Abstract
Acute schistosomiasis is rarely of military concern, but epidemics have disrupted tropical operations. Acute schistosomiasis is particularly challenging to diagnose because it presents as a non-specific febrile disease, often with an urticarial rash before parasites appear in the stool. US Army combat engineers were infected during bridge construction on Leyte in the invasion of the Philippines, requiring mass evacuation to the USA (n=1300) in 1945. An entire RAAF airfield construction squadron became ineffective, with a 40% infection rate from 16 days of exposure around the Bislig River on Leyte. The Chinese People’s Liberation Army’s planned invasion of Taiwan was indefinitely delayed when 38% of the infantry assault force became acutely infected with Schistosoma japonica following amphibious training in the Yangtze River delta. In febrile epidemic situations, great diagnostic efforts are often required to determine the prevention and prognosis for affected units to reassure soldiers against rumour and disinformation.
Keywords: acute schistosomiasis, South China Sea, disease casualties
The importance of full medical intelligence of newly entered tropical areas is obvious from this outbreak, also the need for certainty of pure water supplies.1
This tiny worm defied even the greatest physicians!; Hundreds of villages choked with weeds. Men wasted away. Mao Zedong2
Schistosomiasis is a trematode (fluke) infection with a complex life cycle involving snails and skin-penetrating parasites. It rarely impacts military operations, but it was familiar to the ANZACs of the First World War in Egypt because of the haematuria caused by Schistosoma haematobium after swimming in the Nile River.1 Acute schistosomiasis or Katayama Fever is a relatively rare syndrome occurring soon after exposure to contaminated fresh water and is primarily observed in modern adventure tourists in Sub-Saharan Africa.3 Symptoms include nocturnal fever, cough, myalgia, headache and abdominal tenderness from the migrating parasites following skin penetration. It is often difficult to diagnose as the symptoms predate finding parasites in the urine or stool and may depend on a high index of suspicion based on an exact travel history with freshwater exposures. Although great progress to eliminate schistosomiasis has been made recently, it still exists in parts of South-East Asia and China particularly in isolated rural river valleys.4,5 Historical aspects of schistosomiasis in military populations are reviewed to give perspective to this tropical disease that military physicians are unlikely to encounter except during operations in poorly sanitised rural areas in the Indo-Pacific Region.
The schistosomes native to Southeast Asia are usually speciated as Schistosoma japonica, which generally produces more eggs and acute symptoms than S mansoni or S haematobium, usually found in Africa and Latin America.6 Parasite eggs excreted in the stool or urine hatch in water to form miracidia, infecting freshwater snails as the intermediate host. Free-swimming cercaria from sporocyst rupture in the snails can penetrate the skin of humans, which completes the parasite’s life cycle. Poorly sanitised rural areas where people occupationally contact fresh water, such as rice farmers and fishermen, are typical of remaining foci of schistosomiasis. Mass chemotherapy with modern oral drugs such as praziquantel has greatly reduced the disease burden in many places but schistosomiasis remains a zoonosis in some parts of China and Southeast Asia.4,7,8
The US military of the Second World War had little experience with schistosomiasis even with its colonial history in the Philippines. An outbreak of Schistosoma japonica in late 1944 was unexpected and remained largely geographically limited to Leyte despite the eventual capture of all the Philippine Islands by the US military. Combat engineers engaged in bridge building/repair were particularly affected, but the common exposure was freshwater contact in areas regardless of the type of military personnel involved. Attack rates included up to most engineer companies but were usually in the 10–20% range. Screening of whole units often found asymptomatic cases, creating a dilemma in handling highly infected groups.9 Due to the potentially toxic nature of the then-current therapy (antimony injections) and the public health aspects requiring long follow-up periods, the US Army Surgeon General ordered known cases (n=1300) of schistosomiasis to be evacuated to two specialist tropical disease hospitals in the USA for evaluation.9 Most soldiers were not acutely ill in the USA, and the antimony treatments were better tolerated than expected.10 Three months was the usual period to determine relapses, defined by the reappearance of ova in stools. A majority of those medically evacuated were only mildly ill, and only a few deaths (n=2) occurred due to neurological complications.11 Although there were some concerns, particularly that prisoners of war might become public health risks of re-establishing infectious foci of schistosomiasis outside of the Philippines (e.g. Hawaii), this did not occur.9
Similar events occurred in one Australian military unit, the Number 3 Airfield Construction Squadron RAAF (Figure 1). This squadron was on Leyte for only 16 days, staging for its onward movement to Mindoro; however, almost all of the infections were traced to freshwater contact in the Bislig River in Leyte1 (Figure 2). The epidemic of febrile disease with arthralgia and urticaria starting two weeks later on Mindoro was originally thought to be sand-fly fever but was eventually recognised as Katamaya Fever from schistosomiasis once parasite eggs were found in stools.1 The entire squadron was eventually repatriated for evaluation in Australia, where 226/565 (40%) airmen were found to be infected with schistosomiasis.12 Most of the men were asymptomatic, but >100 continued to excrete schistosome eggs for up to a year. Treatment with injectable antimony appeared only loosely connected to any clinical outcome.12 Eosinophilia was a useful laboratory marker that persisted even after one year. The major outcome of the Allies encountering schistosomiasis in Leyte was the removal of a few highly infected units (50th US Army Combat Engineers, RAAF No 3 Airfield Construction Squadron) from theatre for public health purposes due to difficulties in treatment and diagnosis.1,9

Figure 1: No 3 Airfield Construction Squadron RAAF was one of the few Australian units involved in the invasion of the Philippines. In December 1944, they landed briefly (16 days) on Leyte where they encountered schistosomiasis before moving on to Mindoro. Australian War Memorial (AWM) photo HOB/56/0661/MC, now in the public domain.

Figure 2: Nearly 40% of the men in No 3 Airfield Construction Squadron RAAF were acutely infected with Schistosoma japonica during water contact on Leyte, similar to that shown in AWM photo OG1830, now in the public domain.
Katayama Fever demonstrated an important political impact in 1949 when it delayed and then removed the threat of invasion of Taiwan by the Chinese People’s Liberation Army (PLA).2 The Nationalist Republic of China Army had lost the civil war with the PLA in 1949 and had largely retreated to offshore islands, including Taiwan and Hainan. A PLA field army near Shanghai was designated for amphibious training to capture Taiwan, which involved teaching thousands of soldiers to swim since no specialised landing craft existed to take them directly to the invasion beaches 180 km across the Formosa Strait.13 The risk of Schistosoma japonica in the coastal waters of the Yangtze River delta was unappreciated. It resulted in a large outbreak of Katayama Fever involving at least 38% of the invasion force (n=37 000). This delayed the invasion plans by at least six months, by which time the Korean War had started, and the US Navy’s 7th Fleet had deployed to deny PLA access to the waters around Taiwan.13 The PLA eventually captured Hainan Island in 1950, only 30 km from the mainland; however, it was unable to manage an amphibious assault on Taiwan due to delays forced by schistosomiasis (Figure 3). Schistosoma japonica thus became the ‘fluke’ that saved Taiwan.14 Schistosomiasis remains endemic to some of the impoverished sections of China primarily because of the zoonotic nature of the disease and difficulties in removing animal reservoirs. Ironically the schistosomiasis on Taiwan is animal-adapted, such that little, if any, human disease has ever existed on the island.7
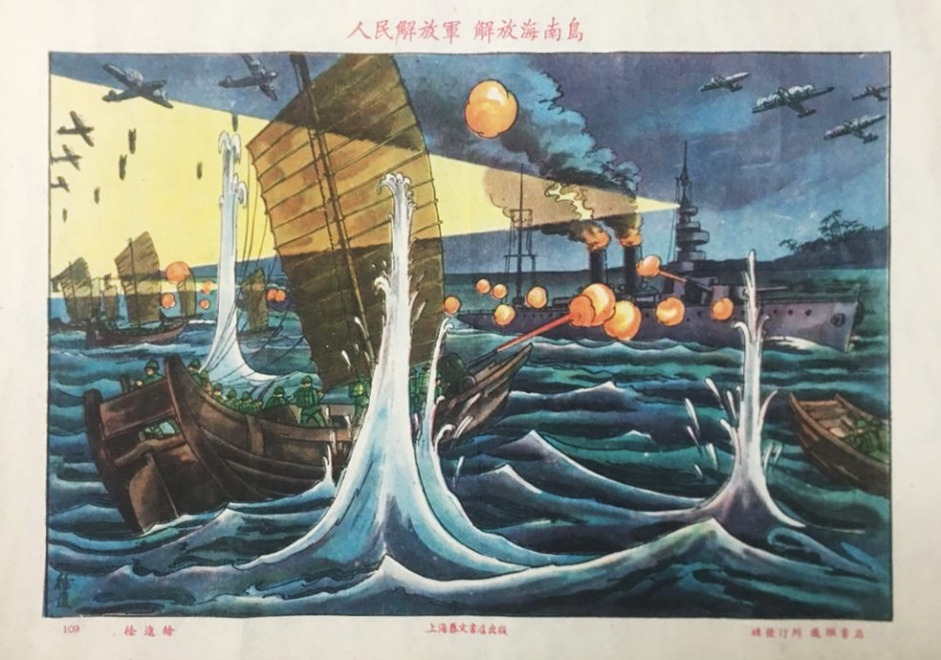
Figure 3: Chinese propaganda poster showing the 1950 liberation of the island of Hainan in southern China, which was supposed to have been the model for the similar invasion of Taiwan, which Katayama Fever disrupted due to Schistosoma japonica. Note the Chinese People’s Liberation Army forces using wooden junks fighting against the Republic of China’s steel naval ships. From http://www.commonprogram.science/poster.html#images2-37
The Australian Defence Force has no current intention of deploying into areas with known foci of schistosomiasis, but that was also true during World War II. The challenge for medical planners is anticipating what exotic tropical infections might become necessary in our Indo-Pacific Region without becoming paralysed by fear of footnotes in a tropical medicine textbook. History is a reasonable screen for risk; if it happened once, it could happen again is the rough logic one can apply to what is recorded in the Official Medical Histories of the War.1 The infectious agents proven to disrupt military operations include malaria, dengue, scrub typhus, influenza and diarrhoeal disease, with minor contributions from filariasis and schistosomiasis. More than the geography, however, it depends on what soldiers are doing in the area. Very few Allied soldiers on Leyte got schistosomiasis in 1944 unless they were swimming in fresh water contaminated by snails. Such a nuanced and thoughtful approach to disease epidemiology will be needed in future campaigns, especially given the near certainty of dealing with internet-generated disinformation from any outbreak of non-specific illnesses.
Funding: No specific funding was given for this work.
Disclaimer: The opinions expressed are those of the author and do not necessarily reflect those of the Australian Defence Force or the US Department of Defence.
Conflicts of interest: The author does not claim any conflicts of interest.
Corresponding Author: G Dennis Shanks, Dennis.Shanks@defence.gov.au
Authors: G D Shanks1,2
Author Affiliations:
1 ADF Malaria and Infectious Disease Institute
2 University of Queensland – School of Public Health






