Introduction
The US Department of Veterans Affairs (VA) spent US$64.7 billion in FY2016 on disability compensation for US Veterans of all eras with service-connected conditions – 37.5% (US$24.4 billion) was spent just on Vietnam-era Veterans (VNE: January 9, 1962-May 7, 1975).1 VNE Veterans are the second largest cohort of US living Veterans (6.2 million), of whom 2.7 million were deployed to the Vietnam Theater.2
‘Service connected’ refers to conditions that were caused or aggravated by military service.3 VA service-connected disability compensation is administered by the Veterans Benefits Administration (VBA) and is based on severity of service-connected disability as well as number of dependents. A combined disability-rating percentage expresses service-connected disability severity on a scale from 0% (not compensable, but related to service) to 100% (most disabling) in increments of 10%. Higher disability ratings result in higher compensation payments and more generous Veterans Health Administration (VHA) access.1
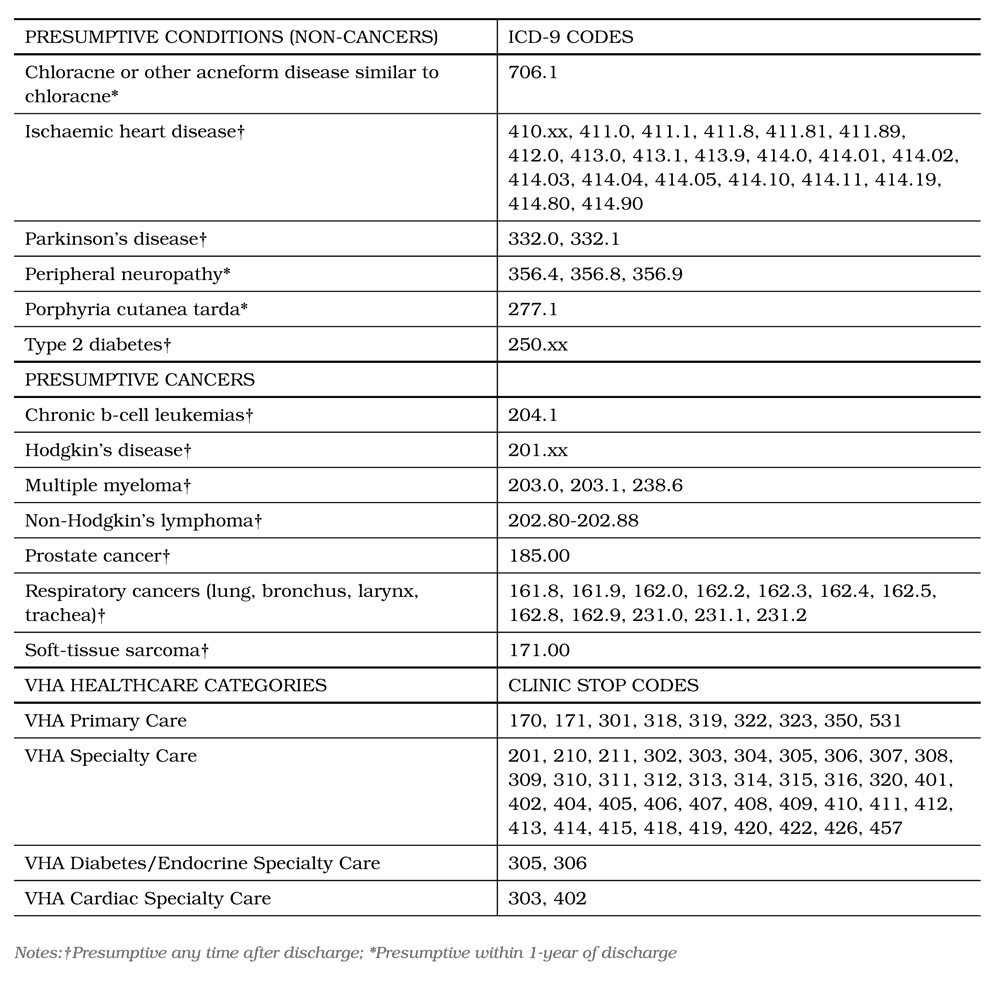
Between 1962 and 1971, the US military sprayed almost 20 million gallons of Agent Orange (AO) over the Republic of Vietnam (RVN).4 AO refers broadly to a class of herbicides that were used to defoliate areas of the jungle and landscape.5 These herbicides were contaminated with dioxin, a known cause of certain cancers and other adverse health effects.5 Currently, 14 conditions (Appendix I) presumed to be associated with AO exposure have been designated as presumed (presumptive) service-connected conditions.6 Type 2 diabetes (DM) and ischaemic heart disease (IHD), both prevalent and costly chronic conditions, were designated as ‘presumptive’ in 2001 and 2010, respectively. A VNE Veteran seeking to establish service connection for a presumptive condition need only provide evidence of a clinical diagnosis and of having ‘stepped foot’ in the RVN between January 9, 1962 and May 7, 1975.5 Once these requirements are met, exposure to AO is presumed because it cannot be documented and presumptive service connection is awarded.
Presumptions, by eliminating the need for Veterans to prove exposure, make it easier for them to receive service connection and thereby access the VA disability system.7,8 Importantly, Veterans with presumptive conditions must apply for presumptive benefits and the VA service connection application process can be complex and time consuming.8,9 Despite legislation and VA policies intended to facilitate service connection, little is known about Veterans’ uptake of presumptive service-connection benefits. Prior work suggests, however, that not all qualified Veterans with diagnosed presumptive conditions apply for and receive their presumptive service-connection benefits.10,11 In this study, we refer to the presence of a diagnosed presumptive condition in the VHA electronic medical record in the absence of a presumptive service-connection award for that condition in the VBA compensation database as a ‘presumption gap.’ We use the term presumption gap to indicate that a Veteran has not received his or her presumptive benefits.
Because the US has a national interest in ensuring that Veterans have access to high-quality VA benefits and services,9 we examined factors potentially associated with presumption gaps among Vietnam Theater Veterans with diagnosed DM or IHD. As DM and IHD were designated as presumptive at different times (DM in 2001, IHD in 2010), we hypothesised that IHD presumption gaps would be more prevalent than DM presumption gaps because less time had
elapsed for Veterans to apply for and be granted service connection for IHD. We further hypothesised that presumption gap would be associated with poorer health (interfering with Veterans’ ability to apply for presumptive benefits) and lower VHA utilisation (representing a higher cost barrier to access).
Materials and methods
The cohort was assembled from the Veterans Service Network Corporate Mini Master File (VETSNET), the primary source of information regarding disability benefits. VETSNET consists of selected fields from the VBA Corporate Database. This database supports the systems used to administer Veterans’ benefits including compensation and pension benefits. VETSNET has been cited in prior work.12,13 In this analysis, we used scrambled Social Security numbers to link VETSNET to VHA data.13,14 The VETSNET data extract provided cross-sectional information as of April 2013 for 1 186 967 VNE Veterans who were receiving VBA benefits for service-connected disabilities.
Because we were interested in Veterans who were likely to have stepped foot in RVN, we used the Vietnam Theater flag (a binary theater/nontheater indicator available in VETSNET) to initially select 317 545 (26.7%) Vietnam Theater Veterans determined by VBA through manual review of military service documentation to have been deployed to theater. We excluded 869 422 (73.3%) Veterans whose presence in the Vietnam Theater was less certain. We then selected 196 650 (61.9%) with at least one inpatient visit recorded in the VHA Patient Treatment File (PTF) during FY11-FY13 (VHA PTF contains information on each inpatient care episode) or one outpatient visit recorded in the VHA Outpatient Event File (OEF) during FY11-FY13 (VHA OEF contains information on each outpatient encounter). We excluded 120 895 (38.1%) with no VHA use in FY11-FY13.
Among the analytic sample of 196 650 Vietnam Theater Veterans, 125 399 (63.7%) had diagnosed DM and 71 251 (36.3%) had diagnosed IHD recorded in VHA electronic medical records. To determine the presence of diagnosed DM or IHD, we required at least two International Classification of Diseases Ninth Revision (ICD-9) codes within a 24-month period (FY2011–FY2012) to avoid unconfirmed or rule-out diagnoses.15
Among those with DM, we considered the presence of a diagnosis for DM in the VHA electronic medical records in the absence of a presumptive serviceconnection award for DM in the VBA compensation database to be a ‘DM presumption gap’. Among those with IHD, we considered presence of a diagnosis for IHD in the VHA electronic medical records in the absence of a presumptive service-connection award for IHD in the VBA compensation database to be an ‘IHD presumption gap’.
Dependent variables
Two binary dependent variables were used to examine presumption-gap status in 2013. The first dependent variable was DM presumption-gap status in 2013 (DM presumption gap/no DM presumption gap). The second dependent variable was IHD presumption-gap status in 2013 (IHD presumption gap/no IHD presumption gap).
Independent variables
Variables were extracted from VHA electronic medical records and VBA compensation database records. Veteran characteristics extracted included age, gender, race, marital status, number of chronic comorbidities and presence of diagnosed posttraumatic stress disorder (PTSD). Because Medicare enrolment by older VHA patients may impact their VA system utilisation patterns,16 continuous variable age (extracted from VHA PTF) was transformed into
a dichotomous variable representing subjects who were 66 years of age or older in 2013 (Medicareenrolment age), or less than 66 years of age (Not Medicare enrolment age). Because some studies have found that blacks are less likely than whites to receive VA service-connection benefits,17 race/ethnicity (extracted from VHA PTF) was categorised
as white, non-white or unknown/missing. Additionally, sex (male/female) and marital status (married, unmarried, unknown/missing) were also extracted as they correlate with service-connection award status and payment amount.18,19
To account for differences in comorbidity burden between those with and without presumption gap, we computed Charlson comorbidity index score (Deyo adaptation), which assesses the overall burden of disease and is associated with mortality (higher scores are associated with higher mortality). Charlson scores are based on the medical impact of up to 19 chronic conditions as recorded in the VHA PTF or the VHA OEF in FY2013. Further details on Charlson score can be found elsewhere.20 The continuous score was transformed into an ordinal variable representing subjects with scores of 0, 1-2 or 3+.
Because PTSD can facilitate or impede service-connection award,19,20 a dichotomous variable representing presence or absence of PTSD was included as a distinct comorbidity. A Veteran had diagnosed PTSD in FY2013 if he or she had ICD-9 code ‘309.81’ recorded in the VHA PTF or the VHA OEF on at least two separate occasions during a 24-month window (FY2012-FY2013).21
To better characterise the sample, additional VHA healthcare utilisation measures (not modelled) from FY2013 are presented: Total number of VHA outpatient healthcare visits, a continuous variable derived by summing clinic stop codes (a Veteran could have more than one ambulatory care visit on any given day) was extracted from VHA OEF; total number of VHA inpatient healthcare visits (extracted from VHA PTF) was dichotomised (at least 1 visit/no visit), as only a relatively small proportion of the sample had been hospitalised in 2013. Given our focus on DM and IHD, VHA specialty endocrine care and VHA specialty cardiac care (both extracted from VHA OEF) were also dichotomised (at least 1 visit/no visit). In addition, length of VHA hospitalisation stay in days, a continuous variable, was extracted from the VHA PTF file.
Veteran characteristics in 2013 extracted from VETSNET included combined disability rating percentage, VBA Individual Unemployability award, VBA Special Monthly Compensation award, VBA Ancillary disability benefit award, branch of service and rank. Because we wanted to capture Veterans whose service-connected disabilities entitled them to maximum benefit levels, combined disability rating percentage (0-100%) was transformed into a three-level variable representing subjects with ratings of 0-40%, 50-90% or 100%.
As measures of disability severity, number of service-connected disabilities, number of non-service-connected disabilities and total number of service and non-service-connected disabilities as of April 2013 were included as continuous measures. Further reflecting disability severity, three dichotomous variables represented presence or absence of the following: (1) VBA Individual Unemployability (IU) provides compensation to Veterans who cannot maintain employment due to service-connected disabilities; (2) VBA Special Monthly Compensation (SMC) provides additional compensation for loss/loss of use of an organ or extremity; (3) VBA Special/Ancillary disability benefits provide additional types of compensation to Veterans with particularly severe service-connected conditions.22 A Veteran was considered to have a VBA Special/Ancillary disability benefit if they were receiving a clothing allowance, vocational rehabilitation and employment and/or special adaptive equipment or housing grants. Finally, total monthly VBA disability compensation payment accorded by the above benefits was reported in 2013 US dollars.
Because Veterans who served in the Army or Marines were more likely than those who served in the Navy or Air Force to experience combat,22,23,24 and combat is a correlate of service-connection award status, branch of service at discharge was operationalised as a five-level variable (Army, Marines, Navy, Air Force, all other branches). Additionally, because lower rank at discharge (relative to higher rank) is associated with poorer health and lower socioeconomic status,24,25 both of which are associated with service-connection award status, rank at discharge was operationalised as a three-level categorical variable (Officers, Enlisted or non-commissioned officers, Unknown or missing).
Statistical analysis
The VA-New Jersey Health Care System Institutional Review Board approved this study. All analyses were performed with SAS 9.3 (SAS Corp: Cary, NC), were two-tailed and conducted with α=0.05 significance level.
In analysing descriptive statistics for Veterans with DM or IHD, we compared presumption gap versus no presumption gap for all initial variables. A p value of α < .05 denoted a statistically significant difference between these groups. Descriptive statistics are presented as percentages (categorical variables) or medians and interquartile ranges (continuous variables).
In conducting multivariable analyses, we applied a multi-step approach: First, we conducted bivariate analyses to explore associations between candidate predictors and each outcome. Those predictors that had a bivariate association with an outcome at significance level p<.2526 were retained for the multivariable model. Second, binary logistic regression with forward selection27 was used to model relationships between binary dependent variables and independent variables. Binary logistic regression is a generalised linear model that uses the binomial distribution and a logit link function.28 Model coefficients are estimated by a maximum-likelihood algorithm and exponentiation of the coefficients provides odds ratios for independent variables.28 Third, we examined the contribution of each predictor to the multivariable model using a Wald chi-square test with an adjusted significance level. The Bonferroni stepdown method, which was used to derive the adjusted significance level, is appropriate when several statistical tests are being performed simultaneously on a single dataset.30
Table 1. Characteristics of Vietnam-Theater Veterans with Diabetes or Ischaemic Heart Disease
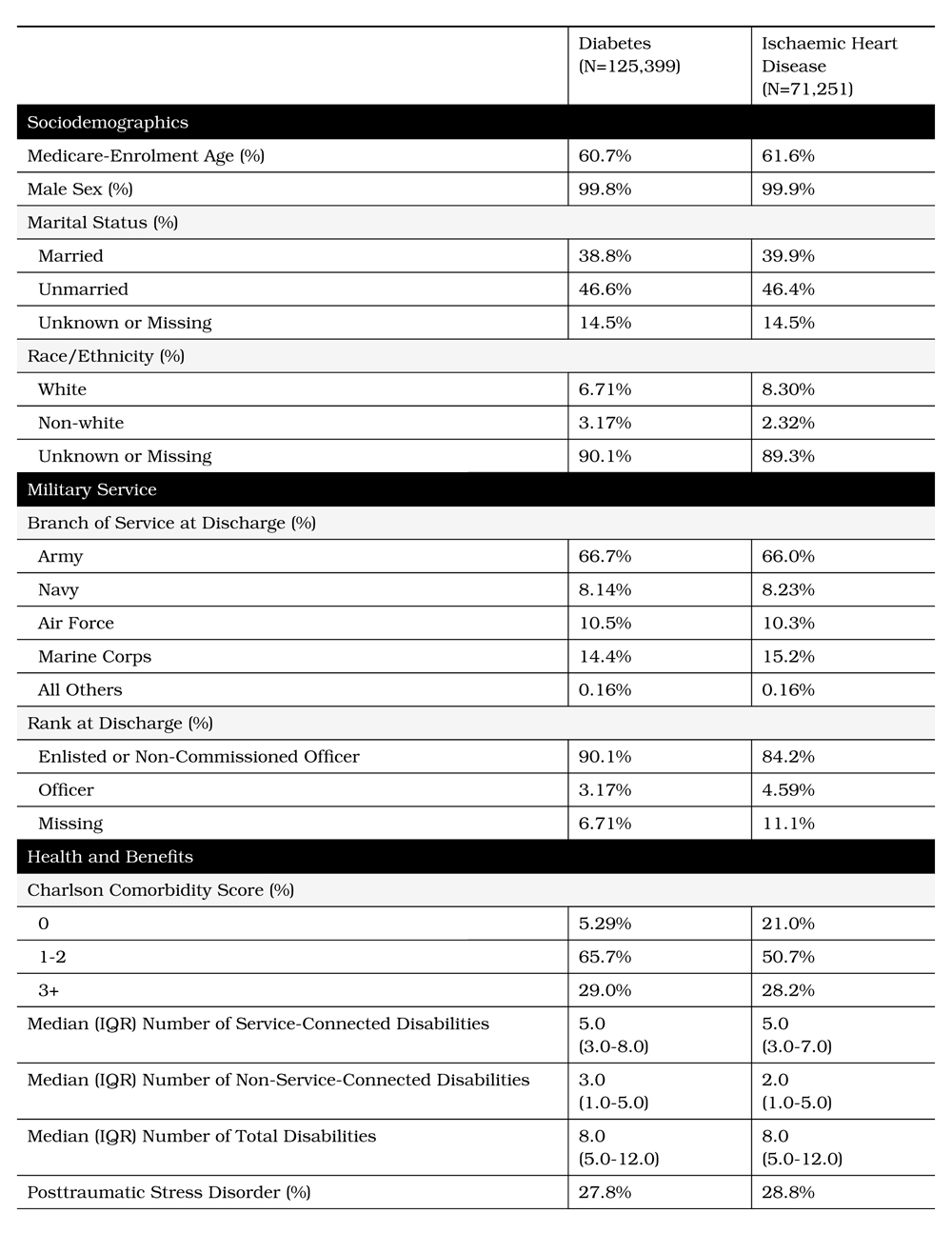
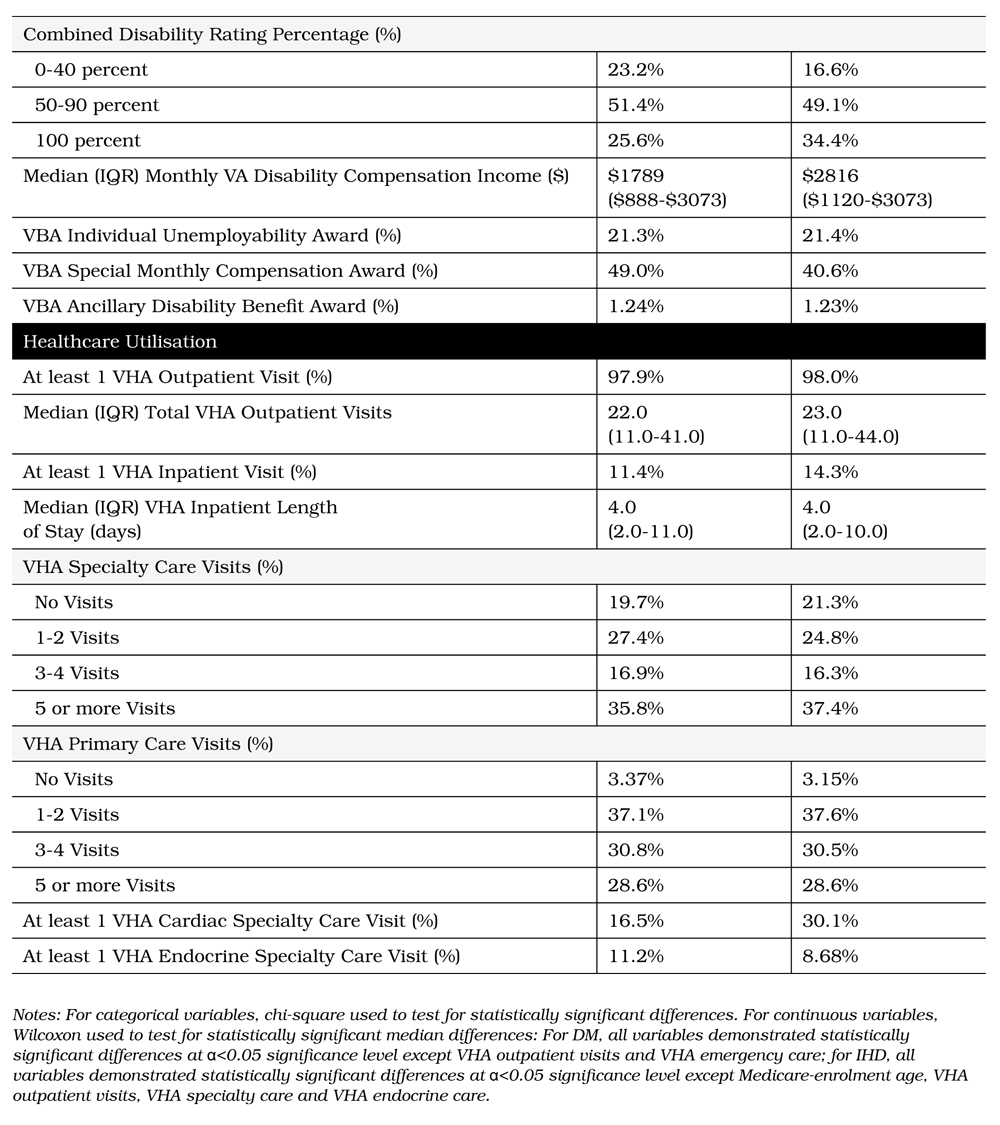
Table 2: Presumed Service-Connected Award Status in 2013 for Vietnam-Theater Veterans with Diabetes or Ischaemic Heart Disease
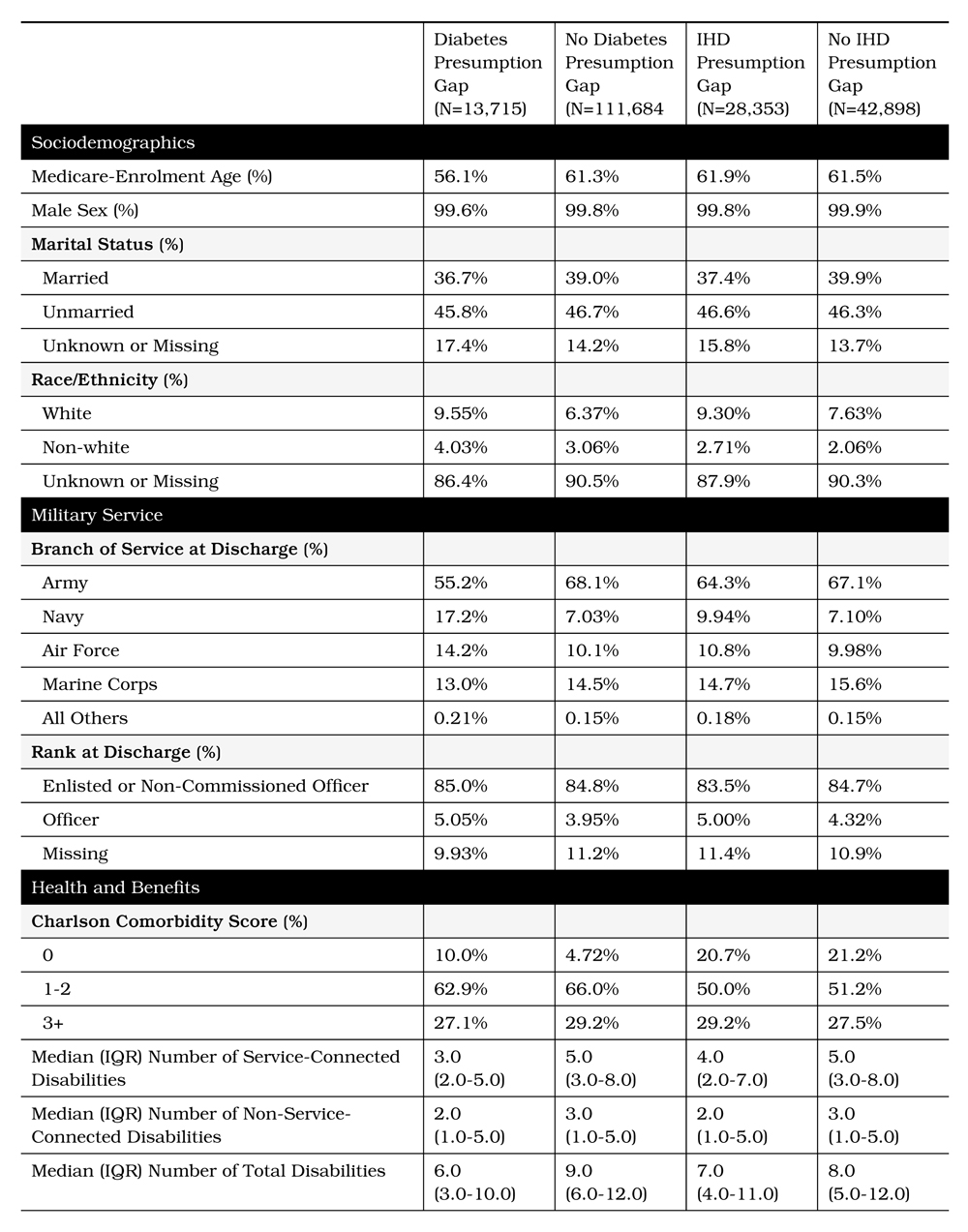
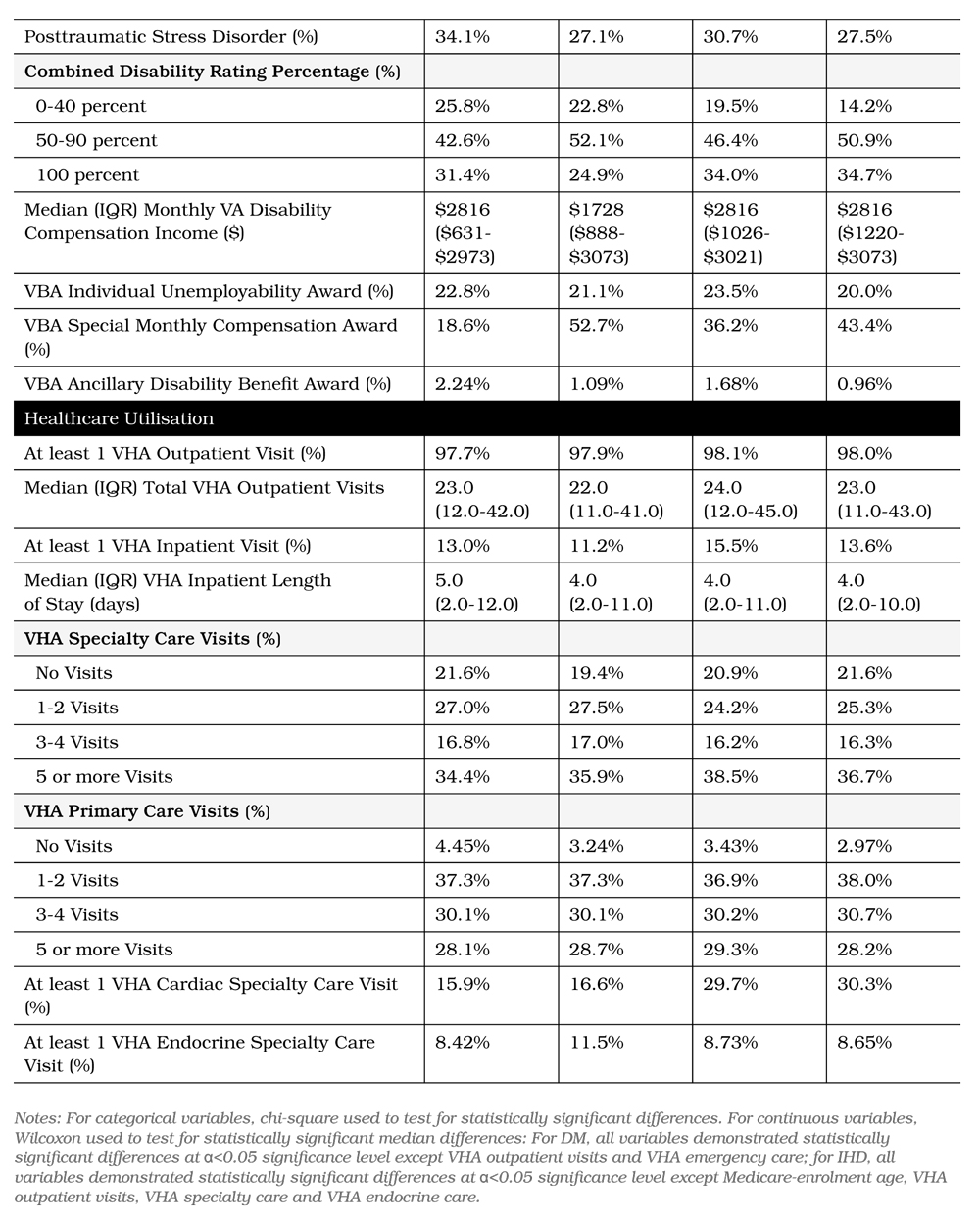
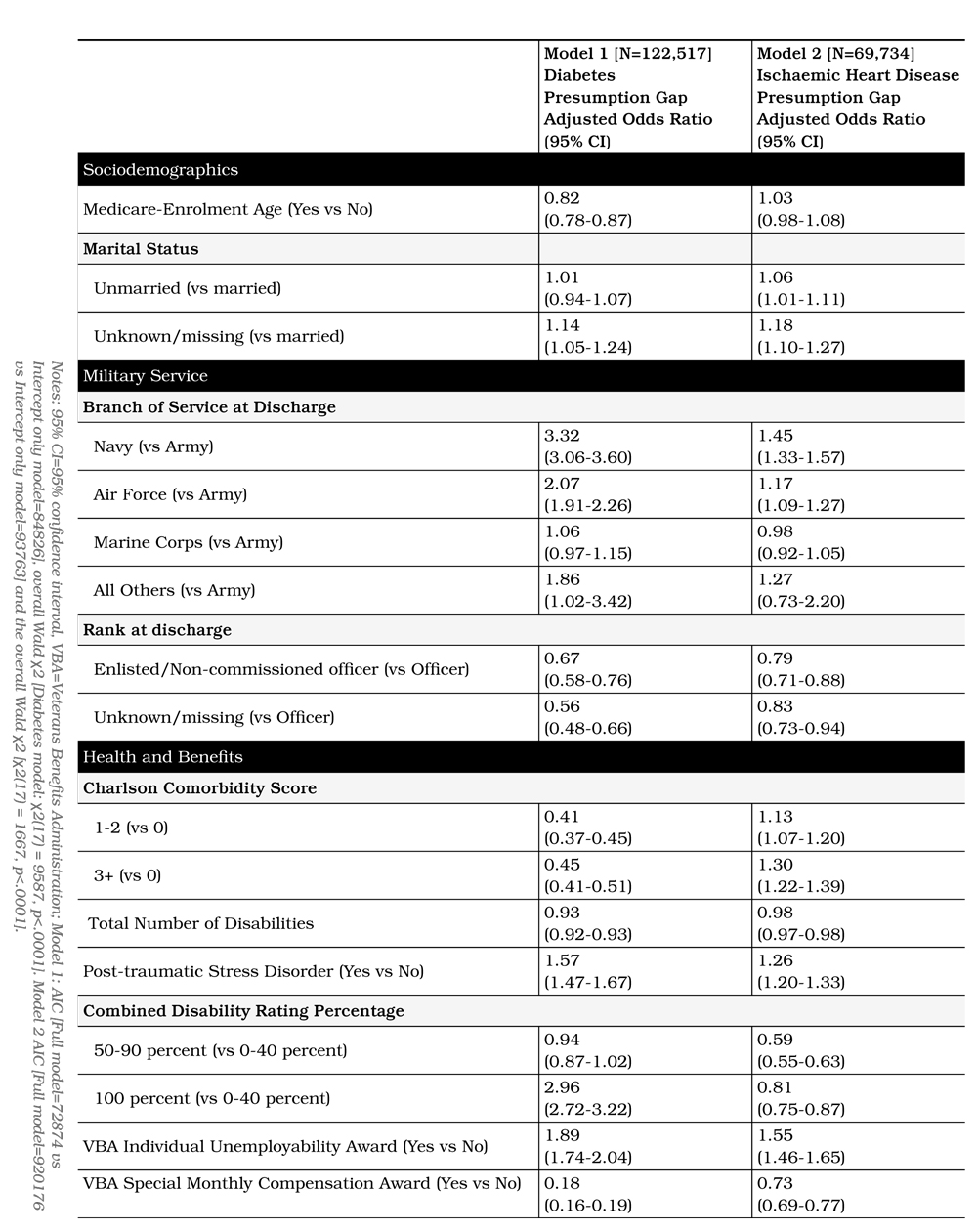
Table 3: Multivariable binary logistic regression modelling of factors associated with diabetes presumption gap (vs no diabetes presumption gap) or ischaemic heart disease presumption gap (vs no ischaemic heart disease presumption gap)
In assessing goodness of model fit, since the HosmerLemeshow goodness of fit test performs poorly for large samples30, goodness of fit was instead assessed with the following: Akaike Information Criterion (AIC) fit statistic was used to compare the full model to the intercept only model (the model with the smallest AIC is considered best).31 Additionally, the Wald χ2 goodness of fit test was used to evaluate overall model fit (p values of α<0.05 significance level indicate satisfactory fit).26 To assess overdispersion, the deviance statistic was divided by its degrees of freedom (the result should be approximately equal to 1 when no lack of fit or overdispersion exists).31,32 As a final indicator of fit, to assess multicollinearity, we generated Variance Inflation Factors (VIF) (VIFs of approximately 1.0 indicate little/no multicollinearity).33 In multivariable modelling, race/ethnicity (83.8% unknown or missing) was excluded due to excessive unknown or missing observations. For all other variables, missing observations were deleted through an automated process of listwise deletion.
Results
Among 196 650 Vietnam Theater Veterans (mostly male) who were VBA and VHA users, 125 399 (43%) had DM and 71 251 (25%) had IHD, in 2013. Among those with diagnosed DM, 13 715 (10.9%) had a DM presumption gap, and 111 864 (89.1%) did not have a DM presumption gap in 2013. Among those with diagnosed IHD, 28 353 (39.7%) had an IHD presumption gap and 43 898 (61.3%) did not have an IHD presumption gap, in 2013 (Table 1).
Unadjusted analysis (Table 2) of Veterans with DM revealed that those with a DM presumption gap (relative to no DM presumption gap) had higher rates of PTSD (DM gap=34.1% vs no DM gap=27.1%), 100% combined disability rating (DM gap=31.4% vs no DM gap=24.9%), and VBA IU award (DM gap=22.8% vs no DM gap=21.1%) and received higher median VBA disability compensation payment (DM gap=US$2 816 vs no DM gap=US$1 728). In contrast, those with a DM presumption gap (relative to no DM presumption gap) were less frequently of Medicare-enrolment age (DM gap=56.1% vs no DM gap=61.3%), had 3+ comorbidities (DM gap=27.1% vs no DM gap=29.2%) and VBA SMC award (DM gap=18.6% vs no DM gap=52.7%). With the exception of endocrine care (DM gap=8.42% vs no DM gap=11.5%), those with and without a DM presumption gap had similar VHA utilisation patterns in FY2013.
The final DM presumption gap multivariable model (Table 3) included Medicare-enrolment age, Charlson comorbidity index score, branch of service, PTSD, combined degree per cent, SMC, IU, marital status, rank and total number of disabilities. After adjusting for covariates (Table 3), DM presumption gap continued to be associated with greater likelihoods of PTSD (OR=1.57, 95% CI: 1.47-1.67), 100% combined disability rating (OR=2.96, 95% CI: 2.72-3.22), VBA IU award (OR=1.89, 95% CI: 1.74-2.04), lower likelihoods of Medicare-enrolment age (OR=0.82, 95% CI: 0.78-0.87), 3+ comorbidities (OR=0.45, 95% CI: 0.41-0.51) and VBA SMC award (OR=0.18, 95% CI: 0.16-0.19).
In terms of fit for the DM presumption-gap model, the AIC [Full model=72874 vs Intercept only model=84826] and the overall Wald χ2 [χ2(17) = 9587, p<.0001] indicated adequate fit (Table 3). As further indication of adequate fit, we found no evidence of overdispersion [Deviance/DF=1.02, p=0.0021] or multicollinearity [VIF≈1.0].
Unadjusted analysis (Table 2) of Veterans with IHD revealed that those with an IHD presumption gap (relative to no IHD presumption gap) more frequently had PTSD (IHD gap=30.7% vs no IHD gap=27.5%), 3+ comorbidities (IHD gap=29.2% vs no IHD gap=27.5%) and VBA IU award (IHD gap=23.5% vs no IHD gap=20.0%). Those with an IHD presumption gap (relative to no IHD presumption gap) less frequently had 100% combined disability rating (IHD gap=34% vs no IHD gap=34.7%) and VBA SMC award (IHD gap=36.2% vs no IHD gap=43.4%). With the exception of inpatient care (IHD gap=15.5% vs no IHD gap=13.6%), those with and without an IHD presumption gap had similar VHA utilisation patterns in FY2013.
The final IHD presumption gap multivariable model (Table 3) included Medicare-enrolment age, Charlson comorbidity index score, branch of service, PTSD, combined degree percent, SMC, IU, marital status, rank and total number of disabilities. After adjusting for covariates (Table 3), similar to DM gap experience, IHD gap was associated with greater likelihoods of PTSD (OR=1.26, 95% CI: 1.20-1.33) and VBA IU award (OR=1.55, 95% CI: 1.46-1.65) and lower likelihoods of VBA SMC award (OR=0.73, 95% CI: 0.69-0.77). In contrast to the DM gap experience, IHD gap was associated with increased likelihood of having 3+ comorbidities (OR=1.30, 95% CI: 1.22-1.39) and lower likelihood of having 100% combined disability rating (OR=0.81, 95% CI: 0.75-0.87).
In terms of fit for the IHD presumption-gap model, the AIC [Full model=92176 vs Intercept only model=93763] and the overall Wald χ2 [χ2(17) = 1667, p<.0001] indicated adequate fit (Table 3). As further indication of adequate fit, we found no evidence of overdispersion [Deviance/DF=1.34, p=0.0021] or multicollinearity [VIF≈1.0].
Discussion
This study found, as hypothesised, a larger presumption gap for IHD (39.7%) than for DM (10.9%) in 2013. This suggests that it may take time for Veterans to become aware of, apply for and be awarded service connection, even for their diagnosed conditions that are presumed related to military service. In 2013, DM had been a designated presumptive condition for 12 years and IHD for only 3 years. This difference in presumption gap size for these two conditions with markedly different time since the policy change (i.e., presumptive designation) is critical in understanding the differences between factors associated with IHD and DM presumption gaps.
Our findings suggest that for some Veterans, chronic comorbid conditions may delay or impede filing of a presumed service-connection claim because impairments may make it difficult to complete the lengthy application, or attend all required evaluations.10 Veterans busy managing multiple chronic health conditions may have less time and opportunity to become aware of, or act on more recent changes in presumptive policy. Among Veterans with IHD, those with an IHD presumption gap had higher comorbidity burden and were much more likely to have diagnosed PTSD, compared to those without an IHD gap, during the study period. While a DM presumption gap was associated with greater prevalence of PTSD, the presence of 3+ comorbidities was associated with a lower likelihood of a presumption gap (in marked contrast to Veterans with IHD). These findings, in suggesting that PTSD may be a common impediment to uptake of presumed service connection in both condition cohorts, are consistent with studies suggesting that mental health conditions may impede receipt of disability benefits, particularly among those with severe mental illness.34,35 While this study did not examine different levels of PTSD severity, subsequent studies might wish to evaluate the role of mental health condition severity level in uptake of presumptive benefits. The difference in the relationship between presumption gap and burden of comorbid conditions most likely reflects the difference in time since the presumptive service-connection policy inception for these two conditions.
Another interesting finding of the study is that the DM presumption gap appeared to be associated with attainment of maximum allowable benefits. Among our sample, those with a DM gap were more likely than those without this gap to have a 100% combined disability rating and to receive VBA IU benefits. Both of these benefit statuses result in monthly disability compensation at the 100% rate. It is worth noting that Veterans with a 100% disability rating receive highest priority VHA care for all service and non-service-connected conditions at no cost; for these Veterans, addition of a presumptive service-connection award for their DM would not alter their access to VHA healthcare services, compensation payment, priority group assignment or co-payments. These Veterans would have little incentive to file a presumptive claim, resulting in a persistent DM presumption gap, as more maximally-rated Veterans develop this age-related chronic condition.
Overall, such extensive use of the VA system is consistent with our contention that while reduced uptake may reflect the inability to acquire benefits for some with very poor health, it may also reflect limited interest in acquiring additional service-connection awards for others who have ‘maxed out’ on their VA benefits. We suspect that a sample of Vietnam Theater Veterans less engaged with the VA benefits system would demonstrate different characteristics in relation to presumption gaps.
Limitations
In this cross-sectional study there is some possibility of misclassification of Vietnam-Theater status, a key characteristic of our population of interest. However, because the theater flag we used from VETSNET is only applied when there is documented evidence of intheater service verified by the VBA, misclassification is likely to be minimal. Also, presumptive service connection has been incrementally expanded to include Veterans deployed to the waters near Vietnam (brown-water Vietnam Veterans), some Veterans deployed to the Republic of Korea, and is currently being considered for US Navy Veterans on ships which transported AO (blue-water Vietnam Veterans). Therefore, our results may not be generalised to these groups. In addition, findings from our own prior studies36,37 lead us to believe that other factors (such as social support, education, literacy and financial means) are likely also associated with the presumption gap for these conditions; our data, however, were inadequate in this study to explore these associations. In addition, since we were only able to examine the presumption-gap status of Veterans with DM or IHD due to VETSNET data limitations, it is possible that factors associated with these disease presumption gaps differ from factors associated with presumption gaps for other presumptive conditions (e.g., prostate cancer). As an additional limitation, this analysis was restricted to VA system users. Given that a majority of Veterans in any given year do not use the VHA, inclusion in our sample of Veterans who were not VA system users might have led to different results. Finally, because this analysis was restricted to living Veterans with DM or IHD, results may be subject to survivor bias.
Conclusion
Service connection is a multibillion dollar annual federal expenditure to the benefit of Veterans. Presumptive service connection is a critical special accommodation to address the challenges of documenting military-related exposures with latent negative health effects. Our findings provide essential, new information about presumed service connection for IHD and DM for Vietnam Veterans and elucidate the relationships among Veteran characteristics, presumed service connection and VA system utilisation.
It appears that it may take several years from presumptive designation to widespread uptake of the benefits. VA may want to consider more aggressive outreach of such policies, especially targeting those with covered conditions diagnosed in VHA. Additionally, because PTSD and the heavy burden of chronic conditions may be a barrier to benefit uptake for some Veterans, VA may consider enhancing outreach and assistance programs focused on this group to increase awareness of service-connected benefits. On the other hand, many Veterans who have already maxed out their VA benefits appear aware that there is limited incentive for seeking additional benefits.
For Veterans and Veteran advocates, our findings offer clues to why presumptive benefits were ‘left on the table’ among Vietnam Veterans who did not file for presumed service connection despite their diagnosis of IHD and DM. For VA policymakers and Veterans Service Organisations, our findings can help shape the resources and approaches needed to accelerate the uptake of disability and healthcare benefits by eligible Veterans.
Corresponding Author: Dennis Fried, Dennis.Fried@va.gov
Authors: D Fried1,2, M Rajan3, C Tseng1, D Helmer1
Author Affiliations:
1 US Department of Veteran Affairs
2 War Related Injury and Illness Study Centre
3 Weill Cornell Medicine
Appendix I. Presumptive conditions (ICD-9 codes) and VHA healthcare categories (clinic stop codes)