G. D Shanks
Abstract
Measles remained a lethal infection during the early 20th century within the military but mortality disappeared prior to immunisation 50 years later. Historical records were reviewed to understand this transition. Measles mortality in soldiers was largely (>80%) due to secondary bacterial pneumonia but this could be highly seasonal, as seen in US Army recruits at Columbus Barracks 1911–13.The UK Highland Division had a lethal (65 deaths / 529 cases, 12%) measles epidemic 1914–15 but this was highly variable within different battalions. The Australian Imperial Force 1914–18 experienced 103 measles deaths (1.5% case fatality rate) half of which occurred in Australia before deployment. Measles remains highly pathogenic and absence of adult mortality cannot be guaranteed if immunisation rates are not maintained or antibiotic-resistant bacteria continues to spread. The Australian Defence Force must be prepared to deal with measles during possible humanitarian assistance missions despite anti-vaccine propaganda.
‘In our camps deaths due to noncomplicated measles were exceedingly rare; indeed,
we are not certain that there were any.’
Victor Vaughn 19221
Measles is a highly transmittable morbillivirus, which, until recently, had been considered a good candidate for global elimination as it only infects humans. Successful elimination of measles from much of the developed world has resulted in falling immunisation rates especially after the measles vaccine was incorrectly associated with autism by various anti-vaccine campaigners. The fact that measles continues to kill >100 000 children each year, largely in sub-Saharan Africa, has been ignored as measles morphs into a minor infection with a funny rash in the imagination of many uninformed adults who have never seen the disease. Measles was a major military problem in the previous century as newly recruited civilians often developed measles when gathered in large military training camps. It was a major cause of death during World War I in the Australian Imperial Force (AIF) and only faded as a military problem when globalisation markedly decreased the numbers of adults who had not been infected as children. Measles immunisation since the 1960s largely eliminated it as a public health concern except for some isolated Pacific Island populations . In the early part of the current century, about one hundred cases of measles were reported annually in Australia, usually as imported cases in those who had not been sufficiently immunised as children. Unfortunately, this public health victory is in danger of being reversed such that military medical officers need to be aware of the possibility of measles as a lethal infection. The military history of measles is reviewed to remind physicians who have never seen measles why it could be important to military preventive medicine.
Measles was a highly lethal infectious disease during the US Civil War killing 4246 Union soldiers with countless others dying within the Confederacy. Case fatality rates ranged from 6% in white soldiers to 11% in black soldiers.2 Postwar measles was mostly a problem in the recruit camps and an extended epidemic occurred from 1910–1912 within Columbus Barracks, Ohio with the continuous selection of the 1–3% largely rural recruits not yet immune to measles (See Figure 1).Measles was not remarkably lethal (5% case fatality rate overall) except during February and March when other respiratory infections were common resulting in secondary bacterial pneumonia.3 Despite heroic attempts at early detection and isolation, measles infections were nearly continuous in a camp that was progressively introducing new recruits into a larger camp population.
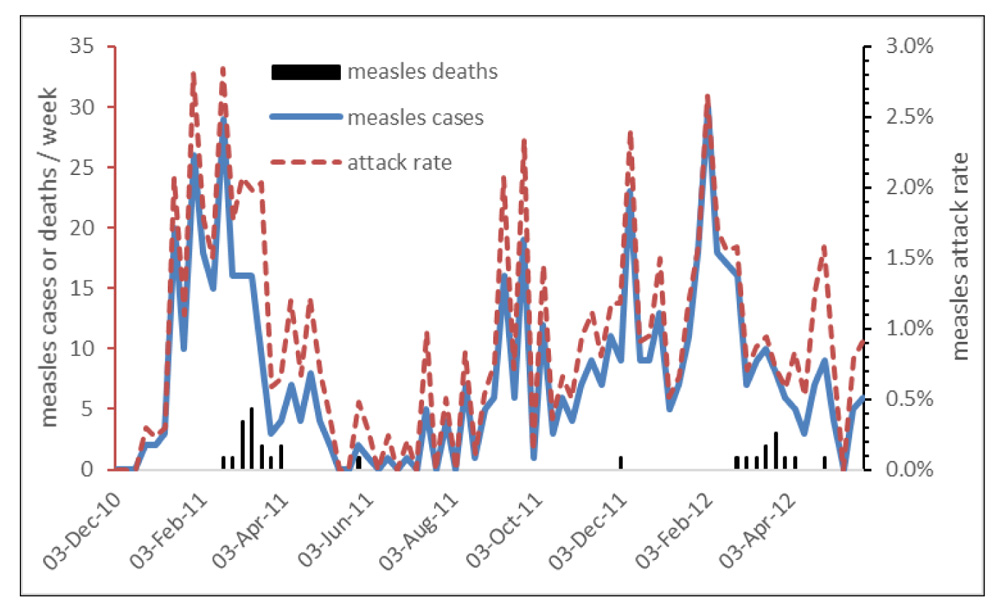
Figure 1: Measles cases, deaths and attack rates as per cent of recruit population of US Army Columbus Barracks, Ohio 1911–1913 showing the mortality was largely limited to February / March despite near-continuous chain of infection over two years.
Columbus Barracks accurately predicted the nature but not the scale of what happened during World War I when the USA suddenly recruited not hundreds but millions of men into the army. Measles was unquestionably the greatest infectious disease problem of the US Army in 1917 killing more than 3000 soldiers during the war although its impact was later obscured by the 1918 influenza pandemic.4 The measles virus attacked the respiratory epithelium but the real risk was that the compromised pulmonary defences of the immunosuppressed soldier would succumb to a secondary infection when respiratory bacteria descended into the lungs to cause pneumonia. Pneumococcus was common but the most lethal pneumonia was caused by what is now called Streptococcus pyogenes and in the preantibiotic era had a 1:3 mortality rate. Although nearly all measles susceptible recruits would be infected after joining the army, the rates of secondary bacterial pneumonia and thus death varied greatly with measles-attributed mortality ranging from 0 to 2.4 / 1000 men in 39 different recruit camps during 1917–1918.1
This was a puzzling lack of uniformity given the near-identical nature of the camps and was based on the risk not of measles, but secondary bacterial pneumonia. It proved a prescient forerunner of what was to occur during the 1918 influenza pandemic. Men who stayed in their barracks rather than crowded hospital wards or those who were triaged to different wards based on bacterial cultures of their throat had much lower bacterial pneumonia rates post-measles infection.4 When Cummings (1921) examined the differences between US soldiers developing measles in the USA as opposed to those developing measles after deployment to Europe, he found that although the attack rates were much higher in the recruit camps (29.3 USA vs 6.8 Europe / 1000 soldiers) the measles case fatality rate was much higher in Europe (2.4% USA vs 4.6% Europe).5 He concluded that the risk of secondary bacterial pneumonia was highest when a soldier with measles was exposed to a large group of ‘seasoned’ or experienced soldiers who were presumably more likely to have a wide variety of respiratory bacteria and thus available to infect the vulnerable man with measles infection. This fits well with the observation by Vaughn that begins this paper that the men died not of measles but bacterial pneumonia following the viral infection.1
Measles in the British Army of World War I was largely confined to men from rural areas typical of the Scottish Highlands who were mobilised as part of the Territorial Army. The Highland Division (51st Division) experienced a measles epidemic after it was concentrated in Bedford for training before its deployment to the Western Front (See Figure 2).6 The measles infection rates varied widely by battalions within the division and was largely determined by whether the soldiers came from urban Edinburgh or rural Dumfries. Battalions with high measles rates did not necessarily have the highest death rates. Simultaneous outbreaks of scarlet fever caused by Streptococcus pyogenes complicated the picture and added greatly to the mortality. By early 1915, 65 deaths occurred from 529 measles cases for a 12% case fatality rate that was greater than that experienced during the US Civil War.
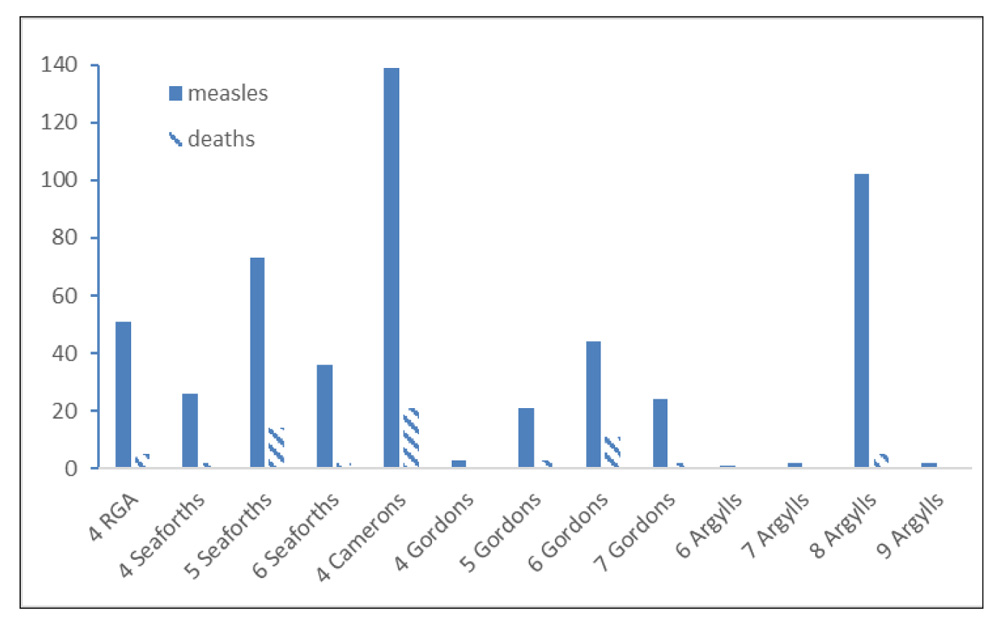
Figure 2: Measles cases and deaths in UK Highland Division units while training at Bedford, UK from September 1914 to March 1915 showing the wide range of disease and mortality in Scottish soldiers. Five additional units (not shown) had only one measles case each and six additional units had no measles. Infantry battalions labelled as shown with 4 RGA = Royal Garrison Artillery.
The USA and UK experiences were reflected on the smaller scale of the AIF, which had 6805 measles cases recorded 1915–1917 although it is likely many cases in recruit camps were under-counted. Measles resulted in 103 deaths for an overall case fatality rate of 1.5% during World War I with only five deaths being from 1918 (See Figure 3).7 Most deaths (53) occurred in Australia although measles also killed 14 in Egypt, 16 in UK and 16 in troopships at sea.8 Considering the largely rural population of Australia in the early 20th century, this was not greatly different from the experience of its USA and UK allies who had larger but more varied populations.
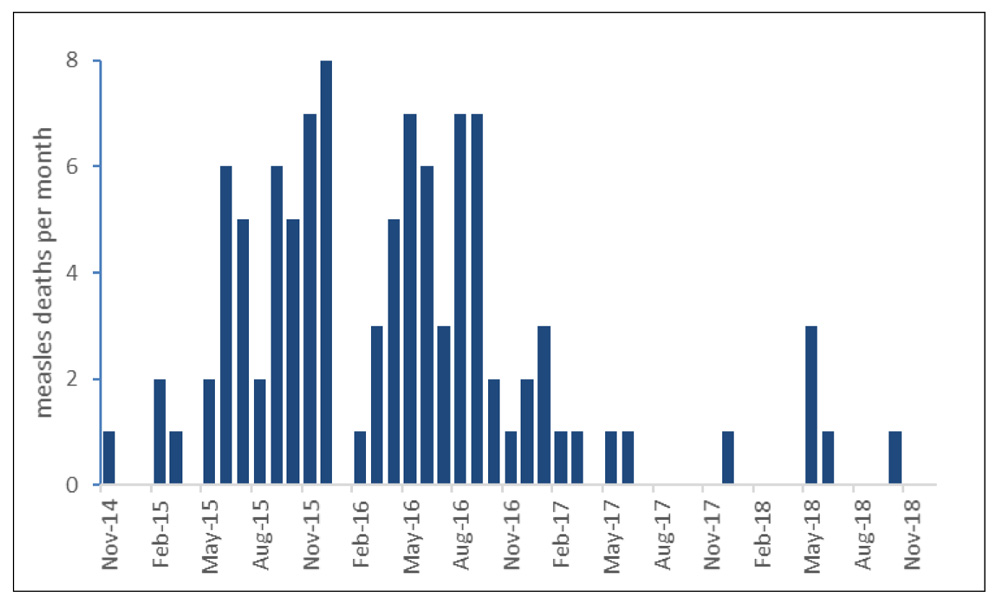
Figure 3: Measles mortality in soldiers of the Australian Imperial Force 1914–1918 of which 53/103 occurred in Australia before deployment during World War I.
Measles ceased to be a military problem prior to the introduction of measles vaccine in the later part of the 20th century as increased population mixing meant that measles infections occurred in children long before they reached military age. Recruit camp and troopship epidemics occurred in Australia during World War II but there were no recorded deaths due to measles. The safe and highly effective measles vaccine introduced from the 1960s seemed to end the need to consider measles in the military other than to ascertain a soldier’s immunisation status on recruitment. Measles, however, was not eliminated globally and retained its pathogenic potential. In 1996, measles immunisation was imperfect in Greece and this produced a large epidemic (1400, 15% attack rate) within the Greek Army.9 More than 30% (434) required hospitalisation; many had pneumonia most of which were due to bacteria such as Streptococcus pneumoniae, Klebsiella pneumoniae or Staphylococcus aureus. Although there were no deaths, six soldiers were admitted to an intensive care unit and in an earlier generation likely would have died without such support. Both the USA and UK militaries currently report only scattered cases of measles usually restricted to dependant family members whereas mumps is a growing problem reflecting further gaps in public health immunisation programs.
Military missions are evolving such that humanitarian assistance/disaster relief interventions are becoming more common. Measles is a known killer in refugee camps set up in the wake of such disasters, sometimes remarkably so; during the Boer War half of the children put into refugee camps did not survive (nearly 30 000 total deaths, 29% mortality overall) largely due to measles and pneumonia.10 Measles immunisation campaigns are one of the first public health interventions recommended in most complex public health emergencies to cover populations, which are often already nutritionally compromised with little previous health care access. A high level of clinical acumen is required when looking for an unfamiliar infection in a stressed population that has potentially been exposed to many other infectious agents. Measles should remain on the differential diagnosis of febrile individuals in the tropics even without a distinctive rash as it remains potentially lethal with an outstanding public health response of effective immunisation. Degrading our technological edge against measles by accepting pseudoscientific arguments against modernity must be vigorously avoided. Anti-vaccine campaigners have to be seen in the same category as other belief systems that seek to nullify our known advantages against likely political and disease threats.
Contributors: GDS is responsible for the entire manuscript.
Conflicts of interest statement: The author does not claim any conflict of interest.
Funding: The author is an employee of the Australian Defence Organisation and a retired US Army medical officer but did not receive any specific funding for this study.
Acknowledgements: The author thanks the many un-named historians, medical librarians and archivists who have unselfishly provided references, data and ideas for this publication.
Disclaimer: The opinions expressed are those of the author and do not necessarily reflect those of the Australian Defence Force or the US Department of Defense.
Corresponding author: G. Dennis Shanks dennis.shanks@defence.gov.au
Authors: G. Dennis Shanks 1,2
Author Affiliations:
1 ADF Malaria and Infectious Disease Institute
2 University of Queensland, School of Public Health