B O’Toole, K Pierse, B Friedrich, S Outram, M Dadds, S Catts
Introduction
Australia’s involvement in the Vietnam conflict from 1962 until troop withdrawal in 1972,1 placed Australians into longer periods of risk of contact with an enemy than at any time in Australia’s history since Gallipoli.2 The Australian Force Vietnam increased in size in 1965 and 1966 and, in conjunction with the troop build-up, the Australian Government introduced conscription for overseas service1 to enhance the previous all-volunteer Army to levels that would sustain the campaign. In the early years of the conflict, National Servicemen (NSM) were used sparingly in Vietnam; however, as the conflict continued, they became indispensable to the Australian effort and eventually constituted approximately 48% of the Australian Force Vietnam. Registering at age 18, being balloted at 20, enlisting in the Army and serving until 22 became the destiny of nearly 64 000 young men of whom more than 19 000 served in Vietnam.3
In Australia, the chances of entering the Army after being called up, and medically and psychologically examined, was only of the order of 1 in 16.3; Appendix IX, p 193 Compared with Regular enlistment, conscription inevitably produced a different makeup of the force, often more educated, with higher socioeconomic standing and more stable pre-enlistment occupations.4 Both groups were arguably physically fitter than their non-military peers and presumably with less emotional instability.
Continued enlistment in the military is contingent upon maintenance of physical fitness. Thus, soldiers with longer military careers may be expected to be healthier than others suggesting that, compared with NSM, Regular soldiers might be healthier for the duration of their service than NSM of the same age who are not in service. Alternatively, military life places physical burdens on soldiers that would be more wearing the longer the exposure, although they may have greater access to medical and health services than their non-military peers. The implications of these competing hypotheses are yet to be tested.
Earlier Australian research into the potential health effects of Vietnam Service focused on NSM3-7 recruited solely to the Army. More recently, cancer incidence8 and mortality9 have been examined in the whole Vietnam Veteran population, including the Navy and Air Force, specifically in NSM;10 however, NSM were not compared with Regulars in any of those studies. Therefore, there are gaps in knowledge due to the lack of previous research in Australia, or militaries elsewhere in the world, that has directly examined whether volunteers or conscripts are at a differential risk of ill health in later life and, in particular, whether they differed in combat experiences. Generalising from research on NSM to regular enlistees, or vice versa, is difficult in the absence of comparative empirical data.
Research into the health of Veterans has shown that exposure to combat increases the risk of physical and psychological injury, particularly post-traumatic stress disorder (PTSD).11-15 This disorder was first codified in the American Psychiatric Association Diagnostic and Statistical Manual (DSM) in 1980;16 its prime progenitor in Veterans is combat. The prevalence of PTSD in Australian Vietnam Veterans has been reported as 20-30%.14,15,17 Combat exposure also increases the risk of a number of other physical and psychological conditions in Vietnam Veterans,13-15 in particular heart disease and circulatory disease and arthritis,15 alcohol use disorder, dysthymia and other disorders.14 PTSD itself is associated with a range of physical health conditions.18 Given the varying conditions in Vietnam over the course of the conflict and the increased deployment of NSM, the degree of combat may have been different for Regulars and NSM. If so, this might suggest that NSM would have different risks for PTSD and other physical and psychological disorders known to be associated with combat .Apart from combat, other aspects of service known to increase risk for PTSD include age at first deployment, rank and duration of exposure to the conflict zone.12,16 Differences between NSM and Regulars in these factors may suggest a differential risk of PTSD. However, the competing expectations arising from these considerations are yet to be tested empirically.
This paper reports analysis of data from a cohort study of a random sample of Australian Vietnam Veterans who were assessed 20 and 35 years after homecoming. The physical and mental health status of the whole cohort has been published previously13-15 and compared with national norms.13, 15 This paper now describes the experiences of Australian NSM and Regular enlistees during and after the Vietnam conflict and their socioeconomic, physical health and psychiatric status at two periods up to three decades following the war. We hypothesise that NSM and Regulars have had differential education, military training, service histories, and combat and combat zone exposure and expect that these may be followed by differential health status, including PTSD and other physical and psychological disorders.
Materials and Methods
Veterans were identified from a computer file developed during the Australian ‘Agent Orange’ studies3-5 holding the Army Service numbers of all men who were posted to Vietnam.19 From the total of 57 643 postings, after removing duplicates, a random sample of 1 000 numbers was selected. The Army supplied the name and date of birth of each man for tracing, contact and in-person interview. All Veterans signed formal consent before interview. Interviews occurred across Australia in Wave 1 between July 1990 and February 1993, and in Wave 2 between April 2005 and November 2006.Wave 1 was conducted an average of 21.96 years (SD = 1.91) after first return to Australia; Wave 2 an average of 36.10 years (SD = 1.92) after, with an inter-interview interval average of 14.18 years (SD = 1.92).Deaths were identified from electronic searches of the National Death Index of the Australian Institute of Health and Welfare.20
Interview assessments comprised standardised questionnaire instruments selected to permit direct comparison with national population statistics and administered by trained clinical and research interviewers. In both waves, the study relied on the Australian Bureau of Statistics (ABS) methods used to gather national statistics on the health of the Australian population at approximate corresponding times, which enabled computation of relative prevalences compared with the Australian population.13, 15, 21
The content of the interviews in both waves comprised a physical health interview, a clinical assessment of PTSD and standardised diagnostic assessment of general psychiatric status. Physical health was assessed using the ABS National Health Survey (NHS) for physical health and associated risk factors that were current at the time (the 1989/90 NHS22 in Wave 1 and the 2004/05 NHS23 in Wave 2). Conditions were coded to prevailing ICD-9/10 rubrics. Combat-related PTSD was assessed using the Structured Clinical Interview for DSM-III (SCID)24 in Wave 1 and the Clinician-Administered PTSD Scale for DSM-IV (CAPS)25 in Wave 2.General psychiatric status was assessed using the Diagnostic Interview Schedule (DIS)26 in Wave 1 and the Composite International Diagnostic Interview (CIDI)27 in Wave 2.The version of the CIDI (V2.1) was that used by the ABS in the Australian National Survey of Mental Health and Wellbeing, 1997.28
Prior to Wave 1, fieldwork data were extracted from the Central Army Records and Psychology Corps Records Offices on the cohort. Data included service details (postings, dates, service milestones), conduct and casualty information, pre-enlistment education and employment and the results of Army psychology classification tests.
Combat was assessed from Army records based on the roles that individual units played, as advised by military advisers to previous Australian studies3 of Vietnam Veterans. The Army Combat Index grouped the units that had been present in Vietnam into six, depending on their role, presence on the field and their experience of combat and casualty risk. These were then weighted by the length of time each soldier was posted to each unit, aggregated over all tours, to produce a continuous scaled measure of exposure to combat that was independent of Veterans’ self-report.19
Members of the research team, volunteer counsellors from the Vietnam Veterans Counselling Service (VVCS) or volunteer officers of the Australian Army Psychology Corps conducted interviews with Veteransin Wave 1.In Wave 2, interviews were conducted by author A and independent clinician-counsellors recruited via their then affiliation with the VVCS or the Australian Centre for Military and Veteran Health. Ethics approvals for Wave 1 were obtained from the Human Research Ethics Committees (HRECs) of Sydney and Queensland Universities; for Wave 2 from the HRECs of the Repatriation General Hospital Concord in Sydney, The University of Sydney, The Australian Government Department of Veterans Affairs, and the Australian Institute of Health and Welfare.
Data Analysis
Bivariate statistical tests compared regular soldiers with NSM using χ2 tests for categorical data and t-tests for continuous data. Multivariate logistic regression was used to compute Regular-NSM odds ratios (ORs) in three hierarchical models: Model 1 adjusted for age at interview; Model 2 adjusted for age at interview and Army Combat Index; Model 3 added other potentially important confounding variables that were identified from bivariate analysis of Army data. Statistical analysis used SPSS V14.0;29 two-sided statistical significance was set at α = 0.05.
Results
In Wave 1, 641 Veterans participated, which was 87% of locatable Veterans and 67.5% of those not known to have died (n = 50).In Wave 2, 450 Veterans participated, which was 51.4% of those not known to have died (n = 125) and 79.4% of those who could be located; 391 Veterans participated in both waves. In Wave 1, 309 NSM and 332 Regulars were interviewed (67.6% and 67.5% of surviving NSM and Regulars respectively) and in Wave 2, 209 NSM and 241 Regulars were interviewed (48.6% and 54.2% of surviving NSM and Regulars respectively).There were no differences in response rates between NSM and Regulars at either wave.
Comparing respondents with alive non-respondents using the Army data revealed only two significant items: the (intelligence) test AGC (OR = 1.12, 95%CI: 1.06, 1.18) and having a charge of Absent Without Leave (AWOL) after return to Australia (OR = 1.52, 95%CI: 1.11, 2.09).A similar result was found for Veterans who responded in both waves (AGC: OR = 1.15, 95%CI: 1.09, 1.21; AWOL: OR = 1.93, 95%CI: 1.27, 2.93), indicating that respondents overall were generally more intelligent and more affiliative toward the armed services.
Table 1 shows temporal information on the Veterans: Regulars were born on average during World War II,
five years before NSM and enlisted five years earlier at younger ages. Regulars had fewer years of school before enlistment, were older at first deployment to Vietnam and had longer pre-deployment Army Service. Their first tour was longer, their total duration in Vietnam was longer, and their durations of Army Service after Vietnam and overall were longer than the NSM. There was no difference in their AGC (intelligence test) scores but Regulars scored significantly higher on the Army Combat Index.
There were more Regulars (18.3%) than NSM (8.6%) who had a pre-enlistment ‘criminal record’ (mainly petty crimes; a serious record would preclude enlistment) (OR = 2.37, 95%CI: 1.61,3.50; χ2 = 19.658 (df = 1), P <0.0005) and more NSM (19.6%) than Regulars (8.6%) who had trade training before enlistment (OR = 2.60, 95%CI: 1.75, 3.87; χ2 = 23.432 (df = 2), P < 0.0005).Corps allocation was dissimilar for NSM and Regulars (χ2 = 12.819, df = 4, P = 0.012); NSM were more likely to be in Infantry than Regulars were (OR = 1.40, 95%CI: 1.08, 1.80).Rank in Vietnam also discriminated NSM from Regulars (χ2 = 231.246, df = 4, P <0.0005): only 1.7% of NS were officers, compared with 12.2% of Regulars; no NSM were NCOs compared with 5.3% of Regulars; only 0.2% of NS were Sergeants compared with 15.1% of Regulars; 12.6% of NSM were Corporals compared with 25.8% of Regulars, but 85.5% of NSM were Privates compared with 41.6% of Regulars.
Table 2 shows the proportion deceased, the age at interview, the marital and employment status and incomes of NSM and Regulars. More Regulars were deceased by Wave 2, consistent with their birth cohort. Marital status was not different at either wave. More NSM were employed full-time and fewer were retired at both waves, but their income distributions were similar.
Tables 3-6 show prevalences of health conditions and ORs and 95% confidence intervals from hierarchical logistic regression models adjusted firstly for age, (Model 1), then age and Army Combat Index (Model 2), then age, Army Combat Index, plus an additional set of potential confounders. This strategy was chosen because age is an obvious confounder for health conditions and adding combat allows the comparison between NSM and Regulars to take into account different combat exposures and tests the effect of combat on each endpoint adjusted for age. The potential confounding variables comprised birth cohort (year of birth), age at deployment, durations of Army Service before, during, post-Vietnam and total, and rank in Vietnam.
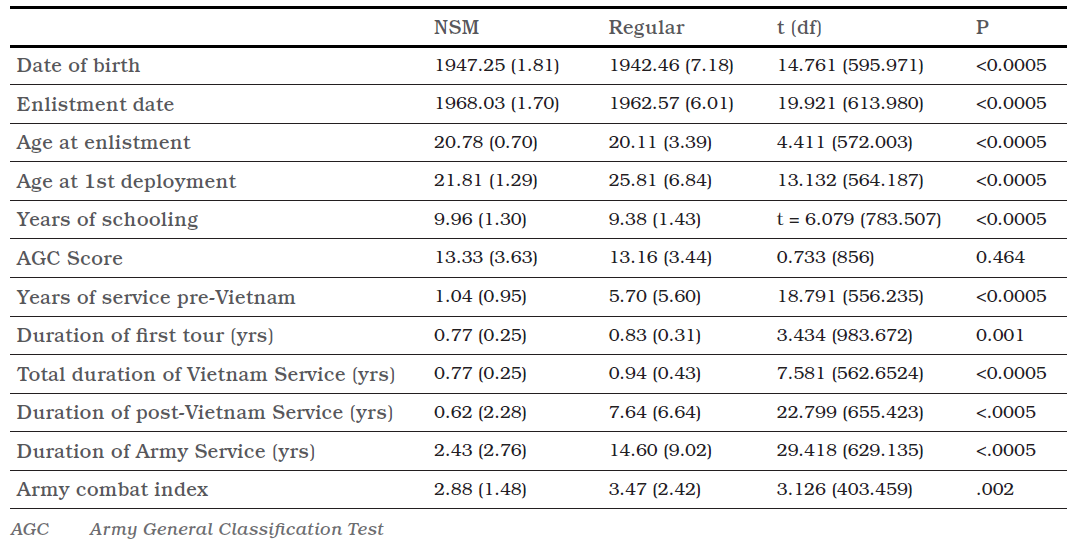
Table 1. Means and Standard Deviations (in Parentheses) for Continuous Data From Army Records for Australian National Servicemen (NSM) (n = 309) and Regular Enlisted (n = 332) Vietnam Veterans, and t-statistics, degrees of freedom (in Parentheses) and statistical significance for t-tests comparing the two groups.
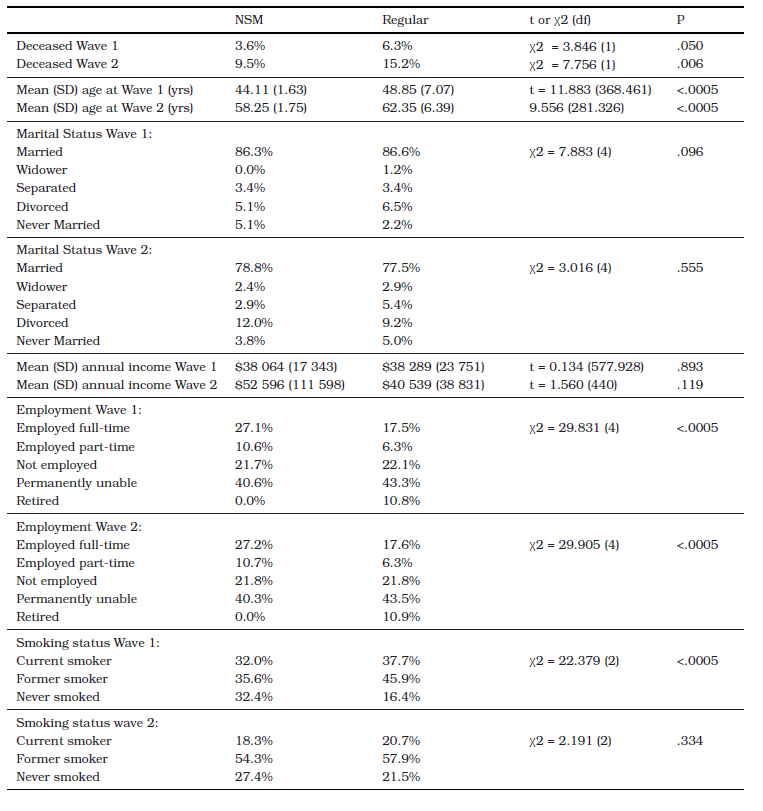
Table 2. Demographic Characteristics of Australian NSM and Regular Enlisted Vietnam Veterans at Wave 1 (July 1990 – February 1993; n = 309 and 332 respectively) and Wave 2 (April 2005 – November 2006; n = 209 and 241 respectively) and Statistical Tests (t-statistics or Chi Square) and P-values for tests comparing the two groups.
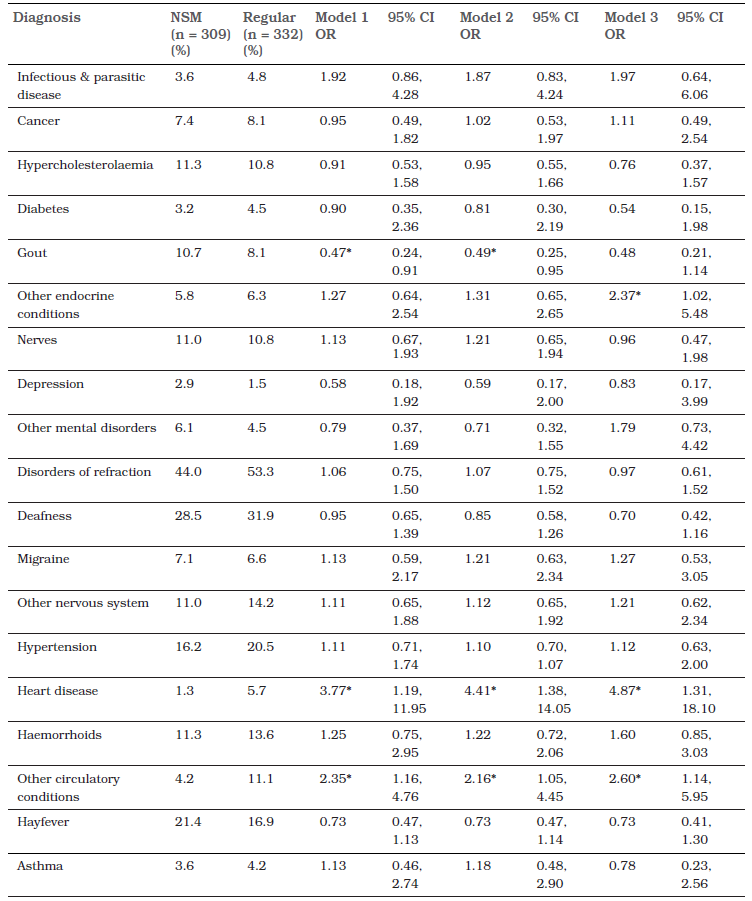
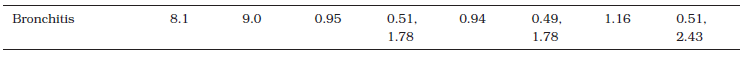
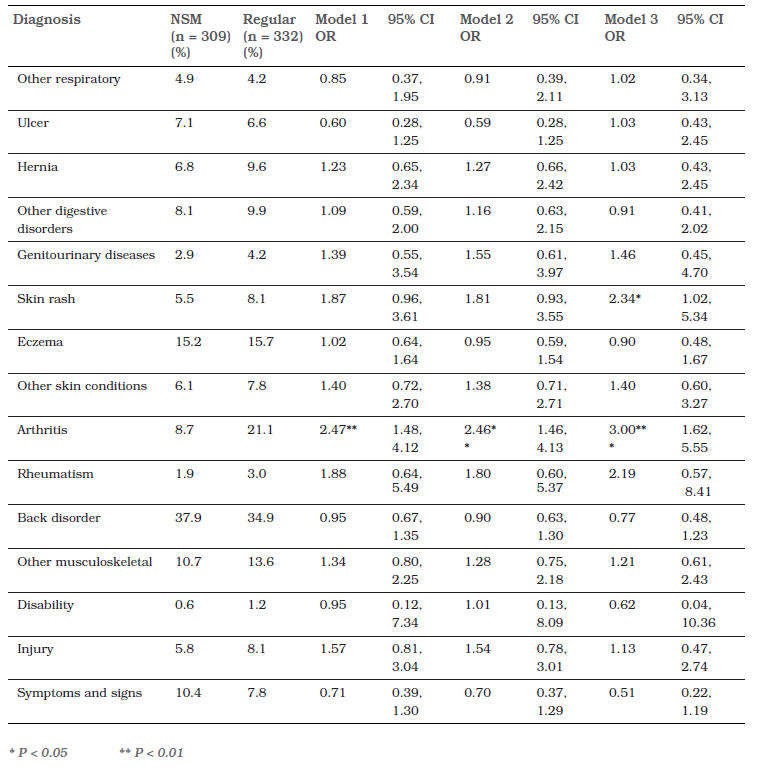
Table 3. Prevalence of ICD-9 Chronic Physical Health Conditions in Wave 1 and Logistic Regression-Modelled Odds Ratios (ORs) and 95% Confidence Intervals (CIs) Comparing Australian Vietnam Veteran Regular Enlistees with NSM; Model 1 adjusted for age, Model 2 adjusted for age and combat, Model 3 adjusted for age, combat, date of birth, age at deployment, durations of Army Service before, during, and post-Vietnam, and rank in Vietnam.
Table 4. Prevalence of ICD-10 conditions in Wave 1 and ORs and 95% CIs Comparing NSM with Regular Enlistees; Model 1 adjusted for age, Model 2 adjusted for age and combat, Model 3 adjusted for age, combat, date of birth, age at deployment, durations of Army Service before, during and post-Vietnam, and rank in Vietnam.
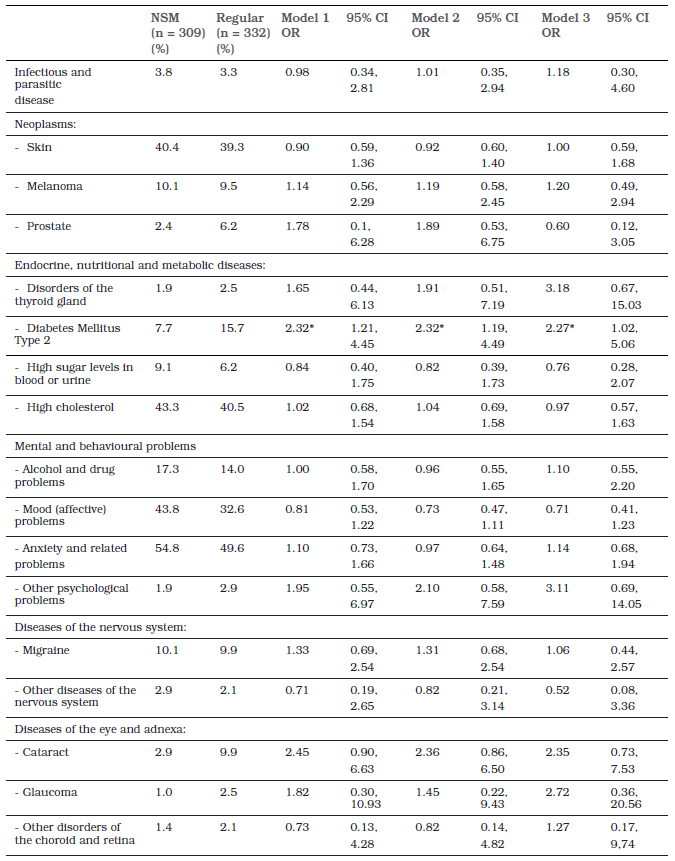
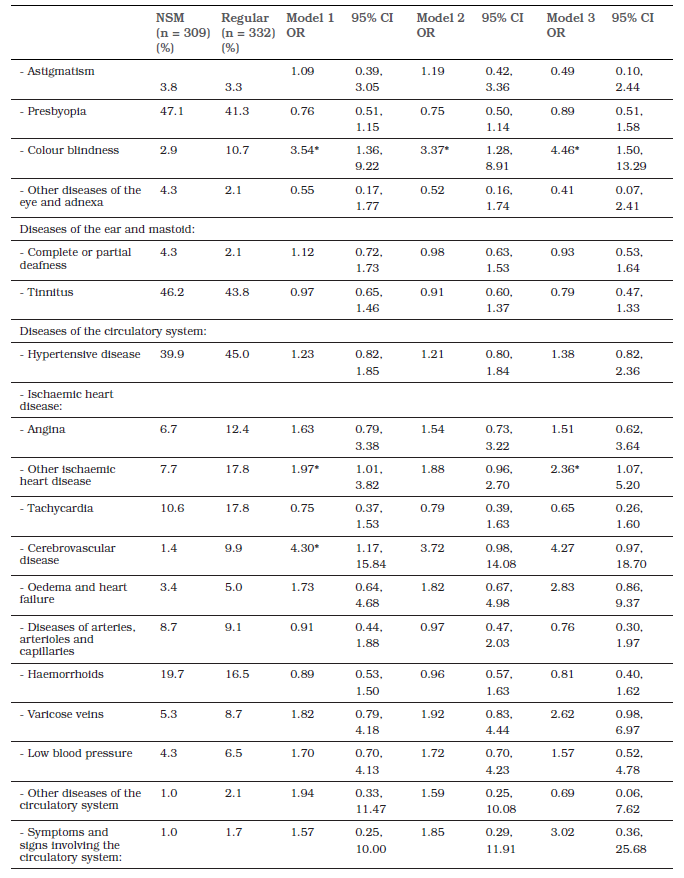
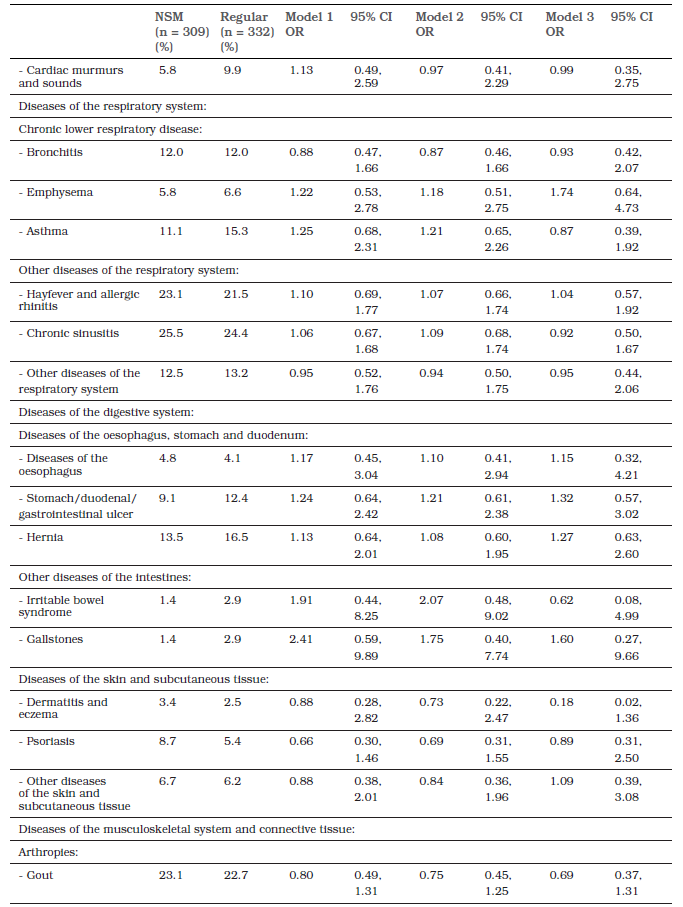
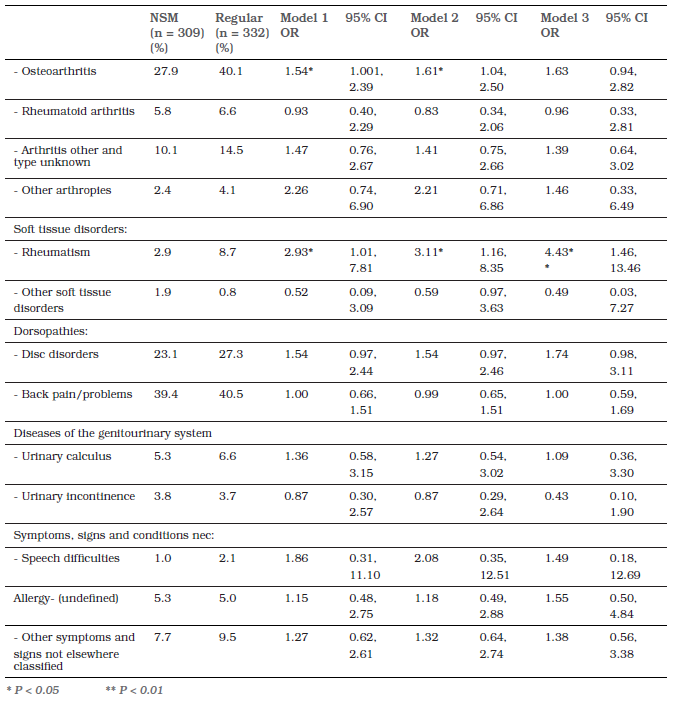
Table 5. Prevalence of DSM-III-R conditions in Wave 1 and ORs and 95% CIs Comparing NSM with Regular Enlistees; Model 1 adjusted for age, Model 2 adjusted for age and combat, Model 3 adjusted for age, combat, date of birth, age at deployment, durations of Army Service before, during and post-Vietnam, and rank in Vietnam.
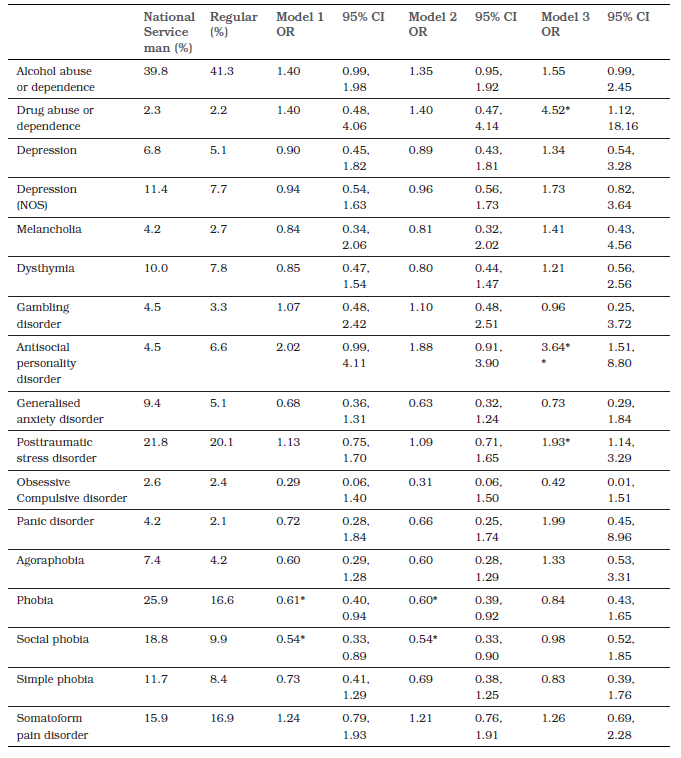
Table 6. Prevalence of DSM-IV lifetime Conditions in Wave 2 and ORs and 95% CIs Comparing NSM with Regular Enlistees; Model 1 adjusted for age, Model 2 adjusted for age and combat, Model 3 adjusted for age, combat, date of birth, age at deployment, durations of Army Service before, during and post-Vietnam, and rank in Vietnam.
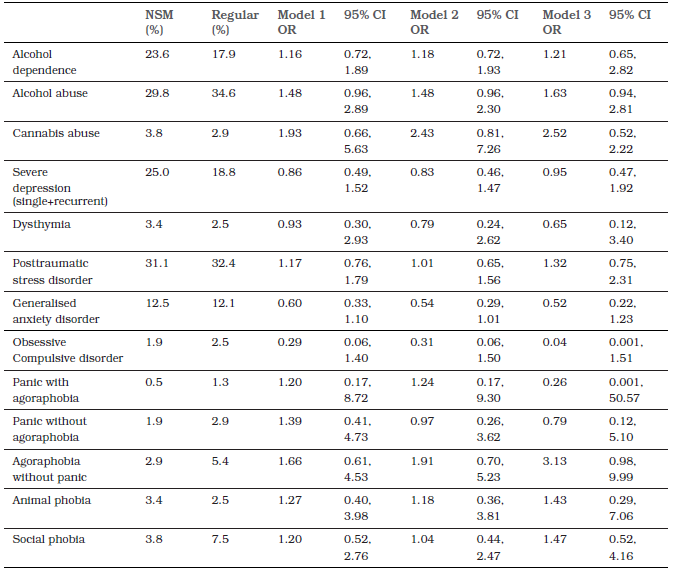
Table 3 shows the prevalence of ICD-9 long term or chronic physical health conditions assessed in Wave 1.Gout was significantly less prevalent among Regulars in Models 1 and 2, but not when the other variables were controlled for. Endocrine conditions became significant only after full adjustment .Heart disease, circulatory conditions and arthritis were more prevalent among Regulars in all models. Apart from these, no other condition discriminated NSM from Regulars.
Table 4 shows the prevalence of ICD-10 physical health conditions assessed at Wave 2.Type 2 diabetes was more prevalent among Regulars in all models; ischaemic heart disease also in Models 1 and 3; cerebrovascular disease in Model 1 only; osteoarthritis in Models 1 and 2; and rheumatism in all models. Otherwise, no other conditions discriminated NSM from Regulars.
Table 5 shows the Wave 1 DSM-III diagnoses. Drug abuse or dependence and antisocial personality disorder were significant only in Model 3.On the other hand, phobia and social phobia were significant only in Models 1 and 2.PTSD risk was not different in Models 1 and 2, indicating that PTSD rates were similar even after adjusting for combat exposure. However, in Model 3, Regulars assumed a significant risk over NSM. Thus, after adjusting for the longer periods spent in the Army before, during and after deployment, and for later age at deployment and higher rank, PTSD risk was significantly elevated in Regulars compared with NSM.
However, PTSD has been reported to shorten military careers,30 so that reduced Army Service post-Vietnam may be a marker of PTSD rather than a confounder and adjusting for it may represent over-adjustment. There was no difference in length of service after repatriation for NSM with or without PTSD (M = 0.58 yrs, SD = 2.45 for NSM with no PTSD and M = 0.33 yrs, SD = 0.38 for NSM with PTSD at Wave 1; t276.047 =1.511, p = .132), but Regulars with PTSD had significantly shorter service than Regulars without PTSD (M = 8.96yrs, SD = 7.00 for Regulars with no PTSD and M = 6.42yrs, SD = 6.58 for Regulars with PTSD; t105.259 = 2.77, p = .007).When the modelling was repeated with post-Vietnam Service duration removed, the NSM-Regular odds ratio was reduced to insignificance (OR = 1.64, 95%CI = 0.89, 3.01; p = .112).
When post-Vietnam Service was removed from Model 3 for other significant outcomes of drug abuse and dependence, phobia, social phobia and antisocial personality disorder, the differences between NSM and Regulars were also no longer significant for drugabuse and dependence (OR = 2.17, 95%CI = 0.59, 8.02; p = 0.247), for phobia (OR = 0.71, 95%CI = 0.44, 1.15; p = .177), or for social phobia (OR = 0.68, 95%CI = 0.38, 1.20; p = .183), but antisocial personality disorder remained significant (OR = 2.59, 95% CI = 1.13, 5.92; p = .025).We can therefore conclude that longer service in the Army after repatriation is associated with decreased risk of these conditions, in addition to PTSD.
Table 6 shows the prevalence of DSM-IV psychiatric conditions assessed in Wave 2 did not differ statistically between NSM and Regulars in any model. NSM and Regulars did not differ in the number of diagnoses and there was no difference in PTSD rates between NSM and Regulars in Wave 2 in any model.
Discussion
It is well known that participation in war, particularly combat, has demonstrable consequences on the physical and mental health of former warriors. The question of whether this is borne equally by volunteers and conscripts has not previously been addressed. The overall results suggest little difference between men who enlisted voluntarily and those who were conscripted in terms of economic, marital, physical and psychiatric health two and three decades after return. Previous findings from this cohort indicate that combat was a risk factor for arthritis and heart and circulatory disease,15 osteoarthritis, angina and cerebrovascular disease,13 and disc disorders and joint injuries were associated with durations of service pre- and post-Vietnam. Given that Regulars saw more combat and spent more time in the Army, their risk of these conditions should be expected to be higher. In the Wave 2 cohort results, Regular enlistment and duration of post-Vietnam Service were associated with osteoarthritis in regression prediction models; these results are confirmed here. It is also likely that military service carries an increased burden of cardiovascular disease and musculoskeletal problems in later life.
Demographically, the differences at interviews included age and employment status but not marital status or annual income. Notable is the lack of difference in economic circumstances, since the higher educational attainments of NSM and briefer military careers would suggest that NSM might have had better career prospects that translated into higher incomes. The pattern of health risk factors also differed between the groups. Regulars had less education and trade training before enlistment, they saw more combat and spent longer in the war zone, all of which should increase their risk in particular of PTSD compared with NSM. In contrast, Regularshad more Army experience before deployment, were deployed at older ages and at higher ranks, and were less likely to be posted to Infantry Battalions, all of which would be expected to reduce their risk of PTSD compared with NSM. While these patterns of risk factors varied between the groups, the rates of PTSD did not. This suggests that the lower risk of PTSD conferred by longer training, older age at deployment and higher rank is counterbalanced by a higher risk from combat and length of deployment in Regulars. Conversely, in NSM the lower risk of PTSD conferred by advantages of higher education, shorter exposure to the conflict zone and lower combat seem to be countered by higher risk conferred by shorter training and deployment to Infantry. If these two opposed forces balance each other to provide equality with the increased risk of PTSD borne by the Regulars due to their higher combat and exposure to the conflict zone, then this suggests that NSM may have been more vulnerable to PTSD, in spite of having seen less combat.
An interesting finding was the reduction to insignificance of the ORs for several conditions after removing one of the potential confounders, duration of service post-repatriation. Drug abuse and dependence, phobia and social phobia were rendered non-significant, while antisocial personality disorder maintained significance. It is possible that this latter disorder is predictive of a preference for serving in the armed services, compared with randomly selected young men from the general population. It is also possible that differential screening and selection imperatives during recruitment of NSM and Regulars acted to reduce the prevalence in NSM. It also suggests that length of service is a significant confounder of the NSM-Regular comparison.
The study here is not without weaknesses. Response rates were not perfect, and the two waves produced slightly different samples at each wave. Thus, between-wave differences may be due to slightly different samples. Secondly, a large number of statistical tests were conducted, of which 5% could be expected to be significant by chance. However, the pattern of results is cogent and points to consistency of findings between the waves. However, some differences may have been missed due to small sample sizes; a number of lower confidence intervals bordered 1.0 and narrower confidence bands from larger samples may have led to 95% CIs that did not contain 1.0.
In conclusion, compared to volunteers, differential advantages of conscripts did not improve their post-discharge socioeconomic status, nor protect them from adverse mental health outcomes post-discharge. PTSD may have been borne disproportionally by Regulars at Wave 1 but this differential dissipated over time. In addition, the similar rates of PTSD in NSM and Regulars may hide a vulnerability conferred by shorter training and Infantry Service among NSM. The notion that Army Service is overtaxing on the body and may raise the risk of cardiovascular and musculoskeletal disease the longer it continues is supported. Otherwise, there appear to be very few overall differences in health between National Service and Regular Vietnam Veterans in later life.
Corresponding Author: Brian O’Toole, brian.otoole@sydney.edu.au Authors: B O’Toole1, K Pierse2, B Friedrich 1,6, S Outram 3,4, M Dadds 1, S Catts 1,5 Author Affiliations:
1 University of Sydney, Brain and Mind Centre,
2 ANZAC Research Institute,
3 University of Newcastle School of Medicine and Public Health
4 Health Behaviour Sciences
5 University of Queensland, Psychiatry
6 Research Department of Epidemiology & Public Health, University College London






