Abstract
Background: Spinal cord injuries (SCIs) demand particular attention; people with SCI report reduced quality of life and impairments in everyday life. We tested whether and to what extent neurofeedback or a physical activity training could, compared to a control condition, improve reaction time and balance as proxies for fine motor control in a sample of Iranian veterans with SCI.
Methods: A total of 30 Iranian veterans with SCI were randomly assigned to the following study conditions: neurofeedback, physical training, or a control condition (conventional therapy). Both at the beginning and four weeks later, reaction times and balance were objectively measured.
Results: Compared to the control condition and over time, reaction times improved in the neurofeedback condition, while balance improved in the physical training condition.
Conclusions: Compared to a conventional treatment condition, neurofeedback and physical training improved skills in specific areas of motor control. Thus, it appears that both neurofeedback and physical training should be introduced as routine interventions for patients with SCIs.
Key words: rehabilitation, reaction time, balance, physical training, neurofeedback, spinal cord injuries
Introduction
Spinal cord injuries (SCIs) are considered a serious health problem. 1 Typically, adults with SCIs suffer from disorders of the cardiovascular and respiratory systems, along with chronic pain; they also report reduced quality of life. Thus, SCIs are associated with considerable reductions in functional status, including poor motor performance, and extensive psychological issues such as severe negative emotion and low self-esteem as well as increased needs for medical and paramedical support. 2 Prevalence rates have been estimated at between 50 to 1 298 cases per million worldwide; the range varies considerably across occupations. 3 For example, the risk of injury involving SCIs is particularly high among construction industry workers (26%), transportation and retail workers (15% respectively), manufacturing workers (13%), and agriculture and utility workers (11% respectively), whereas some other occupations have a low risk of such injury. 3 Additionally, and not surprisingly, prevalence rates for SCIs are high among soldiers, and this holds particularly true for those soldiers serving under wartime conditions. As regards the situation for Iranian veterans of the first Gulf War, it is estimated that up to 2 000 veterans are still suffering from such injuries. 4
Treatment options for SCIs include physical therapy, occupational therapy and rehabilitation psychology, along with various forms of medication. The latter are widely employed to treat pain and muscular spasms, though they also have side effects. 1 In the present study, we focused on physical training (PT) and neurofeedback.
PT is one of the best non-pharmaceutical methods of treatment for SCI,2 and there is extensive evidence that PT is a crucial contributor to the overall wellbeing of those with disabilities,5,6 with a positive effect on motor functions. 7 PT consists of exercising at progressively increased intensity and speed to avoid sudden pressure drops. In this study, we employed vestibular exercises as recommended by Cawthorne and Cooksey. 8 These authors claim that such exercises can serve as support for new arrangements of peripheral sensory information, allowing new vestibular stimulation patterns necessary for new motor skills to become automatic. These exercises are part of a vestibular rehabilitation program and involve head, neck and eye movements and posture control exercises in different positions, use of soft surfaces to reduce proprioceptive input, and exercises with eyes closed to exclude visual cues. 8
While PT is well established as a treatment for SCIs, more recently neurofeedback (NF) and neurofeedback training (NFT) have attracted increased interest. For instance, NF and NFT have been employed to treat pain, as the feedback via the neurofeedback device serves to reinforce neuronal activities associated with specific brain activities. 9 Within the field of NFT, a 12- to 15-Hz oscillation of the sensorimotor cortex has proved to be a promising link between adaptive mental states (e.g. automatic process-related attention) and skilled visuomotor performance(14). A 12- to 15-Hz oscillation of the sensorimotor cortex is also referred to as SensoriMotorRhythm (SMR). There is now evidence of the positive effects of NFT in adults with chronic pain,10 attention-deficit/hyperactivity disorder,11 and fibromyalgia,12 with impacts on motor performance enhancement,13,14 and cognitive flexibility. 9 Neurofeedback has also been employed in the treatment of anxiety and traumatic brain injury, and in the recovery of patients with impaired motor performance. 9 Additionally, NFT has the potential to replace aspects of physical exercise, particularly among people with disabilities13,14 and thus for whom regular participation in physical exercises could be rather difficult, while improving health-related problems associated with a sedentary lifestyle.
To summarise, both PT and NFT have the potential to improve motor control among people with SCIs; however, previous scientific efforts have focused primarily on pain relief. In this respect, it is important to emphasise that NFT does not have a negative impact on motor performance,15 fatigue,12 or spinal cord lesions. 16,10
Previous studies of the treatment of SCIs have considered variables such as walking speed and distance on a treadmill, over-ground walking speed (OGWS) and lower extremity motor scores (LEMS). 17 In contrast, important variables such as balance and reaction time have so far not been assessed. More specifically, and to the best of our knowledge, no study has directly examined the influence of NFT on reaction time or balance among SCI patients. Nor has the possible influence of NFT on reaction time and balancing been compared to that of PT. Accordingly, the aim of the present study was to assess whether and to what extent either NFT or PT might have on reaction time and balance, and whether these different interventions might have the same positive effects.
The following two hypotheses and one research question were formulated. First, following others,7,13,9,6 we expected that, compared to a control condition, both NFT and PT would impact positively on reaction times. Second, we expected that, compared to a control condition, both NFT and PT would improve balance. 18,8 Whether, compared to PT, NFT produces better results with respect to reaction time and balancing or vice versa were treated as exploratory research questions. We believe that answers to these questions might help both caregivers and patients with SCI improve the latter’s motor skills, which in turn could have positive effects on quality of life.
Materials and methods
PROCEDURE
Iranian male veterans with SCI were recruited for the present randomised clinical trial. Participants were fully informed about the aims and the procedure of the study, and the anonymous data handling. They all signed written informed consent. At baseline, reaction time and balancing skills were tested. Next, participants were randomly assigned to one of the following conditions: neurofeedback training (NFT), physical training (PT), control condition (CC). The intervention lasted four weeks. At the first, second and third weeks and conclusion of the study, participants’ reaction time and balancing skills were again tested. The Review Board of the Urmia University (Urmia, Iran) approved the study, which was conducted in accordance with the rules laid down in the Declaration of Helsinki and its later amendments.
SAMPLE
At total of 30 Iranian low paraplegia veterans (SCI at L3, L4 (ASIA B – D) took part in the study. Mean age was 51.5 years (SD = 3.87), and mean weight was 82.0kg (SD = 8.94). Inclusion criteria were: 1) Iranian male veteran; 2) age between 48 and 60 years; 3) spinal cord injury and grade ≥3 of sensation according to the International Standards for Neurological Classification of SCI; 4) right handed (assessed by the Edinburgh Handedness Inventory; 5) signed written informed consent. Exclusion criteria were: 1) psychiatric issues, as ascertained by a brief psychiatric interview; 2) intake of mood- and alertness-altering medications or substances.
POWER ANALYSIS
Power analysis was performed with G*Power® 3.1.9.3.(19). A minimum sample size of nine participants is required to detect a mean difference of 2.0, standard deviation of 2.0, 90% power and 5% type I error, between baseline and the study end. Furthermore, Julious20 has suggested that samples of 10–12 participants should be sufficient to run interventional pilot studies.
RANDOMISATION
Randomisation was achieved using computerised software: www.randomizer.org®.
INSTRUMENTS
The ProComp Infiniti (2180 Belgrave Avenue, Montreal, QC H4A 2L8 Canada) encoder is an eight channel and BioGraph software was used. The encoder has eight protected pin sensor inputs with two channels sampled at 2048 s/s and six channels sampled at 256 s/s. The ProComp Infiniti encoder is able to render a wide and comprehensive range of objective physiological signs used in clinical observation and biofeedback. BioGraph software reorganised functionality.
REACTION TIME
The Nelson reaction time test21 was used to measure the reaction speed of hands. The Nelson’s test consists of stopping a rod-shaped timer upon a command. At the starting position, the palms are on the table 30 cm apart and upon the command ‘ready’ the subject claps hands, gliding them on the table, then stops the timer. This activity is repeated 20 times; the five lowest and five highest results are disregarded. The reliability coefficient was found to be 0.75.
BALANCING
The Berg Balance Scale (BBS)22 is used to assess balance by direct observation. The scale requires
10 to 20 minutes to complete and measure the patient’s ability to either maintain balance statically or while performing various functional movements over a specified time. This instrument has excellent reliability (0.96) and objectivity (0.98).
INTERVENTIONS
Neurofeedback training (NFT):
The NFT involved 12 sessions, with three sessions per week. Electroencephalography (EEG) was recorded at two electrode sites (C3, C4) corresponding to the International 10–20 system. All sites were initially referenced to A1 and then re-referred to linked ears offline. EEG data were collected and amplified using a ProComp Infiniti® device with BioGraph software. EEG signals were sampled at 12–15 Hz, recorded online. The electrode was placed at C3 and C4 for sensorimotoric rhythm (SMR) training with the reference placed on the right ear. The amplitude of the SMR was transformed online into graphical feedback representations including audio-feedback tone by acoustic bass (Game Boat) in the Biograph® software (installed on a laptop). In these games, three boats appear and the patient is asked to drive the middle boat and win a race against the other two. In the SMR training, the middle boat was linked to SMR and the two other boats were linked to the delta and theta waves. When the patient maintains SMR 80% of the time above the threshold of theta and beta waves and keeps the theta and beta waves for 20% of the time below the threshold, the middle boat begins to move. Each NFT session lasted 45 minutes. The target for the SMR NFT group was to increase absolute SMR amplitude over the designated threshold. Adjustment of training threshold difficulty was used progressively to enhance participants’ efficacy during NFT.
Physical training (PT):
As with the NFT condition, participants in the PT condition were trained for 12 session, each session occurring three times a week. The sessions lasted for 60 minutes. The Cawthorne and Cooksey Exercise8 was employed as the PT intervention (see also the research guide in Ribeiro and Pereira8). The Cawthorne and Cooksey Exercise consists of vestibular stimulation. Specifically, the exercises include the following elements:
Eye and head movement. While sitting down, turn the head to the left and right first slowly then faster, with eyes open; move the head up and down with eyes open.
Head and body movement. While sitting down, place something on the floor, remove it, pick it up and put it back on the ground. Shoulder rotation bending forward, and moving in front of and behind the fixed knees.
Standing exercises. Sit down and get up; sit back down and get up, sit back down and get up; sit back down and get up with eyes closed. As you get up, turn to the right; as you get up, turn to the left; throw a small ball from one hand to the other with arms raised; throw a small ball below the knees from one hand to the other, repeat this action.
Control condition (CC):
Participants in the control condition underwent conventional therapy, attending physiotherapy sessions for about 40 minutes once a week.
Statistical analysis
Two mixed two-way ANOVAs were computed with the factors Group (NFT, PT and CC), Assessment Sessions (five assessments), the Group by Assessment interaction, and with dependent variables reaction times and balance scores. Post-hoc tests were performed after Bonferroni-Holm corrections for p-values. Effect sizes for ANOVAs were indicated by partial eta-squared coefficients, while for pairwise comparisons Cohen’s ds were reported. All statistics were performed with SPSS® 22.0 (IBM Corporation, Armonk NY, USA) for Windows®.
Table 1: Descriptive overview of motor performance (Balance and reaction time), separately for groups
(Neurofeedback, Physical training, Control) and for test sessions (Pre-test, Assessments 1, 2 and 3, Post-test)
| Groups | |||
| Neurofeedback training | Physical training | Control | |
| N | 10 | 10 | 10 |
| M | (SD) | M (SD) | M (SD) |
| Balance | |||
| Pre-test | 37.88 (5.32) | 38.36 (6.01) | 37.67 (6.07) |
| Assessment 1 | 38.67 (5.17) | 41.65 (5.03) | 40.16 (5.78) |
| Assessment 2 | 39.70 (4.92) | 43.45 (4.87) | 41.04 (5.32) |
| Assessment 3 | 40.97 (4.12) | 45.17 (4.12) | 42.44 (4.91) |
| Post-test | 41.52 (4.03) | 48.39 (4.01) | 43.20 (4.05) |
| Reaction Time | |||
| Pre-test | 0.24 (0.07) | 0.24 (0.09) | 0.24 (0.09) |
| Assessment 1 | 0.21 (0.06) | 0.23 (0.07) | 0.25 (0.07) |
| Assessment 2 | 0.19 (0.04) | 0.22 (0.06) | 0.24 (0.08) |
| Assessment 3 | 0.17 (0.03) | 0.22 (0.07) | 0.24 (0.07) |
| Post-test | 0.15 (0.01) | 0.21 (0.05) | 0.24 (0.05) |
Table 2: Inferential statistical indices for motor performance with the factors Group (NFT, PT and CC), Test session and the Group by Test session interaction.
| Factors | |||
| Group | Test | Group x Test interaction | |
| F partial eta2 | F partial eta2 | F partial eta2 | |
| Balance | 67.61 0.88 (L) | 184.62 0.95(L) | 11.75 0.56 (L) |
| Reaction Time | 27.25 0.73(L) | 53.204 0.95(L) | 55.43 0.82(L) |
Notes: NFT = neurofeedback training; PT = physical training; CC = control condition; (L) = large effect sizes
Results
All descriptive and inferential statistical indices are reported in Tables 1 and 2, and are not repeated in the text.
REACTION TIME
Reaction times improved over time. Compared to the CC, patients in the NFT conditions had more rapid reaction times. The significant Time by Group interaction showed that reaction time significantly improved in the NFT and PT conditions but not in the CC. Post-hoc analyses with Bonferroni-Holm corrections for p-values showed that at the end of the study, reaction time was shortest in the NFT condition while reaction time was shorter in the PT condition than in the CC.
For single assessment points, post-hoc analyses showed that, compared to the PT and CC, the NFT condition reaction time decreased significantly after three sessions (Assessment 1), six sessions (Assessment 2), nine sessions (Assessment 3) and 12 sessions.
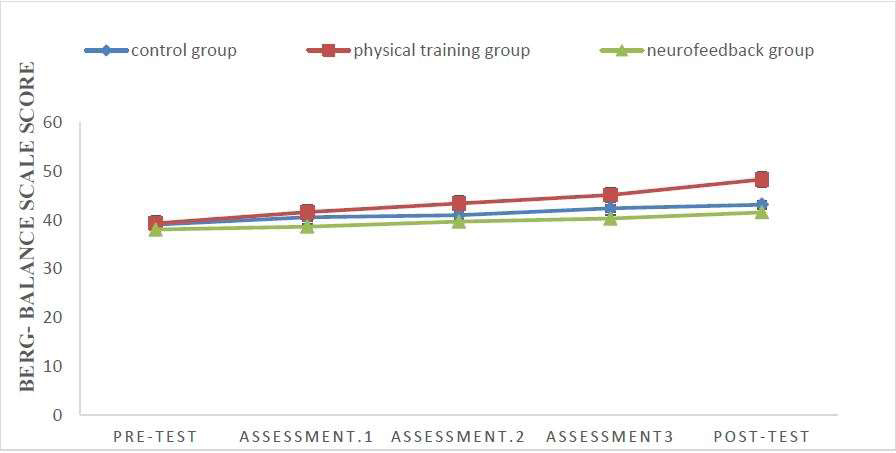
Figure 1. Reaction time decreased over time, but more so in the Neurofeedback condition than in the
Physical training or Control conditions. Points are means, and bars are standard deviations.
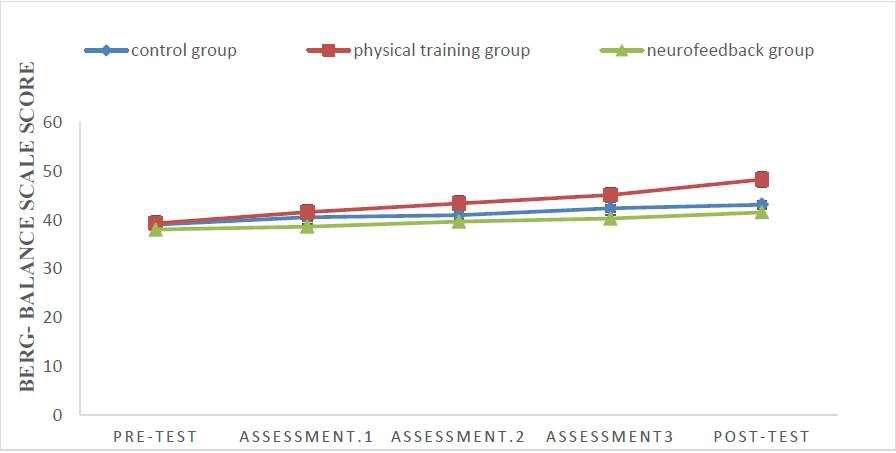
Figure 2. Balance scores increased over time, but more so in the Physical training group than in the
Neurofeedback or Control conditions. Points are means.
BALANCE
Balance scores improved over time. The significant Time by Group interaction showed that balance scores significantly improved in the PT condition but not in the NFT or CC. Post-hoc analyses with Bonferroni-Holm corrections for p-values showed that by the end of the study, balance scores were highest in the PT condition. Additionally, balance scores were higher in the CC than in the NFT condition.
For single assessment points, post-hoc analyses showed that, compared to the NFT and CC, the PT condition balance scores had increased significantly after 12 sessions.
Discussion
The key findings of the present study were that NFT and PT had differential impacts on the motor skills of veterans with SCIs. Specifically, when compared to a CC and to PT, NFT improved reaction time, but in contrast compared to the control and NFT conditions, PT improved balance. The current study adds to the literature in an important way, showing that both NFT and PT have benefits for the motor skills of people with SCIs.
Two hypotheses and one research question were formulated and each is considered in turn.
Our first hypothesis was that, compared to a CC, both NFT and PT would improve reaction times. This hypothesis was fully supported. While reaction times improved over time, they were not significantly reduced in the CC (Table 1 and 2; Figure 1). These results are consistent with those reported in several previous studies,15,23,24,25,14 but not consistent with some others. 18,14 We believe that these results add to the current literature in an important way, showing that NFT improved the motor reaction times of patients with SCIs.
While the data available from this study cannot shed any direct light on the underlying neurophysiology and neuropsychological mechanisms, we propose that the following processes may have been involved. Studies have shown that individuals with disabilities face greater physical and psychological barriers than healthy individuals do. 26 Despite the positive effects of exercise on the overall health of veterans with SCI, psychological and physical barriers prevent them from participating in health programs. 2 In addition to the motor and sensory problems of veterans with SCI, psychological problems have also been reported. 5,26 Thus, NFT offers a route to overcoming these mental and psychological barriers. 18,9 SMR is considered an indicator of cortical activation, which is inversely related to somatosensory processing. 24 On the other hand, augmenting SMR power might improve attention-related processes by improving impulse control and the ability to integrate relevant environmental stimuli. 9,14 Moreover, a facilitative sense of control and confidence can be observed following SMR NFT. 25 Thus, increased SMR implies the maintenance of a relaxed, focused state by reducing motor perception by the sensorimotor cortex;14 this corresponds with the concept of automaticity proposed by Fitts and Posner. 27 In other words, SMR NFT enables a person to accomplish motor tasks automatically. Furthermore, Doppelmayr and Weber14 found that SMR NFT not only resulted in a significant increase in SMR amplitude, but also facilitated the function of simple and choice-reaction time tasks. Furthermore, NFT indirectly reduces psychological barriers and anxiety,18,9 increases confidence, mental states of conscious attention and physical relaxation. 9 Ros and colleagues23 suggested that augmented SMR enhances the learning of a complex motor performance by developing sustained attention and a relaxed attentional focus as well as increasing working memory. One form of dysfunction following SCI is the dwindling function of the upper extremities. 2 Hand function impairment involving loss of manual dexterity and abnormal movements shows that performance of routine daily activities can be adversely affected. 28 It is believed that psychological variables have an effect on upper extremity reaction times. Therefore, consistent with the findings of the present research, NFT appears to have more effect on hand motor functioning. However, NFT had no effect on balance. This finding may be due to NFT protocols. The NFT protocol of the present study was the largest manoeuvre on the increasing of SMR frequency band, but increasing the range of the beta frequency band was not included in our study. However, the NFT protocol in the Hammond et al18 study was targeted to increase beta and reduce theta and this resulted in improved balance.
Our second hypothesis was that, compared to a CC, both NFT and PT would impact positively on balance, but again this hypothesis was not fully supported. Rather, only the PT condition produced significant improvements. This pattern of results is in line with some,8,29,2,7 but not all previous studies. 30 However, we believe that our results expand upon previous research in showing that repeated motor skill training has the potential to impact successfully and positively on the balance of patients with SCIs.
While the new data is unable to shed light on the underlying neurophysiology and neuropsychological mechanisms here, we suggest that the following processes may be involved. Numerous studies have been conducted to examine the effect of physical therapy techniques in reducing muscles tensions and improving balance and gait parameters. 29 The Cawthorne and Cooksey exercises are designed to restore balance as far as possible, and to train the eyes, muscles and joints to compensate for permanent vestibular dysfunction. 14 The Cawthorne and Cooksey exercises, which can be particularly important for SCI patients, improve balance and reduce the cycle of decline in performance. 8 PT was more effective than NFT in improving the balance of veterans with SCI. Because the control centres of the vestibular system are balanced, so PT is more effective with respect to vestibular control factors. The Cawthorne and Cooksey exercises involve training and vestibular rehabilitation via balance control centres such as vision and proprioception, through which the vestibular system operates8. On the basis of existing studies and the present findings, we can say that the Cawthorne and Cooksey training may help restore the balance of the veterans with SCIs.
The exploratory research question asked whether, compared to PT, NFT has superior effects on reaction time and balance or whether the converse is the case. This has been comprehensively answered above
Despite the novelty of the findings, the following limitations warrant against their overgeneralisation. First, the sample size was small, though we did also rely on effect sizes, which are not sensitive to sample size. Second, we only assessed male patients; accordingly, it is unclear whether the present results would also be obtained for female patients. Third, we performed no long-term follow-up; accordingly, it would have been interesting to know whether the observed benefits of the interventions were retained over time. Pulling these points together, future studies should assess larger samples, including both male and female patients and, most importantly, follow them up to establish the longer-term effects of the interventions.
Conclusions
As the results indicate, NFT had greater influence than PT on the upper extremity functioning of veterans with SCI. Conversely, PT had a greater influence than NFT on balance. Therefore, it isrecommended that NFT is used for veterans’ upper extremity reaction times and PT is used for veterans’ recovery of balance following SCIs.
Conflicts of interest
The authors certify that there is no conflict of interest with any financial organisation regarding the material discussed in the manuscript



