 12-week PFMT programs, respectively.28,30 It is important to note that these PFMT programs did not occur in isolation and reported outcomes are due to the combination of PFMT with clinic therapy sessions involving upper and lower limb strength training and conditioning.28,30
Table 3. Military survey and quasi-experimental studies: key data and findings
| Author/ Year/ Country | Study design | Participant Characteristics | Prevention/ management interventions | Outcomes measures | Description of main results |
|---|---|---|---|---|---|
| Criner JA. (2008). USA | Quantitative descriptive (cross-sectional survey) | N = 69 female army personnel with SUIa Mean age: 40.12 years Mean BMIb: 25.4 Mean height: 162.6cm Mean weight: 66.7kg Ethnicity: 71% Caucasian, 13% African American, 16% Other Rank: 68.1% officers, 31.9% enlisted Job: 53.6% registered nurses, 27.5% licenced practical nurses, 14.5% other Health history: 70% pregnant at least once Median parity: 2 SUI for >1year: 78% Mild-moderate symptoms: 94.2% |
N/A | Demographic data form UDI-6 MFBC MFCC WOCQ IIQ |
Low response rate (18%) weight = SUI symptoms time with SUI = i QOLj symptom distress = QOL field barriers = coping styles/ problem-solving strategies field barriers = QOL Self-management strategies reported: 78.3% PFMk exercises 78.3% panty liners 71% limit fluid intake 66.7% change underclothes frequently 62.3% use the restroom more often 17% avoid exercises 8.7% avoided strenuous exercise |
| Davis et al. (1998). USA |
Quasi- experimental (observational) |
N = 50 active duty female soldiers with UIl (EGm), 10 asymptomatic soldiers (CGn) Mean age: EG: 31.9 years, CG: 36.4 years Mean weight: EG: 63.5kg, CG: 64.9kg Mean height: EG: 164.1cm, CG: 161cm Parity: EG:1.4, CG: 1.5 |
CG and EG: PFM exercises (2 month program, 10s contraction/ 10s relaxation, 20mins, 2xday) |
Urodynamics 6-month follow-up questionnaire |
CG and EG: Improved subjective ratings of UI severity post-training: severity of UI symptoms, pre- training 81%, post-training 12% Daily episodes of UI: 3.83 UI episodes per day to 1.83 UI episodes per day Urgency symptoms: 85% to 70% post-treatment Participants who continued PFM exercises for 6 months = minimal/ no urinary loss Attrition: 12 participants with UI not included due to being transferred |
| Sherman et al. (1997). USA |
Quasi- experimental (controlled trial) | N = 39 active duty female soldiers with UI Mean age: 28.5 years Mean parity: 1.28 Ethnicity: 55.9% Caucasian, 32.7% African American, 8.3% Hispanic, 3.1% other 21.7% had used PFM exercises before, 2% regularly |
PFM exercises with/without biofeedback (2 month program, 10s contraction/10s relaxation, 5 times with 30s rest between each trial) |
Urodynamics Pelvic examination |
PFM exercises with/without biofeedback reduced UI symptoms, no differences between groups. CG: Mean number of leaks: 7.27 episodes to 2.9 episodes Mean number of voids per night: 0.65 to 0.26 Mean fluid intake per day: 1.5L to 1.7L Self-management strategies reported: 13.3% restrict fluids Attrition: 4 dropped from PFM exercise only group due to receiving electromyographic feedback, 2 dropped out from pre- existing injury to PFM and opted for surgery, 1 dropped out due to diagnosis changing |
a: stress urinary incontinence; b: body mass index; c: urogenital distress inventory short form; d: military field barrier checklist; e: military field coping checklist; f: ways of coping questionnaire; g: incontinence impact questionnaire; h: increased; i: decreased; j: quality of life; k: pelvic floor muscle; l: urinary incontinence; m: experimental group; n: control group
Table 4. Military case studies: key data and findings
| Author/ Year/ Country | Participant Characteristics | Prevention/management interventions | Outcomes measures | Description of main results |
|---|---|---|---|---|
| O’Boyle et al. (2004). USA | 36-year-old active duty female soldier 12-year history of anal incontinence |
Daily pad use (self-management) Anal sphincteroplasty and perineorrhaphy (surgery) |
Symptoms Rectal examination |
12 months post: Good anal tone Continent |
| Painter et al. (2007). USA | 35-year-old female soldier with SUIa United States of America Army basic combat training SIJb pain: 5-6/10 at rest, 7/10 running Parity: 4 (3 vaginal delivery, 1 emergency caesarean) Past History: Left proximal diaphyseal femur fracture (ORIFc), Left greater trochanteric bursitis, leg length difference Posture/gait: ‘normal’, Lumbar extension & right lateral flexion reduced by 25% |
Fluid restriction and pads (self-management) Therapy sessions: Twice per week for 3 weeks: Stationary bike warm-up Weightbearing left hip strengthening exercises PFMd exercises Ice General aquatic program SIJ belt HEPe: 10-12 reps of PFM exercises, 3-5x a day |
Lumbar active ROMf Self-report of amount of urinary leakage Pain ASLRg test |
After 6 weeks of treatment: Normal, pain-free lumbar ROM & hip strength Negative ASLR test Good lumbopelvic control SIJ belt while running and jumping Denied urinary leakage 2 month follow-up: Basic combat training, SIJ pain resolved, no leakage 6 month follow-up: Return to full activity, full duties, no issues, no fear of leakage Yoga 2-3x a week |
| Seward S. (2013).USA | 31-year-old female soldier 5-year history of SUI (during deployment) SIJ pain Gait: “normal” lumbar & hip ROM: “normal” hip MMTh: “normal bilaterally” |
PFM exercises and pads (self-management) Therapy sessions: 10 clinic assessments and PFM exercises for 45 mins over 12 weeks HEP: 10-15 reps of sequenced PFM and TAi exercises at least 3 times per day |
Patient report ICIQ-UI SF | After 6 weeks of treatment: No reports of urinary leakage when coughing/ sneezing 12 week follow-up: Stopped absorbent pad use Lifting heavy boxes was only aggravating factor 12 month follow-up: Nil issues |
a: stress urinary incontinence; b: sacroiliac joint; c: open reduction internal fixation; d: pelvic floor muscle; e: home exercise program; f: range of motion; g: active straight leg raise test; h: manual muscle testing; i:transversus abdominis; j: International Consultation on Incontinence Questionnaire for Urinary Incontinence Short Form
Table 5. Athlete studies: key data and findings
| Author/ Year/ Country | Study design | Participant Characteristics | Prevention/management interventions | Outcomes measures | Description of main results |
|---|---|---|---|---|---|
| Dockter et al. (2005). USA | Quantitative descriptive | N = 109 female collegiate athletes (EGa), 68 non- athletes (CGb) Mean age: EG: 19.17 years, CG: 18.82 years Height: EG:168.07cm, CG:167.79cm Weight: EG: 64.64kg, CG: 65.28kg |
N/A | N/A | Education in EG and CG: 80.8% = no education on PFMc 19.2% = education on PFM (from media, written instructions) Self-management strategies reported in EG and CG: 41.4% urinated before activity 30% did not do anything |
| Ferreira et al. (2014). Portugal | Quantitative (randomised controlled trial) | N = 32 volleyball athletes with UId (16 EG, 16 CG) Mean age: EG: 19.4 years, CG: 19.1 years BMIe: EG: 22.8, CG: 21.5 Duration of UI: EG: 2.4, CG: 1.6 Years of sport practice: EG: 6.9, CG: 4.9 Number of weekly trainings: EG: 3.6, CG: 4.8 |
PFM education and PFM exercises vs CG (education pamphlet-only) CG: Education pamphlet included information on PFM anatomy, UI, aetiology of SUI, prevention strategies for UI and PFM exercises. EG: Education pamphlet as above PFM exercises included 30 PFM sustained contractions (no duration noted), 4 PFM quick contractions after each sustained contraction, once per day for three months Weekly club visit to ensure adherence to PFM training program Urinary diary to track urine leakage |
Bladder diary Questionnaire Pad test | End of training intervention: Reduced urinary leakage by 45.5% (EG), 4.9% (CG) Reduced frequency of urinary leakage episodes to 1.8 episodes per 7 days (EG), 1.9 episodes per 7 days (CG) |
a: control group; b: experimental group; c: pelvic floor muscle; d: urinary incontinence; e: body mass index
Of relevance clinically, it was identified that PFMT is not necessarily made more effective by coupling it with biofeedback.26
Dockter and associates8 found that 80.8% of their study’s participants were not aware of the role of PFMs. Furthermore, Ferreira and colleages29 determined that education in conjunction with PFMT was more beneficial in preventing and managing incontinence in female athletes than education alone. Education was provided to both the control and experimental groups via information pamphlets on pelvic floor muscle anatomy and physiology, UI aetiology, strategies to prevent urinary leakage, as well as instructions on how to contract the pelvic floor muscles.29 Urinary diaries were implemented in the experimental group to track fluid intake, and amount and frequency of urination were also employed as outcome measures in the study.29 Further, the combination of education with PFMT improved outcomes, resulting in reduced urinary leakage and frequency of urinary leakage episodes when compared to education as a stand- alone intervention.29 Conversely, education as an incontinence prevention strategy was not included in any of the military studies.
Apart from PFMT, fluid restriction or daily pad use were identified by several included studies as key self- management strategies for both UI and AI symptoms used by female military personnel.25,26,27,28,30 In addition, Criner25 noted that military women frequently changed their underclothes (67%), visited bathroom facilities more often (62%), avoided exercise (17%) and avoided strenuous exercise (9%) if they suffered from UI. In comparison, self-management strategies for UI in female elite athletes identified in the survey by Dockter8 involved urination prior to participation in activity, not laughing and no intervention.
Surgical intervention (anal sphincteroplasty and perineorrhaphy) was found to resolve impacts of AI in one female soldier, 12 months post-procedure.24 This case study provided level IV evidence,31 as it was only focused on one individual, and it was also the only article focused on AI included in this systematic review. Therefore, it is difficult to determine how replicable the study’s results would be for other military women, or female elite athletes, experiencing similar AI symptoms. Furthermore, the effectiveness, safety and role of surgery for UI and POP were not determined by the findings of this review.
There was limited information regarding the safety of reported intervention strategies, but no adverse outcomes were reported by any of the included studies. Two of the included studies reported attrition data.14,26 One of these studies lost 12 participants to follow-up as they were transferred,14 while the other lost a total of seven participants due to PFM injury, mistaken diagnosis and a change to groups.26 None of the studies provided information on adherence to the prevention and management interventions investigated.
Limitations of included studies
An array of limitations were identified within the included studies. Firstly, there was only one randomised controlled trial. Therefore, prevention and management strategies for UI, AI and POP have not been widely investigated rigorously for this population, resulting in less certainty in the findings due to the potential for confounding and risk of bias in the remaining studies. Furthermore, seven of the included studies focused on UI and only one on AI, meaning that POP was not considered, and very limited evidence exists in relation to AI. Seven of the studies were conducted in the USA, suggesting that international and cultural differences in prevention and management of UI, AI and POP have not been considered in any depth. All six military studies were also focused on Army women, resulting in no available information about interventions used in other military services. Lastly, none of the studies were published recently, causing the data presented to be less relevant to contemporary military women and athletes. The lack of recent studies also limited capacity within the review to examine longitudinal trends, which might, for example, indicate changes in PFD prevention or management practices over time. Furthermore, long-term follow-up beyond 12 months was not investigated in any of the included studies. As a result, it is difficult to determine whether these interventions have ongoing or lifelong benefits in preventing and managing UI, AI and POP.
Discussion
It is clear from this review that very few studies have explored the safety and effectiveness of prevention and management strategies for UI or AI in military women and female elite athletes, and none have explored strategies for POP in these populations. Nevertheless, from the included studies, it is clear that PFMT is an effective strategy in the prevention and management of UI. However, there is limited evidence to indicate it is safe. Despite few high-quality clinical trials of interventions for UI in the female military population, this finding is consistent with current recommendations for the general population that PFMT is safe and should be the first treatment option for women experiencing UI symptoms.32 Although the studies included in the review presented specific PFMT programs, optimal dosage and practice of PFMT are unclear, with variability in the application between studies and individuals.33 Further research is warranted to ascertain how these strategies can be optimally implemented in the broader female military and elite athlete populations. Additionally, the combination of PFMT with an education program gave positive results in reducing UI symptoms in the female athlete population, so investigation into how military women may also benefit from the addition of such an education program is necessary. Yet, it is unclear from this systematic review whether PFMT and education as a combined intervention were more effective than PFMT alone.
From the included studies, it is evident that women from these populations use various self- management strategies to manage UI symptoms— these include PFMT and, concerningly, fluid restriction and daily pad use. Strategies such as these may aid in reducing the number of accidents and avoid the negative consequences associated with accidents such as needing to change underclothes and embarrassment.34 However, strategies such as fluid restriction and daily pad use do not address the underlying contributing factors to UI and may compromise the women’s health in the long term. Fluid restriction as a UI management strategy during military fieldwork is potentially dangerous to the health of female military personnel due to the risk of dehydration and heat stress.13 Further to this, daily pad use may be effective in the short term but may be unsafe long term. As pads can be in limited supply during deployment, duration of use may be longer, and alternative items such as toilet paper or paper towels are sometimes used.35 Using these as alternatives may not be as effective as the use of pads in managing UI and may increase the risk of skin irritation.34 Further to this, decreased access to handwashing, showering and laundry facilities and resources in deployed military environments, and decreased sanitation may increase the risk of infections.35
A range of alternative prevention and management interventions for UI, AI and POP, commonly used clinically, have been investigated in the general female population. These include mechanical devices such as pessaries and various surgical procedures. Pessaries are effective in 60% of POP cases in the general female population.36 However, women affected by POP over the age of 55 in the general population were found to experience more adverse effects such as discomfort with pessary use than PFMT, despite pessaries being more cost-effective.37 Female military personnel rarely use pessaries,15 as being an internal device, barriers may arise relating to decreased hygiene and sanitation in deployed environments.35
Various surgical procedures are also used to treat UI, AI and POP. The type of surgery selected often depends on the severity of the patient’s symptoms, the patient’s choice and general health, as well as the preference and skills of surgeons.38 Surgical effectiveness for POP in the general female population varies between studies (19.2–57.6%), with treatment success usually based on anatomic support noted.39 Encouragingly, from a patient perspective, 71% consider their surgery to have been ‘very successful’.39 Despite there being multiple approaches and types of surgery for these conditions, women in the general population report higher satisfaction levels with surgical intervention than non-surgical options such as PFMT and pessaries.40 Furthermore, surgery repeat rates vary between 6–28% for women in the general population.41-42 Adverse outcomes of these surgical procedures include urinary retention, dyspareunia and, if used, mesh exposure.42 In female military and female athlete populations, there have been no studies comparing surgical outcomes with conservative management strategies such as PFMT. Further research is essential to determine the safety, viability, cost-effectiveness and occupational impacts of a broader range of interventions for the prevention and management of UI, AI and POP in female military and athlete populations.
The findings of this systematic review provide valuable knowledge for health professionals, military women and female athletes experiencing UI and AI symptoms as well as for researchers investigating UI, AI or POP. Additionally, this review provides insight into how military women and female athletes prevent and manage UI symptoms. The results of this review may also provide useful guidance for military health services seeking to develop recommendations and clinical guidelines that would inform healthcare facilities regarding UI and AI prevention and management. Ultimately, military women and female elite athletes experiencing UI may benefit from implementing evidence-based treatment options discussed in this review, which may facilitate improved health outcomes.
Suggestions for future research
As discussed, further research into the prescription of PFMT and the role of PFM education is needed in the female military population for UI, AI and POP prevention and management. In addition, it would be beneficial for research to compare strategies regarding their outcomes and safety. Furthermore, research is warranted into how female military personnel can be better supported with their pelvic floor health in deployed environments. This may involve how the additional provision of sanitary items may improve PFD symptoms or how implementing predeployment education programs regarding PFD, pelvic floor anatomy and PFMT benefits these women. This review largely focused on UI, as studies focused on AI and POP were limited or unavailable. On this basis, additional quantitative research into military women and female elite athletes experiencing other types of PFD, such as AI and POP, as well as interventions to prevent and manage these conditions, is also required. As a result, military women and female elite athletes would benefit due to additional evidence and advice on how to reduce the impacts of UI, AI and POP. Research investigating alterations in occupational or training loads post-surgery for military women and female elite athletes may also be warranted to determine surgery repeat rates and factors affecting optimal recovery. Resultingly, the pelvic floor health of military women and female athletes would benefit.
Review strengths and limitations
This was the first systematic review investigating prevention and management strategies for UI, AI and POP in both military women and elite athletes. Strengths of this systematic review included clear inclusion and exclusion criteria with clearly stated aims. It used a broad-based, systematic approach in deciding study eligibility. An array of databases was searched, ultimately increasing the likelihood of identifying relevant articles. The methodological quality of the included articles was systematically appraised, and the review implemented a systematic approach to data extraction and synthesis. These standardised and systematic approaches reduce the risk of bias in the review. Overall, the systematic review provides a clinically-relevant summary of the findings of published studies on the prevention and management of UI in military women and athletes, while identifying existing research gaps on this topic and AI and POP.
However, it should also be noted that this systematic review is limited by the small number of available studies for inclusion. Despite the breadth of the search strategy, it remains possible that some studies may have been missed. In particular, studies published in languages other than English were excluded, and this may have also resulted in missing relevant articles. Similarly, studies published prior to 1994 were excluded. Finally, studies indexed in databases other than those searched or published in less-indexed journals may not have been located by this review.
Conclusion
This systematic review has demonstrated that few published studies have investigated strategies used to prevent or manage UI, AI and POP in military women and female athletes. PFMT was found to be the most common intervention implemented for UI prevention and management in military women and female elite athletes. Education regarding PFMT and relevant pelvic anatomy was also found to be beneficial in female elite athletes. Both of these interventions were found to be safe and improve symptoms. In comparison, other self-management strategies concerningly used by military women, such as fluid restriction and daily pad use, may reduce UI symptoms in the short term but may place the health of female military personnel at risk due to dehydration, heat stress and skin irritation. Further research is required in this area but currently, PFMT and likely also education programs will aid in the prevention and management of UI in military women and female elite athletes. Military women should apply caution in relation to the daily use of pads and fluid restriction as self-management strategies for UI due to potential for adverse health consequences.
Corresponding Author: Catrin Garrington, catringarrington@gmail.com
Authors: C Garrington1, S O’Shea2, R Pope2
Author Affiliations:
1 Charles Sturt University
2 Charles Sturt University Albury-Wodonga Campus – School of Allied Health, Exercise and Sports Sciences



