K Kerr, M Romaniuk, S McLeay, S Walker, J Henderson, A Khoo
Abstract
Background Australian veterans have an increased risk of posttraumatic stress disorder (PTSD). Guilt is a common post-trauma reaction; however, research in this area is limited.
Purpose This study aimed to explore the relationship between guilt, PTSD severity, alcohol use, anger, history of suicide attempts and deployment period among Australian veterans with PTSD.
Material and Methods A retrospective analysis was conducted on 219 ex-service personnel diagnosed with PTSD who attended a Military Trauma Recovery Day Program. Veterans completed self-report questionnaires as well as a clinician-administered PTSD assessment tool. Demographic information and self-reported history of suicide attempts were also recorded.
Results Guilt scores were significantly correlated with PTSD severity (R=0.411), anger (R=0.373) and alcohol use (R=0.239). Guilt was most strongly correlated with the re-experiencing cluster of PTSD (R=0.420), although it was significantly correlated with all clusters (hyperarousal R=0.343, and avoidance R=0.327). Guilt scores were significantly higher in those who had attempted suicide and for contemporary veterans.
Conclusions In Australian veterans with PTSD, guilt was significantly associated with PTSD severity, anger, alcohol use, attempted suicide and being a contemporary veteran. The study highlights the importance of guilt identification and treatment by clinicians for improved outcomes.
Conflicting interests The authors declare that there are no conflicts of interest.
Introduction
Compared to the general population, Australian veterans have an increased risk of being diagnosed with posttraumatic stress disorder (PTSD),1 a psychiatric condition characterised by symptoms of re-experiencing, hyper-arousal, avoidance and alterations in cognitions and mood following exposure to a single or multiple traumatic events.2 The 2010 ADF Mental Health Prevalence and Wellbeing Study estimated that 8.3% of Australian Defence Force members had experienced PTSD in the past 12 months. In contrast, the incidence of PTSD in the general Australian community in the same time frame was 5.2%.1 It is recognised that active service can result in witnessing, failing to prevent or committing acts during combat and peacekeeping missions that violate personal values and morals.3 These experiences can trigger various emotions, and guilt is a common and significant reaction to trauma.4
Guilt is a retrospective emotion and can be conceptualised as a psychological state involving perceived moral transgressions linked to action (or inaction) or behaviour, whereby individuals feel a sense of regret or remorse.5,6 There is a lack of consensus within the literature regarding whether the emotional experience of guilt is adaptive or maladaptive to human functioning.4 Some types of guilt, such as behavioural guilt, may serve a prosocial function by encouraging individuals to change maladaptive behaviours.7,8 However, trauma-related characterological guilt (wherein an individual self blames and attributes the trauma or its consequences as arising from negative personal characteristics such as a direct result of them being a bad, defective or worthless human being) is associated with worse psychopathology.7,8 Certain types of guilt increase the risk of developing PTSD, depression and substance use disorders.9,10 Research has also shown traumatic guilt to have a strong correlation with general measures of PTSD severity as well as various symptom clusters of the condition.5,11,12,13
A number of theoretical and statistical models have been developed to explain the relationship between guilt and PTSD. Individuals with PTSD often avoid negative memories, feelings and thoughts associated with the trauma they experienced, and this may consequently block their ability to process feelings of guilt.14 Guilt can also emerge if a traumatic experience violates an individual’s personal morals, values and standards, which can lead to intrusive thoughts and ruminative activity. 15,16
Trauma-related guilt has been found to partially mediate the relationship between PTSD and depression in veterans exposed to combat.11, 17 Marx et al.17 examined a sample of 1323 male Vietnam veterans in which combat-related guilt was found to partially mediate the association between exposure to violence in combat and PTSD symptomatology.
Furthermore, guilt completely mediated this relationship when the individual was directly involved in the violence.17 This indicates that greater personal involvement in an event can influence guilt in the development of PTSD symptoms.17 The amount of guilt an individual may experience after a traumatic event is also related to their perceived failures to prevent, or try to prevent, the event.15,18
Using conditional latent growth mixture modelling, very high levels of guilt, combined with very high PTSD and depression scores, were found to predict the poorest treatment response in Australian veterans who completed a trauma recovery program.19 However, for those who had very high PTSD scores but low guilt scores, large symptom improvement was found, highlighting the role that guilt plays in clinical treatment and outcomes of veterans.19
Guilt has also been found to be a strong predictor of suicidal ideation among veterans. Bryan et al.6 studied 69 active service military personnel engaged in outpatient mental health treatment who completed self-report tools measuring shame, guilt, PTSD, depression and suicidal ideation. In those with a history of suicidal ideation, feelings of guilt were significantly higher.6 Additionally, guilt was independently and significantly associated with increased frequency and severity of suicidal ideation, with this relationship stronger than that of depression and/or PTSD.6 In a sample of Vietnam combat veterans, guilt about combat actions was the most significant predictor of suicidal ideation and attempts compared with depression, anxiety, PTSD and survivor guilt.20 These findings were further supported in a study of Iraq and Afghanistan combat veterans whereby guilt was significantly correlated with suicidal ideation.6
Much of the research on guilt in veterans as a specific population has primarily occurred in a US context and has examined those who served during the Vietnam era. There is a lack of research using Australian veteran samples focusing specifically on traumatic guilt and its relationship with psychopathology and suicide attempts within this population.
The current study aimed to explore the relationship between guilt, PTSD severity, alcohol use, anger and service period (contemporary vs older conflicts) among Australian veterans with PTSD. Contemporary veterans were defined as veterans who had Australian military service from 1999 onwards 21 and were of interest due to the increased demands of contemporary service, including longer and more frequent deployments and potentially a more ambiguous enemy.16 Furthermore, the study aimed to determine whether guilt was higher among those who had a history of attempting suicide.
Method
Participants
Data were available for 219 veterans, including 217 males (99%) and 2 females (1%) aged 24–86 years
(52.9 ± 13.3). One hundred and forty-nine (68%) had served exclusively in the Army, 32 in the Navy (14.6%), 30 in the Air Force (13.7%), and 8 (3.7%) served in multiple branches. One hundred and forty veterans had served in conflicts or operations prior to East- Timor, and 61 had served in more recent operations. Of the total cohort, 110 veterans served in Vietnam, 34 served in Iraq and/or Afghanistan, 57 served in peacekeeping or peacemaking operations (e.g. East Timor, Somalia, Rwanda), and 18 did not have active service.
Descriptive demographics of the studied population are presented in Table 1.
Table 1: Summary demographics of studied population
| Demographic | n total n = 219 |
% | Mean | SD | Range |
|---|---|---|---|---|---|
| Age | 52.9 | 13.3 | 24-86 | ||
| Sex | |||||
| Male | 217 | 99.0 | |||
| Female | 2 | 1.0 | |||
| Marital status | |||||
| Married | 150 | 69.0 | |||
| De facto | 11 | 5.0 | |||
| Separated/divorced | 38 | 17.0 | |||
| Widowed | 4 | 2.0 | |||
| Single | 16 | 7.0 | |||
| Highest education level | |||||
| Primary | 4 | 2.0 | |||
| Secondary | 112 | 51.0 | |||
| Trade | 41 | 19.0 | |||
| College | 39 | 18.0 | |||
| University | 23 | 10.0 | |||
| Employment status | |||||
| Full-time | 53 | 24.2 | |||
| Part-time | 14 | 6.3 | |||
| Retired | 51 | 23.3 | |||
| Not working/unable to work/TPI | 96 | 44 | |||
| Other | 5 | 2.2 | |||
| Service branch | |||||
| Army | 149 | 68.0 | |||
| Airforce | 30 | 13.7 | |||
| Navy | 32 | 14.6 | |||
| Multiple | 8 | 3.7 | |||
| Conflicts served | |||||
| Pre-East Timor only | 132 | 60.0 | |||
| Served from East Timor onwards | 61 | 28.0 | |||
| Served in both periods (Pre-East Timor onwards) | 8 | 4.0 | |||
| Not deployed | 18 | 8.0 | |||
| Trauma from deployment | 201 | 91.8 | |||
Procedure
The study was a retrospective analysis of data collected as part of routine practice for Australian veterans who attended the Military Trauma Recovery Day Program (TRP) as outpatients at Toowong Private Hospital over seven years. A veteran was defined as a person who had served in the ADF at any time point. The TRP is a cognitive behaviour therapy (CBT) based program in which veterans attend four days per week for six weeks, then two days per fortnight for another six weeks, with two one day follow-up sessions at three and nine months. All veterans were diagnosed with PTSD by their referring psychiatrist.
Prior to the commencement of the TRP, they participated in a multidisciplinary pre-admission assessment with interviews by a psychiatrist, clinical psychologist and social worker to confirm their PTSD diagnosis and to assess their suitability for a group program.
A chart review was conducted to collect demographic and service data, including age, gender, education level, marital and employment status, conflicts served in, number of years in the military and roles in combat and/or peacekeeping missions (categorised according to the Australian War Memorial22). Formal measures were also completed as detailed in the measures section. Ethics approval for the study was obtained from the Department of Veterans’ Affairs (E012/008) and Griffith University (PSY/17/12/ HREC). Written consent was gained from participants as per the TRP protocol.
Measures
Participants completed several self-report questionnaires administered at intake to the TRP, which assessed symptoms of PTSD, anger, alcohol use and guilt. History of suicide attempts was assessed by asking the veterans, ‘Have you made a previous attempt on your own life?’ The Clinician-Administered PTSD Scale for Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV) (CAPS-IV) was administered at pre-admission assessment (one week to one month before the commencement of the TRP). A brief description of each questionnaire is below.
The Clinician-Administered PTSD Scale for DSM-IV (CAPS-IV):
The CAPS-IV is a structured clinician-administered assessment tool containing 30 items corresponding to the DSM-IV-TR criteria for PTSD. The CAPS-IV has shown good psychometric properties across various clinical populations and research settings.23 It has good sensitivity (0.84) and specificity (0.95) and has excellent test-retest and inter-rater reliability.24
The Alcohol Use Disorders Identification Test (AUDIT):
The AUDIT was developed by the World Health Organization and is a 10-item self-rated screening tool used to assess hazardous and harmful alcohol consumption. It contains questions on alcohol consumption and dependence, drinking behaviours and questions related to problems and consequences of drinking. Scores range from 0 to 40, with higher scores indicating higher risk. The test has shown good sensitivity (0.86) and specificity (0.89).25
Dimensions of Anger Reaction (DAR):
The DAR is a seven-item self-report questionnaire used to measure anger disposition, with scores ranging from 0–56. Higher scores indicate stronger anger reactions. In Vietnam veterans with combat- related PTSD, the DAR was found to be a reliable and sensitive measure of anger with an internal consistency of 0.91.26
Experiences of guilt:
Guilt was assessed using the associated features questions on the CAPS- IV, which consisted of two items. The questions included: 1. ‘How much of the time in the past month have you felt guilty about anything you did or did not do during your military service?’ 2. ‘How much of the time in the past month have you felt guilty about surviving a traumatic event when others did not?’ Clinicians rated each item from 0 (none of the time) to 4 (most of the time), and then assessed intensity by asking: ‘How strong were these feelings of guilt?’ Scores ranged from 0 (no feelings of guilt) to 4 (extreme, pervasive guilt). Total scores range from 0–16. The internal consistency has been cited as high (0.89), with item-total correlations ranging from 0.84-0.86.19
Data analysis
Statistical analyses were performed using R, version 3.13.27 Continuous demographic and psychological data were described by their mean, standard deviation (SD) and range, and categorical data by count and per cent (%) of the total population. Correlations between continuous psychological data were assessed by generating scatterplots and determining the correlation coefficient (R) for each relationship. Strengths of correlations were considered to be very weak where R<0.2, weak (R = 0.2–0.4), moderate (R = 0.4–0.6), strong (0.6–0.8) or very strong where R >0.8.28 Relationships between continuous psychological data and binary variables (history of suicide, conflicts served—pre- East Timor or East Timor onwards—and trauma from deployment) were assessed by non-parametric Mann-Whitney tests with data presented as box- and-whisker plots. Significance level was considered as p < 0.05.
Results
Summaries of CAPS-IV, DAR, AUDIT scores and history of suicide attempts are presented in Table 2, with 24.2% (n=53) of veterans having attempted suicide. Guilt scores were found to be significantly positively associated with all measures, being moderately correlated (R = 0.4–0.6) with CAPS- IV score, and weakly correlated (R = 0.2–0.4) with DAR and AUDIT. Plots of CAPS-IV, DAR and AUDIT scores against guilt scores are presented in Figure 1, with correlation coefficients and significance levels presented in Table 3.
The authors also explored if guilt was more strongly correlated with any of the CAPS-IV cluster scores (re- experiencing [cluster A], avoidance [cluster B], and hyperarousal [cluster C]). Guilt was most strongly correlated with the re-experiencing cluster (R = 0.420, moderate correlation). All other relationships showed weak (R = 0.2–0.4) but significant correlations (Table 2). Guilt scores were significantly higher in those who had a history of attempted suicide (p = 0.00642) and contemporary veterans who had served in conflicts post-East Timor (p = 0.0410) (Figure 2, left and centre panels). Guilt scores were not significantly different between those who had trauma from deployment and those who had guilt from non-active service.
Table 2: Summary statistics of psychological measures explored in the analysis and history of attempted suicide, n=219
| Psychological measure | N | % | Mean | SD | Range |
|---|---|---|---|---|---|
| Guilt | 6.62 | 4.31 | 0-16 | ||
| CAPS-IV total score | 69.2 | 21.3 | 20-116 | ||
| Cluster A: Re-experiencing | 17.7 | 8.88 | 0-39 | ||
| Cluster B: Avoidance | 27.4 | 9.75 | 2-51 | ||
| Cluster C: Hyperarousal | 24.0 | 6.10 | 5-36 | ||
| AUDIT | 14.9 | 9.31 | 0-40 | ||
| DAR | 30.6 | 14.2 | 0-56 | ||
| History of attempted suicide | 53 | 24.2 |
Figure 2
Correlation betweeen guilt scores with CAPS, DAR and AUDIT scores
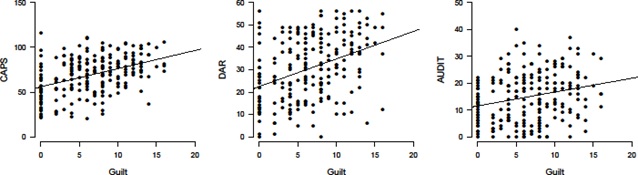
Table 3: Correlation between guilt scores with CAPS, DAR and AUDIT
| CAPS | CAPS Cluster A Re- experiencing | CAPS Cluster B Avoidance | CAPS Cluster C Hyperarousal | DAR | AUDIT | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| R | p-value | R | p-value | R | p-value | R | p-value | R | p-value | R | p-value | |
| Guilt | 0.411 | 2.42e- 10*** |
0.420 | 8.91e- 11*** |
0.327 | 7.37e- 7*** |
0.343 | 1.89e- 7*** |
0.373 | 1.18e- 8*** |
0.239 | 0.000369*** |
*p < 0.05, **p < 0.01, ***p < 0.001.
Figure 2
Relationship between guilt scores with history of previous suicide attempts, contemporary veteran (defined as service post-East Timor) and deployment
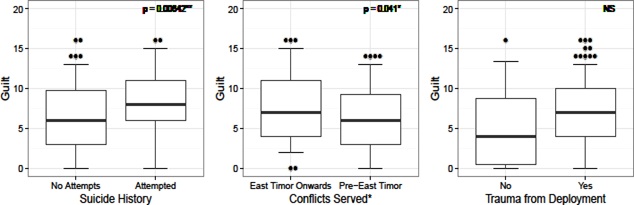
NS, not significant, p < 0.05, **p < 0.01, ***p < 0.001. Plots show the median and 25th-75th percentile range (box) and 5th-95th percentile range (whiskers). *Excluding veterans who served across both periods.
Discussion
The current study aimed to explore the relationship between guilt, PTSD severity, alcohol use, anger and period of deployment and to determine whether guilt was higher among those who had a history of suicide attempts. It was found that all these factors were significantly correlated with guilt. Additionally, being a contemporary veteran was significantly associated with guilt. To the best of the authors’ knowledge, no previous research has investigated suicidality concerning guilt among Australian veterans with PTSD. In line with previous research, it was found that guilt was significantly correlated with PTSD severity. This suggests that patterns within the Australian cohort are similar to those reported from the US with higher levels of guilt associated with increased PTSD psychopathology.5,11,12 For PTSD symptomology, guilt was strongly related to each of the symptom clusters, with the strongest association found for re-experiencing symptoms.
Henning & Frueh12 also found the severity of guilt regarding combat situations was positively correlated with the re-experiencing of PTSD. Re-experiencing could be conceptualised as the brain replaying an event in an attempt to process a resolution or try to find alternative ways of thinking about the event.
Guilt was significantly positively associated with self- reported anger and alcohol use within the veteran population; however, this relationship was weak. The relationship between anger and PTSD severity in combat veterans has been well established in the literature.29,30 In contrast, little empirical evidence exists regarding the relationship of guilt to anger, and the research that does exist demonstrates inconsistent findings; indicating further research is required to determine if the positive relationship can be replicated.31 In regards to guilt being associated with higher alcohol use, this may be the first study to specifically examine the relationship between these variables among Australian veterans. A similar finding was found by Okulate and Jones,32 with a significant association between survivor guilt and alcohol use among inpatient Nigerian military personnel who served as peacekeepers in the Liberian and Sierra-Leonean wars. This finding could indicate that veterans use alcohol to numb painful guilt cognitions and emotions; however, further research is needed to examine this specifically.
The study also determined that veterans experiencing higher levels of self-reported guilt were more likely to have previously attempted suicide. This is consistent with Bryan et al.’s5,6 results, which found guilt was significantly associated with more frequent and severe suicidal ideation in a sample of American combat veterans. Many veterans report direct culpability for their actions and/or inactions during deployment, which results in guilt.16 Guilt is experienced as a sense of remorse and regret, which can be psychologically and physically painful and uncomfortable, especially when reparation cannot be made, which is often the case in active service situations.31 Suicide is recognised as a way to escape painful emotions.33
The current study also found that contemporary veterans who had served in conflicts post-East Timor were more likely to experience traumatic guilt. A significant correlation between being an Australian contemporary veteran and suicide attempts has been previously established34. Litz et al.16 stated there are increased demands on contemporary defence force personnel with longer and more frequent deployments resulting in more repeated exposure to tragedy and horror. They argued that contemporary veterans had had many unconventional threats in their theatres of war, such as unidentifiable enemy, the use of technology (drone attacks, improvised explosive devices) and civilian threats leading to more morally ambiguous situations, increased opportunity for collateral damage, more chance of acting outside of beliefs and value systems, and hence, increased chances of guilt.16 It is also possible there is a time bias, where contemporary veterans have not had as much time to process their military experiences.
Limitations and directions for future research
Several limitations of the study need to be acknowledged. The study was retrospective and did not examine the past psychopathology and guilt scores of veterans who had suicided, who may have had different profiles compared to suicide attempters. Ethical and practical considerations limit research that examines suicidality. The current study used a brief two-item measure of guilt, which is somewhat limited. That said, measurement variability is a limitation throughout the guilt literature, as the construct of guilt is often not distinguished from the construct of shame clearly and consistently.31 As such, future research could examine the link between guilt (and related constructs) with psychopathology using multiple psychometric measures allowing a more multifaceted conceptualisation of guilt. In addition, future research should focus on determining the effective treatment of cognitions and feelings tied to guilt.
Conclusion
Among a cohort of Australian veterans with PTSD, there was a significant positive association between guilt and severity of PTSD symptoms, anger and alcohol use. In addition, guilt was significantly higher among contemporary veterans and those who had attempted suicide in the past. These results highlight the importance of early identification of guilt by clinicians and the application of effective treatment to repair or reduce feelings of guilt.
Corresponding Author: Katelyn Kerr
Authors: K Kerr 1,2,5, M Romaniuk3,4,6, S McLeay3,7, S Walker 1,8, J Henderson1,9, A Khoo1,3,7
Author Affiliations:
- Toowong Private Hospital
- Australian Institute for Suicide Research and Prevention
- Gallipoli Medical Research Foundation
- Institute of Health and Biomedical Innovation
- Savior Rooms
- Institute for Resilient Regions
- The University of Queensland
- Supported Pathways
- Lilley Place


