Abstract
Although historically greatly feared due to its ability to kill quickly from dehydration, cholera has not featured in recent ADF military operations except in 2010 when United Nations Peacekeepers from Nepal were linked to the introduction of cholera into post- earthquake Haiti. The collapse of field sanitation during the building of the Thai–Burma railway by Allied Prisoners of War (POW) led to multiple lethal cholera epidemics in 1943. Despite half of affected POW dying of cholera, the case rates were only about 10% of those exposed; the disease appeared to spare officers, Dutch soldiers and those recently immunised with killed, whole-cell vaccines. Factors that may also have played a role in the POW camps include malnutrition-induced hypochlorhydria, ABO blood type and lack of oral rehydration therapy knowledge. Oral cholera vaccine might be considered for use in the ADF during tropical operations, including disaster relief efforts in populations with active cholera epidemics.
And my memory of the cholera epidemic was not just the cholera, was the incessant Last Post… they used to burn the corpses and then there were the burials of the non-cholera.
CAPT Hugh de Wardener RAMC, 198 Field Ambulance1
Cholera is a toxigenic disease caused by gastrointestinal infection with Vibro cholerae that can rapidly kill adults from massive dehydration and electrolyte loss. It currently occurs mainly in Africa or tropical Asia, although cholera has invaded Europe and the Americas during pandemics over the last two centuries. Cholera is rare in societies with functional water and sewage systems, such that it is usually seen in the context of refugee camps (Goma in Democratic Republic of Congo, 1994) or conflict with great population displacement (Bangladesh War of Independence, 1971; Yemen 2016–2020). During the colonial period in India, cholera could destroy British Army units, as occurred in 1846 when a quarter of the 86th Regiment died at Kurrachee.2 Injected whole-cell, killed cholera vaccines were developed early in the twentieth century for use during mass religious pilgrimages in India and were credited with high levels of protective effectiveness despite predating the era of randomised clinical trials.3 Such vaccines became standard for troops deploying into the tropics although the protection period was thought to be measured in weeks/ months, not years.
The Australian Army largely avoided cholera during World War I, although its first specialised infectious disease unit was formed in 1916 in the Sinai desert to address a cholera epidemic in Egyptian drivers of the camel train.4 Cholera was a major threat to military formations only when field sanitation systems completely broke down during a war. This occurred during the terrible experience of the 8th Division Australian Imperial Force (AIF) and other Allied units during their experience as Prisoners of War (POW) of the Imperial Japanese Army, especially in 1942–44 during the building of the Thai–Burma railway.1
Successive groups of POW were forced to march up the railway track from Kanchanaburi, Thailand, often overnighting in temporary camps that had been massively faecally contaminated by previous groups of POW or Asian labourers. Although the medical officers were very aware of the cholera threat, they had neither the time nor means to institute preventive measures. Inevitably given the terrible conditions and Japanese disregard for anything other than railroad construction, cholera epidemics broke out within the POW. These appeared as scattered outbreaks in POW camps along the railway, each of a few thousand men. Four separate outbreaks were documented and reported after the war in medical publications.5-8 Cholera cases (n=150–220) were about 10% of each camp’s population resulting in about a 50% case mortality rate (deaths n=53–101), often in the form of biphasic epidemics (see Figure 1). Treatment had to be instituted under harrowing conditions during the middle of the monsoon season, often in forced isolation from the main camp. Some intravenous rehydration was possible with improvised means (bamboo cannulas) and crude solutions (rock salt in filtered river water), but the worst-affected POW were dead within hours of symptom onset.9-11 It was noticed that despite what must have been nearly universal exposure, Dutch soldiers, officers and medical personnel only rarely developed symptomatic cholera.
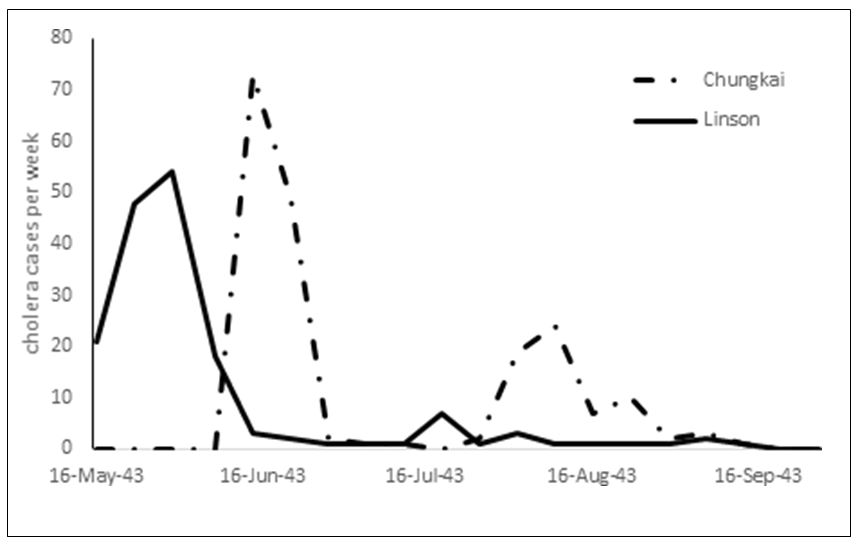
Figure 1: Two cholera epidemics in 1943 Allied Prisoner of War camps along the Thai–Burma railway were described after the war by Marcowitz (Chungkai)7 and de Wardener (Linson Camp)5 where the weekly morbidity data were extracted for this graph.
Explaining why some groups among the POW escaped cholera during an epidemic is not entirely obvious. Military medical officers on the railway credited injected cholera vaccine, which was locally prepared by the Japanese Imperial Army with high levels of protection sometimes within days of use.5,7,8 Based on our current understanding of cholera toxin and subsequent post-war vaccine studies, the cholera vaccines used in the Japanese POW camps seem unlikely to have been highly effective.12 The Dutch soldiers relative freedom from cholera compared to Australian or British POW could have been opportunistic by being in less contaminated camps or due to cumulative immunity from annual cholera vaccination after longer tropical service in the Netherlands East Indies. Officers were less nutritionally debilitated than enlisted soldiers due to not being forced to work on the railway and may explain why officers did not often succumb to cholera. Medical personnel understood infectious diseases better than other POW, but their intense exposure to sick POW would suggest that acquired immunity explained their relative freedom from cholera rather than their ability to better apply field sanitation measures.
Other aspects of cholera that were not appreciated during World War II might have partially explained the devastating but variable effect of cholera on the POW along the Thai–Burma railway. Hypochlorhydria is a known problem of starvation, particularly in pellagra and likely was very common in the vitamin- deficient POW. Hypochloridria reduces the infectious dose of Vibrio cholerae by orders of magnitude as the bacteria survive stomach acid to then infect the small bowel.13 All POW were malnourished, and those with hypochloridria would have been very vulnerable to cholera infection. Helicobacter pylori infection was not appreciated as a cause of peptic disease until decades after World War II. Large numbers of surviving POW with peptic ulcer disease make it likely that many were infected with H pylori which may have contributed to hypochloridria.14 Those with group O blood type are known to be more vulnerable to cholera toxin due to ABO blood group polymorphisms.15 Although blood grouping was done from 1944 in the POW camps in support of an extensive blood transfusion service, most cholera deaths occurred in 1943 and data allowing correlation of cholera mortality to blood groups does not apparently still exist.
Although the record is decidedly mixed, the military has constructively contributed to the post-World War II response to cholera. When located in Taiwan, the US Naval Medical Research Unit 2 discovered that cholera toxin reversed the gut’s normal salt sugar exchange mechanism to produce massive water and electrolyte loss.16 This breakthrough physiological understanding enabled the use of oral rehydration salts as the primary treatment modality for cholera and most dehydrating paediatric diarrheal diseases rather than intravenous fluids. As a result, cholera treatment today is more effective and accessible than what the POW experienced in 1943 because of oral rehydration salt solutions that directly resulted from military-sponsored medical research.
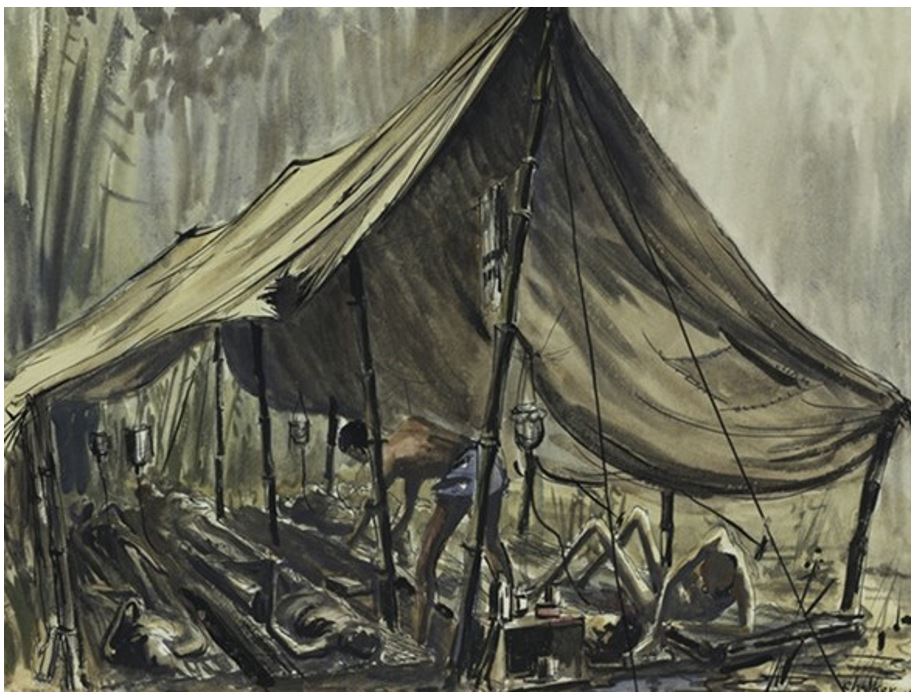
Figure 2: Australian War Memorial ART90844 Cholera tent, Hintok, Thailand along the railway built by Prisoners of War. 1943. Watercolour on paper by Jack Chalker, now deceased, used with the permission of his descendants.
A US Army water purification team in Europe was on call for airborne deployment during the mass displacement of Rwandan refugees into the Democratic Republic of the Congo in 1994. Specialist equipment (Reverse Osmosis Purification Unit) originally designed to remove nerve gas from contaminated surface water was not what was needed in the Goma refugee camps where the basic problem was a huge number of people (nearly 1 million) forced into an area of impervious ground with few water sources.17 The field sanitation problem was solved by stationing individuals at each water point to place a measured amount of bleach into all water containers, but this did not occur before the epidemic peaked at 6000 cholera cases per day and a gross mortality of 25–35/10 000 per day.
On another continent, a massive cholera epidemic in Haiti was directly traced to an introduction by United Nations (UN) Peacekeeping soldiers from Nepal coupled with a breakdown of field sanitation.18 Although military medical officers in the early twentieth century knew that oligo-symptomatic soldiers could be the source of cholera epidemics, this fact had been largely forgotten by 2010. Adequate sanitation, particularly appropriate disposal of collected sewage, could have prevented the cholera epidemic that killed thousands in Haiti. However, the newly introduced pathogen from Nepalese soldiers found fertile ground in the post-disaster Caribbean island. It is estimated that >500 000 cases and in excess of 7000 deaths resulted from this point source introduction of cholera by UN Peacekeeping forces which represents a spectacular failure of field sanitation where ordinary latrine procedures should have stopped contamination of the local river.18
Yemen has experienced the largest cholera outbreaks in recorded history. From January 2017 to December 2020, there were 2.48 million suspected cases of cholera and 3841 associated deaths (unpublished information). Ongoing multistate conflict and prolonged humanitarian crises in Yemen present serious challenges to the control of cholera. As of September 2020, some 3.34 million people were internally displaced, and 17.9 million people were in need of health assistance. In addition, military attacks have damaged water supply, sanitation, hygiene and health services.19 An integrated community-based approach that includes safe drinking water supply, improved sanitation, personal hygiene and early oral rehydration and treatment is essential to prevention and control of cholera.20
Future ADF missions will likely involve deployments into regional areas for humanitarian assistance/ disaster relief (HADR), where cholera is a potential disease risk. Epidemics have occurred in Papua New Guinea as recently as 2009 and involved more than 15 500 cases and 500 deaths over two years.21As long as the ADF can function as a military organisation with its own field sanitation facilities, the likelihood of cholera in ADF soldiers is very low but not zero. Oral cholera vaccine (Dukoral®) is available in Australia given as two oral doses separated by one week. However, it would likely only be recommended for those having direct contact with cholera-infected persons, such as medical personnel in hospitals or engineers working in refugee camps. Recognition by medical personnel of the possibility of cholera in tropical operations/HADR missions is important as readily available oral rehydration salt solutions can lower the previously terrible mortality of cholera to less than one per cent when competently used.192 Given this situation, the ADF should never have to re-live its extraordinary and heroic history of the cholera epidemics in the POW camps of the Thai– Burma railway.1
Conflicts of interest statement
The author does not claim any conflict of interest.
Funding
The author is an employee of the Australian Defence Organisation and a retired US Army medical officer but did not receive any specific funding for this study.
Corresponding Author: Dennis Shanks, Dennis.Shanks@defence.gov.au
Authors: D Shanks1,2
Author Affiliations:
1 ADF Malaria and Infectious Disease Institute
2 University of Queensland – School of Public Health






