J Skipp, P Zimmerman, T Van de Mortel
Abstract
Background: Advances in personal protective equipment, tactical combat casualty care training and improved technologies have led to the increased survival of those injured during combat. However, infection remains a significant complication in combat-related injuries, from initial wound contamination to infections acquired in various treatment facilities.
Purpose: To determine contemporary infection prevention and control (IPC) practices used to reduce healthcare-associated infections (HAIs) in the Australian Defence Force (ADF) deployed Medical Treatment Facilities (MTFs).
Method: An integrated literature review was conducted into the IPC practices of ADF and internationally deployed MTFs.
Results: Thirteen articles were reviewed and five main themes were obtained. For effective IPC, deployed MTFs require IPC-specific standard operating procedures, strict adherence to basic IPC practices, a robust antimicrobial stewardship program and deployed personnel with the relevant expertise and knowledge in IPC.
Conclusion: Infection prevention and control in deployed MTFs comes with its own unique set of challenges. For deployed MTFs, establishing effective IPC practices and procedures will reduce the risk of HAIs and minimise the risk of further harm occurring to injured personnel.
Keywords: infection prevention, infection control, military, military hospital, field hospital
Conflict of interest: The author(s) declare no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Introduction
Healthcare-associated infections (HAIs) are difficult to prevent even in the most optimal healthcare environments.1 Mitchell and Shaban report approximately 165 000 HAIs occur per year in Australia.2 By comparison, the delivery of optimal healthcare in the deployed Medical Treatment Facilities (MTF) of the Australian Defence Force (ADF) faces many challenges.3 These include the complex requirements of the supported force, austere or hostile environments, lack of health personnel and limited logistical support.3 Advances in personal protective equipment (PPE), tactical combat casualty care training and improved technologies have led to the increased survival of those injured during combat.4,5 However, infection remains a significant complication in combat-related injuries, from initial wound contamination to infections acquired in various treatment facilities.6,7
In the field, wounds are initially contaminated with environmental exogenous flora including Clostridium sp., Bacillus cereus, B. subtilis, Pseudomonas aeruginosa and P. stutzeri as well as dust, clothing debris and other foreign materials that are driven into the wounds by explosions.6,8 Fungal species such as Mucor sp., Aspergillus sp. and Fusarium sp., commonly found in the soil in agricultural settings, have also been found to contaminate the wounds of soldiers from the United Kingdom (UK) and United States (US).9 Within deployed MTFs, HAIs are caused by multidrug-resistant organisms (MDROs) such as P. aeruginosa, Acinetobacter baumannii-calcaoceticus complex, Enterobacteriales, Staphylococcus aureus, enterococci or yeast.4,6,7 These infections are nosocomial and likely to have been spread from multiple sources within the area of operations, more specifically in healthcare settings.
If the MTF has been deployed in order to provide support humanitarian operations, initially wound infections will be seen due to trauma usually within 0–4 days. During the post impact phase (0–4 weeks) the MTF is likely to see an increase in airborne, food-borne and waterborne infections.10 It is also likely the MTF will see infections caused by Staphylococcus aureus, group A streptococci, norovirus and adenovirus. Droplet spread infections include influenza virus, Mycoplasma pneumoniae pneumonia, whooping cough, rubella and mumps. The facility is also likely be required to treat patients with airborne diseases such as measles and tuberculosis. Decreasing the risk of transmission of the various diseases would prove challenging in the deployed environment.11
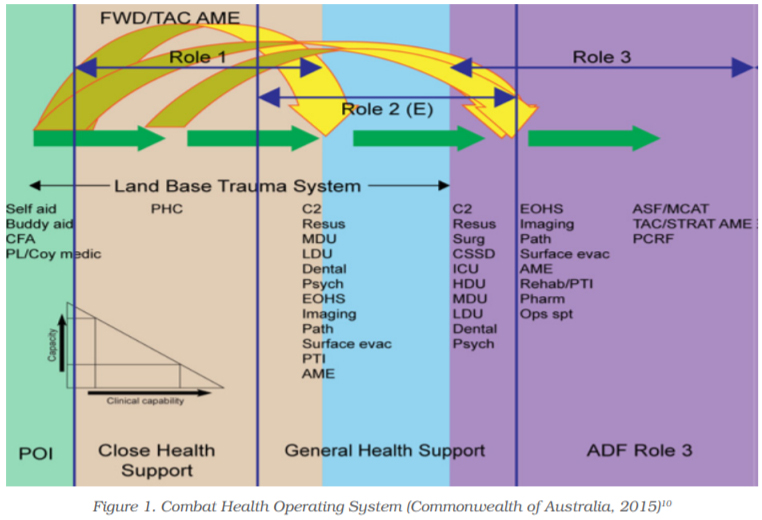
Within a military theatre of operations, care of the casualty commences at the point of injury (POI) with self aid, buddy aid, combat first aiders and medical technicians. Casualties are then transported to the next level of care, via armoured ambulances or medivac helicopter, depending on several factors: the combat situation, weather, terrain or transport assets available. While a Role 1 MTF may be available to provide non-specialist led advanced first aid and resuscitation, casualties are often transported from POI directly to either a Role 2 or a Role 3 MTF for specialist led treatment (Figure 1).Casualties are then evacuated to a civilian health facility outside of the combat zone7 as depicted in the Combat Health Operating System in Figure 1.12 Ensuring that HAIs are prevented while care is being provided along the complex evacuation chain is very challenging.
Various factors including the physical structure of the facilities (which can range from a series of interlocking tents to pre-existing buildings), the regular and constant turnover of healthcare workers (HCW), unfamiliarity with another nation’s MTF IPC procedures (for example, an ADF HCW deployed to work with a coalition partner’s MTF), climate (ranging from extreme cold to extreme humidity) and the presence of dust and sand (which greatly impacts on the successful cleaning of the environment) significantly challenge the prevention and management of HAIs.7 Other challenges include the provision of care to local nationals and the supply chain.3,7 There is no standardised clinical governance (CG) framework for the deployed setting; various ADF MTFs deploy with their own set of standards and guidelines. In contrast, the provision of healthcare to the ADF within Australian bases is facilitated by an organisation called Joint Health Command (JHC) utilising an integrated workforce that include defence members, civilians, contractors and other health professionals.13,14 The health standards that JHC and the ADF apply to garrison healthcare have been produced in conjunction with The Royal Australian College of General Practitioners (RACGP) Standards for Garrison Health Facilities in the Australian Defence Force. These standards provide a robust template for the delivery of safe and effective healthcare to the ADF, including IPC practices.
The Australian Army’s deployable surgical capability (NATO Role 2E or R2E) is provided by the 2nd General Health Battalion (2GHB).The unit has developed a CG framework to improve the services it provides and recognises the benefits of aligning with, and meeting, the standards of care equal to that provided within public and private civilian hospitals. To achieve this, 2GHB has implemented a continuous quality improvement (CQI) project that benchmarks against the national standards provided by the Australian Commission for Safety and Quality in Health Care (ACSQHC).3,15,16
This integrated review aims to investigate the contemporary international literature on the current practice strategies being utilised to improve IPC within the challenging combat environment. This will be used to inform 2GHB’s IPC practices as well as informing the IPC practices of the Royal Australian Airforce (RAAF) and Royal Australian Navy (RAN) deployable MTFs, and care provided by the Army’s 1st Close Health Battalion (1CHB), which provides close health support to the ADF. Defence forces from other countries may also use the information to improve their IPC practices.
Literature review – Search methods
An integrative review method17 was used to investigate current IPC practices. This methodology uses a systematic and rigorous method of reviewing data from various sources (experimental and non-experimental) improving the quality of data analysis and has the potential to allow for diverse primary research methods to play a greater part in evidence-based practice initiatives.14,15
A literature search of five bibliographic databases was conducted, which included Cumulative Index to Nursing and Allied Health Literature (CINAHL) Plus with full text, Medline, EMBASE, PubMed and ScienceDirect for articles published from January 2009 to January 2019.The search terms used in all databases were ‘infection control’ OR ‘infection prevention’ AND ‘military’, OR ‘military hospital’ OR ‘field hospital’. The search terms were entered into the individual databases using the advanced settings and were used to search by title, abstract and keyword.
To broaden the search, the reference lists of the selected articles were examined to identify other potentially relevant sources. Limiters for the search included English only full-text articles from 2009 to 2019, peer-reviewed to ensure currency of information. Exclusion criteria for the initial search included:
- editorials and correspondence
- items that were not journal articles, reviews, publications, government documents or observational studies
- items written in languages other than English
- published prior to 2009
- items not involving infection prevention, infection control, deployed military treatment facilities and field hospitals.
- The inclusion criteria were then refined to focus on the discussion of IPC practices utilised in deployed MTFs or field hospitals.
Quality assessment
The quality of the articles was assessed utilising the Mixed Methods Appraisal Tool (MMAT).19 Using this tool, the quality of articles was scored independently by two authors (JS and PZ) and assessed against the appropriate methodological criteria.
Results
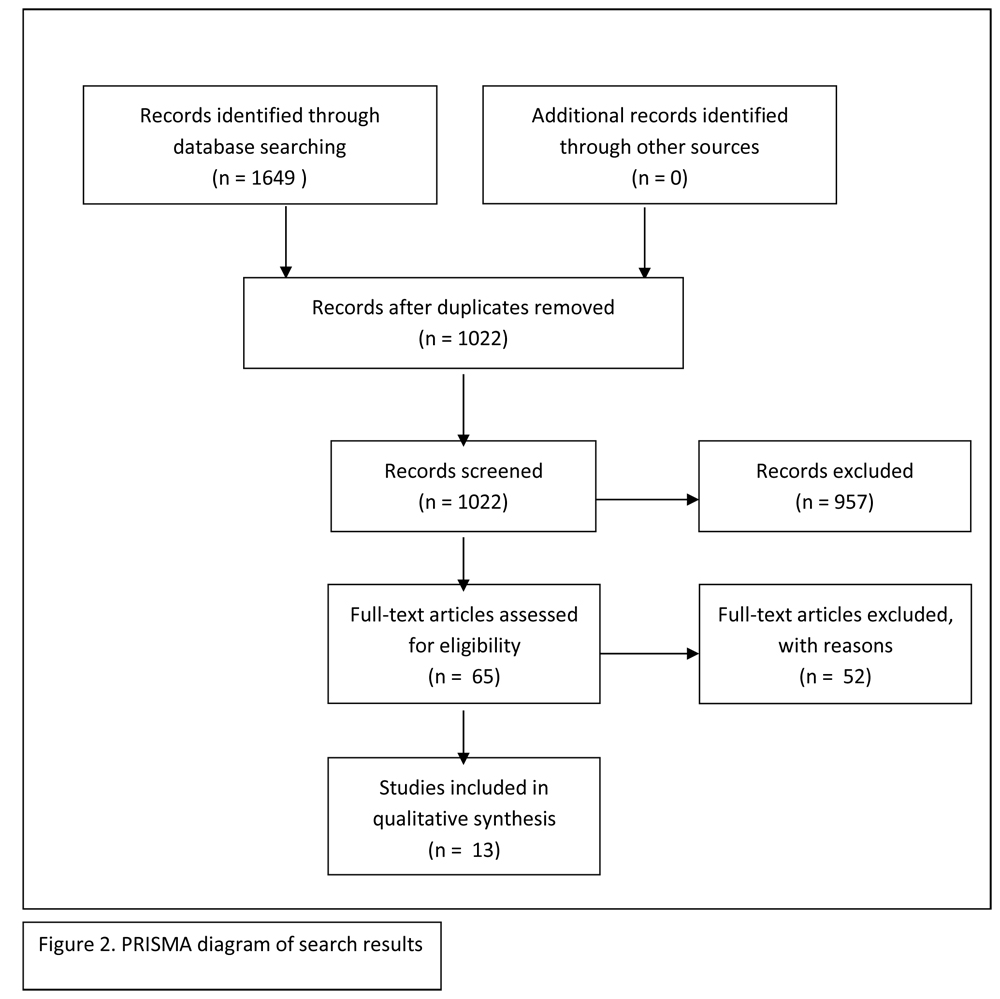
The search yielded a total of 1649 original articles. A total of 627 were discarded as they did not meet the inclusion criteria leaving 1022 articles. The study titles were reviewed leaving a total of 65 articles. The abstracts of these articles were screened leaving a total of 16 articles. An in-depth review of the full text and methodology was conducted, which left a total of 13 that met the inclusion criteria and identified current practice strategies being utilised to improve IPC within the challenging combat environment. Figure 2 demonstrates the search strategy. Based on the MMAT assessment and methodological criteria, article quality ranged from 50–100%.
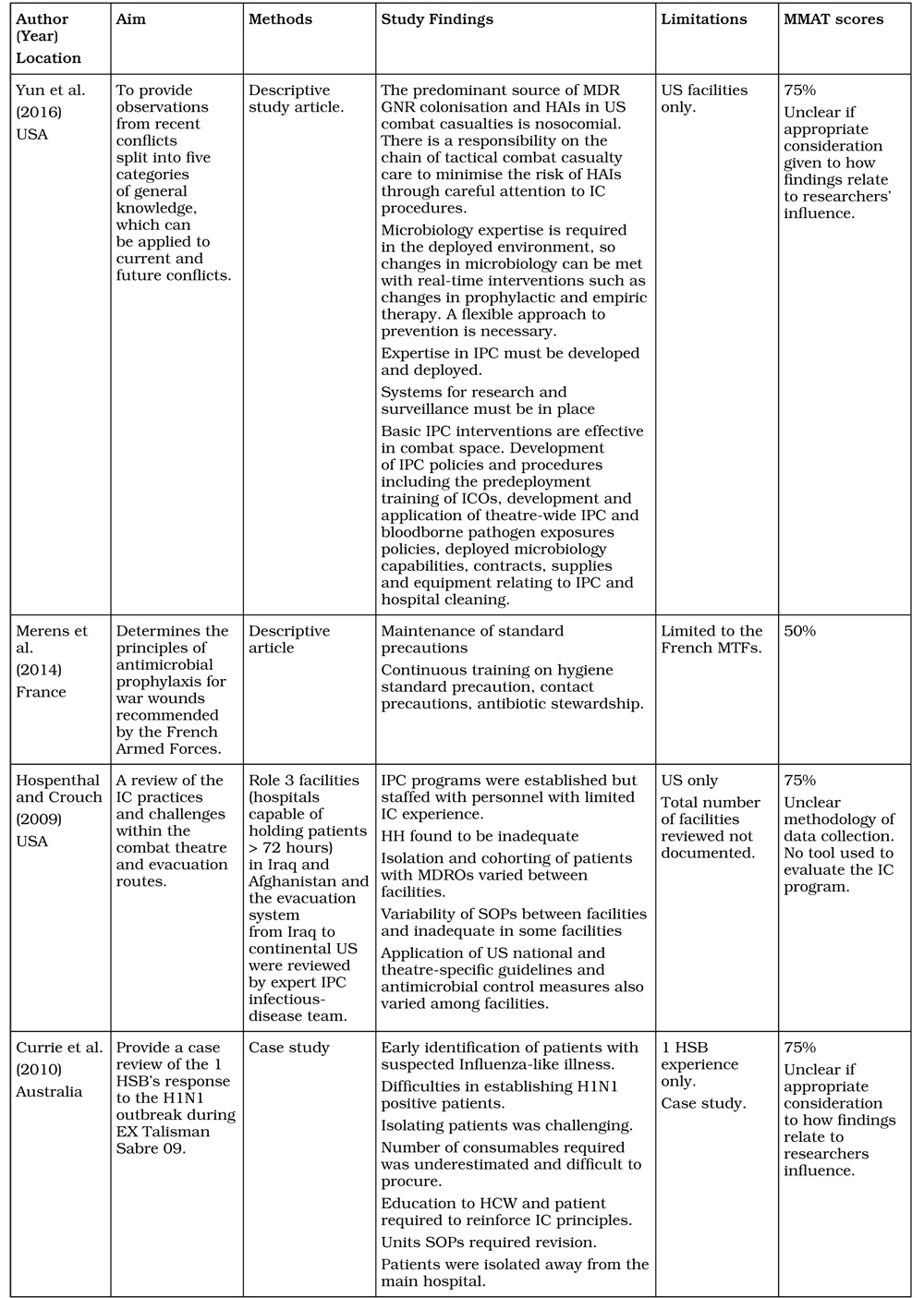
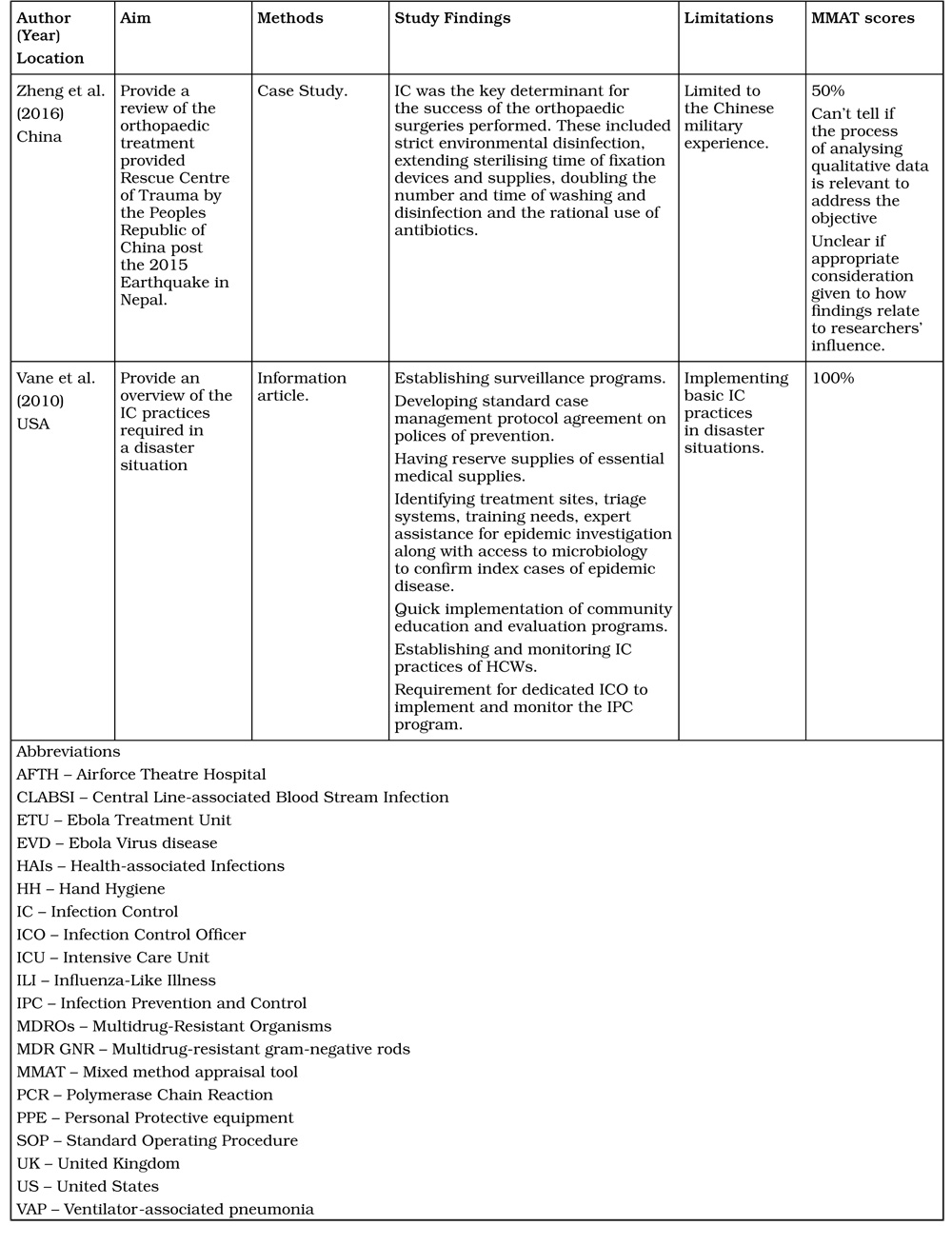
A summary of the included articles is provided in Table 1.Of the 13 articles reviewed, 11 articles had four main common themes that were discussed within each article. These themes are: 1) requirement for IPC expertise and education within deployed MTFs; 2) maintaining an emphasis on basic IPC measures (hand hygiene, environmental cleaning, and cohorting of patients); 3) the use of standard operating procedures (SOPs) and guidelines; and
4) antimicrobial stewardship. These themes were present across various settings including Iraq, Afghanistan, Nepal, Liberia and Sierra Leone. One article describes the introduction of a five-day predeployment IPC course for personnel deploying as an Infection Control Officer (ICO) within the MTFs. Another presents a case study of the deployment of the 1st Health Support Battalion (1HSB) to Exercise Talisman Sabre in 2009 during an H1N1 outbreak describing the challenges faced, highlighting the need for careful predeployment planning, ongoing education of HCW, surveillance and maintenance of basic IPC procedures.
Table 1. Summary of articles included in review
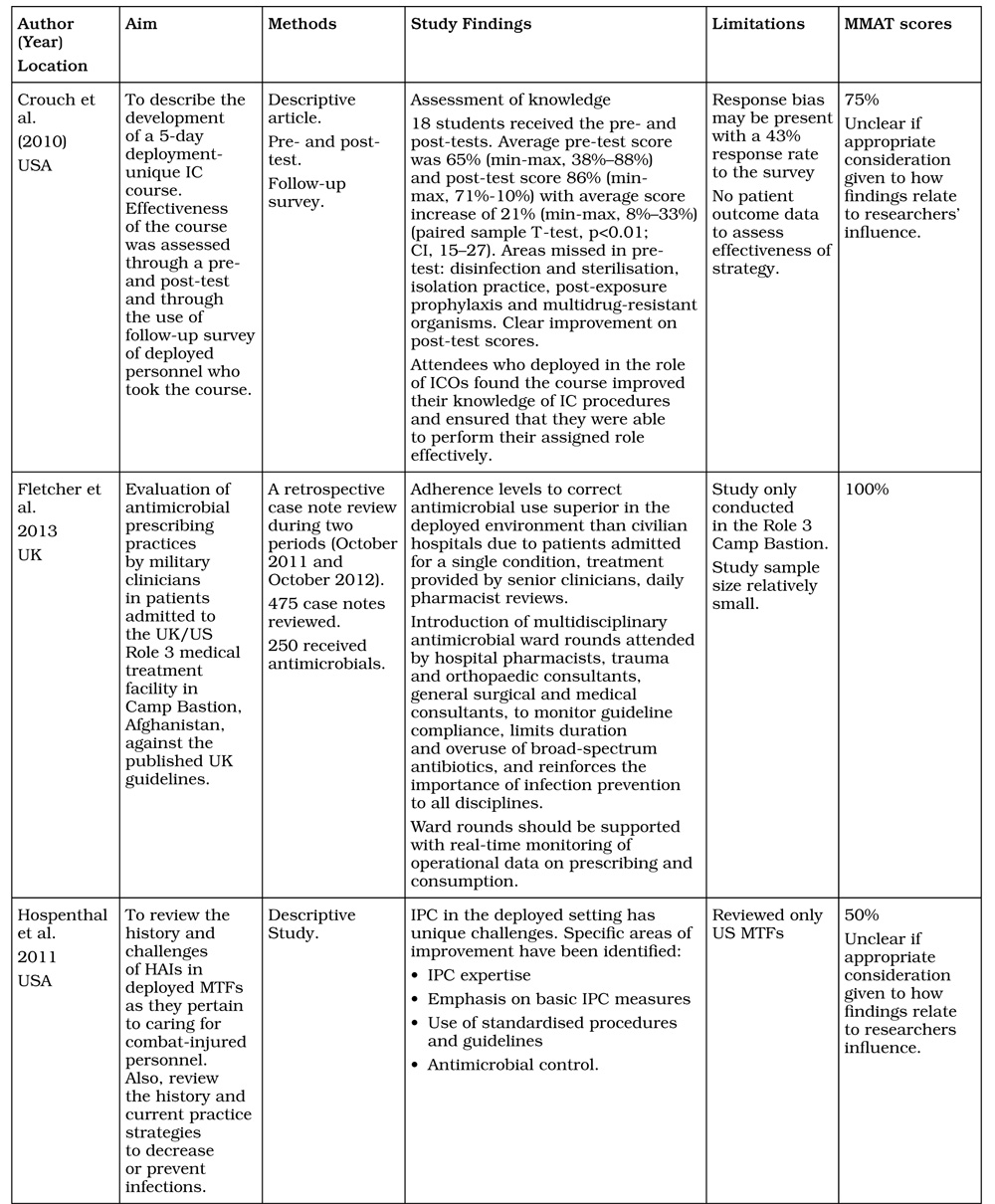
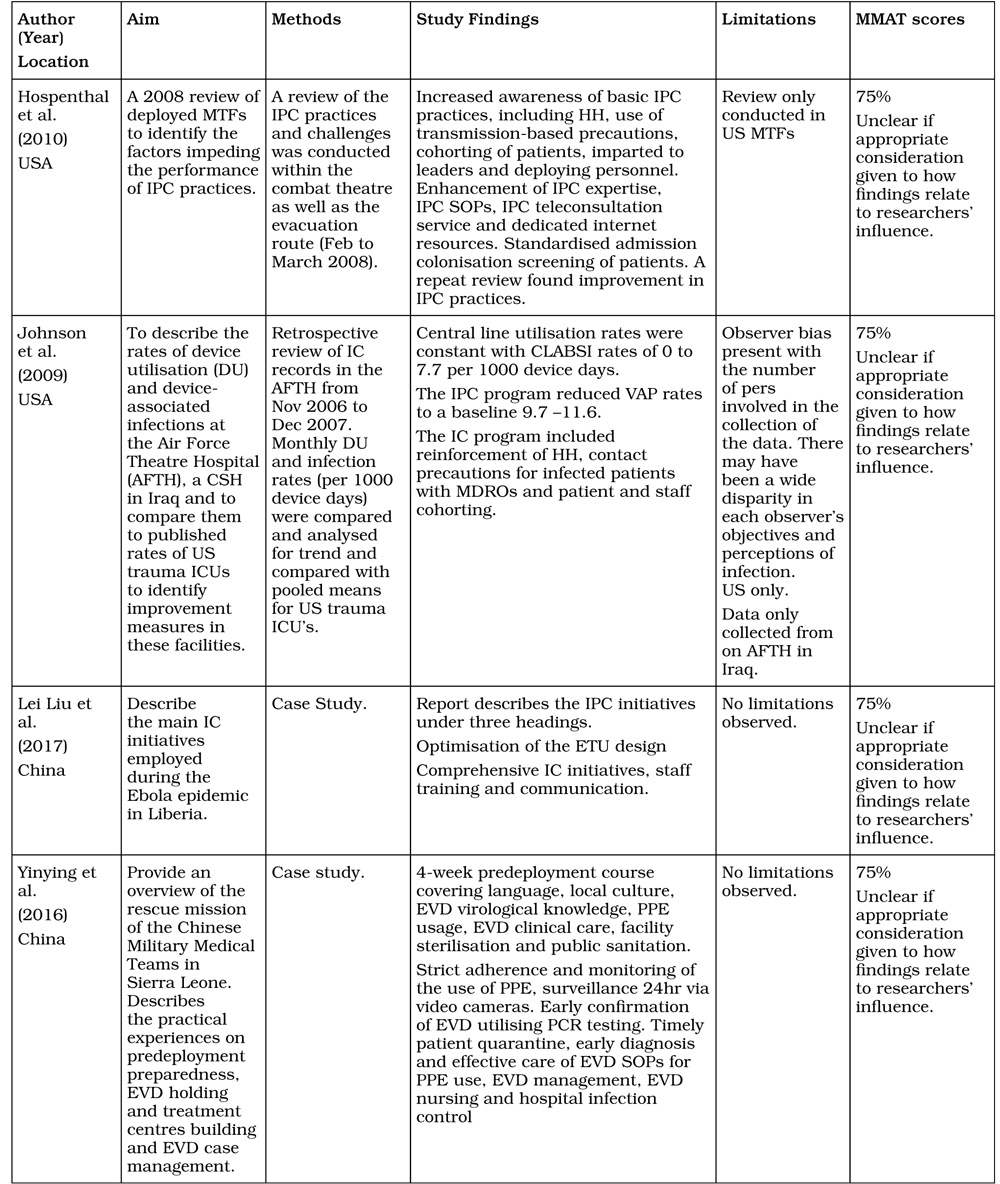
Infection prevention and control training and expertise
In a review by Crouch, Murray and Hospenthal of IPC practices within the theatre of operations of Iraq and Afghanistan, the authors identified standard IPC practices were not being implemented consistently across the various MTF’s within the theatre of operations potentially increasing the risk of HAI’s.5 They described the need for, and development of, a five-day predeployment course focusing on IPC in the deployed setting. This ensured that the ICO assigned to the deployed MTF had the relevant skills and knowledge to oversee and manage the infection control (IC) program within their facility ensuring compliance to IPC practices.5 All course attendees deployed to a Role 3 MTF. The course proved to be effective allowing the participants to perform their roles as ICO within the facilities. The requirement for IPC expertise and ongoing education is described in a further eight articles.1,4,7,17-22
Basic IPC measures
Of the 13 articles reviewed, nine described the importance of maintaining basic IPC measures.1,4,7,17-19,21-23 These articles described ensuring that hand hygiene (HH) is performed and monitored for compliance. Alcohol-based hand rubs (ABHR) should be available for use within combat zones and there should be strict adherence to the correct use of PPE to reduce infection risk to HCWs as well as patients.21,22 Modifications to isolation precautions required in the deployed environment are shown in Table 2.7 Frequent environmental cleaning is also required as part of IPC.23
Standard operating procedures
The revision and development of SOPs relating to IPC are discussed in three articles. Currie describes the ongoing continual revision and development of the SOPs utilised by 1HSB during the H1N1 outbreak in 2009.27 Hospenthal and Crouch in their review of the IPC practices and challenges within the combat theatre and evacuation routes found that there was distinct variability of the SOPs within the various MTFs and the SOPs were often found to be inadequate.4 They emphasised the need to develop theatre-wide IPC SOPs, which could be adapted by the local ICO if required for the individual MTFs.
Antimicrobial stewardship
Antimicrobial stewardship (AMS) is a key strategy in limiting antimicrobial resistance and decreasing preventable HAIs.28 This is discussed in depth in five of the 13 articles reviewed.4,7,17,18,26 An evaluation of antimicrobial prescribing habits in the UK/US Role 3 MTF at Camp Bastion Afghanistan was conducted in October 2011and 2012.29 It found adherence to the prescribing guidelines was superior to that found in civilian hospitals. This is most likely due to the patients being treated by senior medical consultants and daily checks of prescribing habits conducted by the pharmacist. The strict monitoring of antimicrobial use is advocated in the other four articles.4,7,20,21
Table 2. Isolation precautions to prevent transmission of infections in deployed hospitals Adapted from: Hospenthal and Crouch
| Isolation category | Patient placement | Healthcare worker PPE |
|---|---|---|
| Contact precautions | Ideal: Single room. Option: Bed separated from others by 2 metres. |
Ideal: Disposable gowns and gloves for all possible interactions with the patient or items within the patient zone. PPE and HH between patients. Option: Gloves with removal and HH after each patient interaction. |
| Droplet precautions |
Ideal: Single room. Option: Patients with same symptoms cohorted. Separation of 2 metres with curtains between patients. If no curtains separation of 3 metres between patients. |
Ideal: Mask when entering the room. Option: Mask within 3 metres of the patient. Patients to wear masks when transported. |
| Airborne precautions | Ideal: Single room with negative pressure ventilation. Air discharged to the outdoors. Doors to remain shut. Option 1: Single room with a fan exhausting then air outward. Door to remain shut. Option 2: If no single room available, the patient is to be admitted as far away from other patients as possible with a physical barrier around the patient. Do not admit the patient near air intakes. Option 3: Patients admitted to a single quarter separate from the main facility. |
Ideal: N95 mask when in the patient room. HCW should be fit tested using the N95 masks supplied by the facility. Option: N95 mask as above without fit test. Patient to wear surgical mask during transport |
Adapted from Hospenthal, Green and Crouch 7
Discussion
The maintenance of an effective and efficient IPC program in modern civilian healthcare has many challenges.1 In the deployed setting, these challenges are the same along with unique challenges that come with working within a theatre of combat.7 High personnel turnover, care of local nationals who are a potential source of MDROs4, the physical structure of the MTF, extremes in weather and the potential shortage of essential supplies for effective IPC pose challenges to optimising IPC.7
Previously within US MTFs, and currently within 2GHB, the ICOs received no formal training in IPC. They rely on SOPs that are often vague and don’t address the issues of the MTFs.4 The ICO role is usually secondary to their regular duties. Due to the ICO’s lack of expertise and the role being a secondary duty, errors in IPC practices are possible which could lead to an increase in HAIs. By comparison, UK Field Hospitals have dedicated ICOs who report directly to the Hospital Commander. Their IPC program is well established, and in combination with shorter evacuation times from Afghanistan, could account for the lower rates of HAIs in wounded UK personnel.27 Current practice within the US Army MTFs requires deploying Role 2 and Role 3 MTFs to identify and adequately train their ICO before deployment.31
Formal education for the ICOs and continuing education within the MTFs ensures that the IPC is effective during the deployment. Roup and Kelly32 (p1252) explain that ‘the underpinning of a successful IC program is regular education and communication. IPC must be given emphasis and responsible personnel to be successful’. To be effective, the IPC education must be designed for the area of operations the MTF will be operating in and include a range of topics from basic IPC practices to the diseases that are most likely to be observed.1
An example where continual education in IPC improves patient outcomes is the education program introduced to reduce the rates of ventilator-associated pneumonia (VAP) and central line-associated bloodstream infection (CLABSI) in a deployed MTF in Iraq from 2006 to 2007.23 The program reinforced strict adherence to good HH, utilisation of contact precautions when caring for patients with MDROs, staff and patient cohorting, strict AMS and cleaning of the ventilator equipment. Once implemented, the rates of VAP reduced from a baseline of 60 per 1000 device days to 9.7 to 11.6 per 1000 device days.23 A targeted predeployment program with ongoing education during deployments ensures that the IPC program is monitored and maintained potentially reducing the rates of HAIs. Correct HH with soap and water or ABHR is crucial in reducing HAIs. Van Camp and Ortega demonstrated that the use of ABHR in a non-deployed military setting reduced the number of lost duty days due to acute illness. They placed ABHR in the buildings of two aviation squadrons in 2005 and reduced the illness rate from 2.4% in 2004 with 210 duty days lost, to 0.9% with a total of 78 duty days lost in 2005.33 Less than ideal facilities, limited resources and a limited water supply influence HH compliance. Access to ABHR is likely to improve HH compliance.18 HH compliance monitoring is required within the deployed MTF.7
PPE such as gloves, gowns, masks and eye protection need to be used correctly. During the Ebola epidemic in Liberia in November 2014, the Chinese treatment teams implemented a 41-step PPE donning and doffing guide with the requirement for two persons at the don and doff. This ensured that any breaches in the donning and doffing procedure were identified and corrected.21 Adopting the process ensured that no HCW working within the Ebola Treatment Units (ETUs) became infected with Ebola.21 While this is an extreme example of correct use of PPE, it does demonstrate that ensuring PPE is used and applied correctly, it can mitigate the risk of transmission of pathogens from the patient to the HCW and vice versa.
Environmental cleaning of the hospital environment is a key element in the IPC program. Surfaces within the hospital that are frequently touched, such as bed rails and bedside tables, act as reservoirs for organisms that can be spread by the hands of the patients, visitors and HCWs. If a room or bed had been occupied by a patient with an MDRO, evidence suggests that subsequent patients are likely to become colonised with the same organism if environmental cleaning is performed incorrectly.31
In a recent multicentre controlled trial (REACH) conducted between May 2016 to July 2017, an environmental cleaning bundle was introduced into 11 hospitals around Australia.31 The bundles provided recommendations on cleaning supplies, frequency and techniques of cleaning, auditing the cleaning process and created a hospital-wide commitment to improving cleaning. As a result, environmental cleaning of frequent touchpoints in hospital bathrooms increased from 55% to 76% and bedrooms from 64% to 86%. Vancomycin-resistant enterococci infections reduced from 0.35 to 0.22 per 10 000 occupied bed days.31 Implementation of these cleaning bundles into the MTFs could potentially reduce the risk of the transmission of MDROs.
Transmission-based precautions within MTFs can be difficult to achieve due to the size and design of the facility. There is often a lack of available single rooms for infected patients. Adequate separation of the patients can be achieved by ensuring there is an area no less than two metres between the patients by having an empty bed between the patients or having the patient area marked off.1,7,18 Airborne precautions pose a more significant challenge in the deployed environment. Having the isolation ward separate from the main MTF may provide better protection to the other patients and staff.
The overuse of antibiotics in medicine has placed our ability to treat common infectious illness at risk.35 To reduce the risk of developing further MDROs, AMS should be part of the IPC program.29 The AMS program reduces the inappropriate use of antimicrobials, reducing bacterial resistance, patient morbidity, mortality and preserving the effectiveness of the antimicrobials currently available.28 Within Australia, it is a requirement that all healthcare25 providers have systems in place for the safe and appropriate use and prescribing of antimicrobials.28 Compliance with the AMS program can be achieved with a multidisciplinary approach with daily ward rounds that include the pharmacist, consultants and medical officers.29 Microbiology support should also be available to provide epidemiology and susceptibility data to direct antimicrobial therapy. For those facilities that do not have access to microbiology support, operating theatre antibiograms should be available to assist in the selection of empirical antimicrobial therapy.4
An expert review of the IPC SOPs should be conducted to ensure best practice is being followed and there is consistency of the SOPs across MTFs. Along with the SOPs, clinical practice guidelines (CPGs) specific to the care of combat-related infections can reduce the risk of HAIs and thus reduce morbidity and mortality, improve efficiency, ensure consistency in clinical practice and act as a valuable point of reference for clinicians.36
The main limitation of this study is that the articles reviewed are English only and only 13 met the inclusion and quality criteria of the study. Another is that while there is evidence that these interventions can improve IPC outcomes, given the inability to conduct randomised controlled trials of these interventions for ethical reasons (i.e. withholding interventions known to have a positive impact), the degree to which each of these contributes to improvedoutcomes cannot be determined
Conclusion
Conclusion
While the principles remain the same, IPC in the deployed MTF comes with a unique set of challenges. To ensure the IPC program is effective, this integrative review has identified four evidence-based overarching strategies/recommendations required.
Specialised training and expertise in IPC for ICOs to provide mandatory education in IPC predeployment (and during deployment) to all deploying HCWs, assist in the development and sustained implementation and evaluation of SOPs and CPGs, and adapt IPC principles to austere environments.
Provision of ongoing IPC education program during deployment with evaluation of practice standards through HAI surveillance.
Development, implementation, and evaluation of SOPs and CPGs for IPC in the MTF that include all aspects of standard and transmission-based precautions.
An AMS program in conjunction with the use of SOPs and CPGs to standardise the care of the patient and reduce the risks of MDROs and HAIs.
Preventing HAIs and limiting the spread of MDROs is the responsibility of all HCWs within the MTF. Establishing good IPC practices and procedures will reduce the risk of HAIs and prevent any further infection-related harm occurring to injured personnel or civilians in their care.
Corresponding author: John Skipp john.skipp@defence.gov.au
Authors: J Skipp1, P Zimmerman2,3,4, T Van de Mortel5
Author Affiliations:
1 Australian Army, 2nd General Health Battalion
2 Griffith University Griffith Health
3 Griffith University Menzies Health Institute Queensland
4 Gold Coast Health Service District
5 Griffith University, School of Nursing and Midwifery



