G. C. Rose,1 N. Westphalen,2 G. D. Shanks3
Abstract:
Four sailors aboard HMAS Newcastle were infected with falciparum malaria during a port visit to Dar-es-Salaam in Tanzania. All four were successfully treated at sea with oral atovaquone/proguanil. Besides their apparent non-adherence with the usual antimalarial precautions, the key aspects of this outbreak include a lack of on-board definitive diagnostic capability and treatment, both of which have since been addressed for other Fleet units. Although some Royal Australian Navy (RAN) deployments have lower malaria risk, this is not true for East Africa. All Australian Defence Force (ADF) medical officers need to be aware of falciparum malaria, as one of the few infections that can rapidly kill adults.
Key words: malaria, falciparum, Royal Australian Navy, Indian Ocean
Introduction:
Febrile persons returning from Africa have a very long list of differential diagnoses including common (e.g. influenza) and uncommon (e.g. Yellow Fever) viral, rickettsial (e.g. African tick typhus), bacterial (e.g. typhoid fever) and parasitic (e.g. falciparum malaria) infections. Although all of the examples listed are potentially lethal, falciparum malaria is the only common infection that can rapidly (1-3 days) kill non-immune travellers such as military personnel.
For this reason, early consideration should always be given to malaria in the management of any febrile patient from a malaria endemic area. Although many of the more recent Australian Defence Force (ADF) overseas deployments ashore have been to areas with no (Iraq) or limited (Afghanistan) malaria risk, the risk varies far more widely in the Australasian region from very low in Vanuatu to very high on the north coast of Papua New Guinea (PNG). Furthermore, most ADF malaria cases ashore in recent years have been caused by relapsing (Plasmodium vivax) malaria weeks to months after they return to Australia, rather than the more lethal and acute onset Plasmodium falciparum.1
The risks associated with maritime operations in malarious areas depend on the type of operation being undertaken. The Royal Australian Navy (RAN) often conducts extended littoral maritime operations very close inshore (within mosquito range, typically less than 1-2 nautical miles). Examples include RAN personnel conducting hydrographic surveys off northern PNG, and clearance divers conducting explosive ordnance disposal tasks in Bougainville and the Solomon Islands (although the latter tend to be shore, rather than sea-based).
Ships conducting offshore maritime operations are only exposed to malaria risk during port visits in malarious areas which are typically of short duration (four days or less), and usually involve ports where the risk is low. Although ships undertaking these visits require the same antimalarial precautions as for extended littoral operations close inshore, they are usually only required for the duration of each visit, rather than the whole deployment. All personnel undertaking maritime deployments are briefed on the relevant health hazards in accordance with Australian Fleet standard operations, usually with additional deployment-specific guidance and reinforced by port-specific health briefs prior to each visit.
RAN units undertaking Operation MANITOU conduct counter-piracy and interception of narcotic-running dhows along the eastern coast of Africa. When not engaged in operations, these Fleet units will visit a variety of ports, most of which have no or minimal malaria risk. (Figure 1) See Malaria Atlas Project (https://www.map.ox.ac.uk/) for global malaria estimates. However, malaria chemoprophylaxis is required for port visits to endemic malarial countries on the East African coast. Although preventive measures sometimes fail, most ADF malaria cases result from individual non-adherence. Four such failures recently occurred aboard HMAS Newcastle following a port visit to Dar-es-Salaam, Tanzania. (Figure 2) This highly unusual event highlighted several issues for future ADF deployments.
Figure 1: Approximate Zone of Operations for OP MANITOU
Outbreak Description:
During 10-14 June 2015, four sailors presented to HMAS Newcastle’s sick bay with fever, malaise, dehydration, nausea, headaches and fatigue over some days. They were given symptomatic treatment for fever, excused duties and sent to rest in their mess. All four members had returned from shore leave at the same hotel during a port visit to Dar-es-Salaam, Tanzania 26-29 May 2015, where they had extensive outdoor night time exposure to mosquitoes. Despite all crew members receiving warnings that malaria was endemic in Dar-es-Salaam and advice provided regarding appropriate long sleeve clothing to be worn during dawn and dusk, sleeping under mosquito nets if sleeping outside, use the supplied mosquito repellent and direction to take malaria chemoprophylaxis (doxycycline), no precautions were taken to reduce the risk of malaria by the sailors involved.2
On 15 June 2015 the medical officer HMAS Newcastle contacted the Australian Army Malaria Institute (AMI) at Gallipoli Barracks in Brisbane requesting advice for these sailors, who now had fevers to 40˚, dehydration, headaches, abdominal pain and vomiting. The medical officer also made contact with the Fleet Medical Officer (FMO) over the course of the day, for advice on the short to intermediate term management if evacuation was needed. Two members had become visibly jaundiced and were admitted to sickbay, where they were rehydrated with intravenous fluids, treated symptomatically with antipyretics and monitored by the medical team overnight. The rest of the crew were screened for symptoms and no other cases were found.
Although malaria rapid diagnostic tests are available for a ship deploying to malarious areas, they are not considered critical items, nor are they listed as accountable items on the medical allowance
Figure 2: HMAS Newcastle, an Adelaide class frigate, while at sea. (ADF photo)

list (MAL) and so were not routinely carried out and thus not ordered prior to departing Australia. Furthermore, although the on-board chemical analyser (iStat™) was considered a critical item, the cartridges that allowed for rapid laboratory testing were not obtained in Australia prior to departure as they were also not deemed critical.
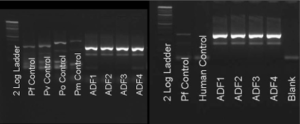
On 16 June 2015 blood was taken pre-treatment for later diagnostic testing, and all four cases were commenced on oral atovaquone/proguanil, Malarone® (1000 mg/400 mg) daily; the only one of the three antimalarial drugs on board (others were primaquine and doxycycline) that could be used to treat falciparum malaria. Although by then all four cases were jaundiced, they had significantly improved by the second day of treatment, beginning to eat again, feeling less dehydrated and their headaches settling. By treatment day three they were clearly improving and they were afebrile by treatment day four. Three of the four cases returned to normal duties by treatment day seven and the fourth returned to duty on treatment day eight. Following advice from AMI, a two week course of primaquine was commenced on treatment day two (16 June 2015), in order to eliminate the risk of relapsing malaria. At the next port visit on treatment day eleven (26 June 2015) malaria rapid diagnostic tests and additional malaria treatment medication (artemether/lumefantrine, Coartem®) were obtained by special courier delivery. Blood taken at the time of illness was positive for falciparum malaria by rapid diagnostic test.(SD BIOLINE™ Malaria Ag P.f/Pan) (Figure 3) Definitive confirmation of the diagnosis of acute falciparum malaria was obtained by polymerase chain reaction of residual nucleic acid at AMI. (Figure 4)
Issues related to malaria rapid diagnostic tests, and treatment medications were raised at the FHD
Figure 3. Rapid diagnostic tests showing that the four sailors were infected with Plasmodium falciparum. Test is SD BIOLINE Malaria Ag P.f/Pan.
Found in the download
Medical Allowance List Working Group (MALWG) on 13 July 15. All MALWG recommendations are reviewed by the FMO and approved by Director, Navy Health (DNH) and compiled for a quarterly published update to the Fleet. In this case, the MALWG agreed to update the MAL to reflect current ADF guidance, by adding artemether/lumefantrine, Coartem®.2 Although this guidance is not publicly accessible through the ADF intranet, the treatments recommended approximate current malaria treatment guidelines from the World Health Organization (https://www.who.int/malaria/publications/atoz/9789241549127/en/).
Discussion
Falciparum malaria has an approximately 48-hour cycle, with a ten-fold multiplication each cycle.3 One can therefore estimate that these sailors were 1-2 days from requiring urgent medical evacuation and 3-4 days from death if not treated. Antimalarial precautions such as mosquito netting, long clothing, insect repellent and chemoprophylaxis must all be employed in order to be effective. Non-adherence is partially due to perceptions of invulnerability common among young men, as well as uninformed reading of internet reports describing an infinite number of adverse events following some antimalarial chemoprophylaxis regimens (typically mefloquine). Practical experiences such as this event, if communicated properly to ADF members, may facilitate better adherence with antimalarial precautions in the future. Even so, this event is considered highly unusual, noting there have not been any known cases of malaria among Navy personnel undertaking seagoing operations (as opposed to those ashore) at least since the early 1960s.
Figure 4 Electrophoresis gel showing DNA bands diagnostic of falciparum malaria in all four sailors (ADF1-4 compared to Pf Control).
Although HMAS Newcastle was authorised to be supplied with malaria rapid diagnostic test kits, they were not available for use when needed and were not considered critical for this deployment. Furthermore, despite having the correct laboratory equipment to conduct limited hepatic and renal function monitoring, no consumable supplies to actually perform them were embarked. As a result, the medical officer’s ability to diagnose these four malaria cases was limited to clinical findings.
Although these issues have since been addressed, this event demonstrates some of the generic risks associated with providing health support for maritime operations that require active management, and the role of Navy medical officers with respect to managing these risks. Even so, timely evacuation remains the only option for RAN and other ADF deployments that do not have a medical officer or malaria diagnostic and treatment capability. Medical officers must take all febrile illnesses following travel to Africa seriously and arrange to rapidly rule out treatable aetiologies such as malaria. Recent failure to understand the malaria risks in Africa in other military forces has resulted in severe illness including deaths and multiple air evacuations.4,5 Although all febrile patients returned from Africa do not have malaria, it is important to quickly ascertain if any such individual has malaria, as it remains a very treatable infection if medications are given in time.
Contributors: Author GCR managed the patients while author GDS provided advice and author NW provided Navy-specific input.
Funding: GCR and NW are serving members of the Royal Australian Navy, while GDS is an employee of the Australian Defence Organisation and a retired US Army medical officer. None received any specific funding for this study.



