H Ighani, E Lawrence-Wood, SJ Neuhaus, A McFarlane
Abstract
Current international literature suggests a higher prevalence of respiratory conditions in military personnel during and following deployment to the Middle East for reasons that are not well understood. Therefore, a systematic review of research into the impacts of deployment on respiratory function among international and Australian contemporary military Veterans was undertaken.
The findings from this review suggest that deployment-related environmental, psychological trauma exposures and other military factors such as physical activity, increased tobacco use and individual susceptibility markers could contribute to respiratory conditions and other health effects not yet identified.
Key words: respiratory conditions, Middle East, military veterans, deployment, risk factors, exposure
Introduction
During the last decade, over 2.5 million United States (US) and coalition troops have deployed to Iraq and Afghanistan.1-3 In addition to combat injuries, late health effects of operational service are well recognised 4, particularly psychological and physical effects of deployment exposures. There is also increasing evidence suggesting a higher prevalence of respiratory conditions among international military personnel deployed to the Middle East Area of Operations (MEAO).5-7 Although no specific risk factors other than deployment have been definitively linked to these respiratory health outcomes, there are many characteristics of deployment that may raise the risk of adverse respiratory health effects, including exposure to various airborne contaminants, burn pits, dust, particulate matter, industrial fires and traumatic exposure.5, 6 In addition, evidence suggests tobacco smoking, physical activities and other individual susceptibility factors such as age, sex, body mass index (BMI), blood pressure, physical fitness, pre-existing conditions and personal characteristics may also increase the risk of respiratory symptoms and may enhance susceptibility to environmental exposures.8-11
Although many studies have reported increases in respiratory conditions and symptoms among military personnel, existing knowledge regarding underlying aetiology is yet to be fully clarified. Therefore, a systematic review of research into the impacts of deployment on respiratory function among contemporary military Veterans of deployments to the MEAO was undertaken. The aim of this review was to examine the evidence regarding specific exposures and risk factors in the deployment environment that could be associated with respiratory symptoms and illnesses among military Veterans, and to ascertain whether there are unique risk factors and manifestations of respiratory health among deployed personnel. In this review, we summarise the existing published research related to the respiratory health of military personnel deployed to Iraq and Afghanistan and examine evidence regarding associations between various deployment and other factors, and respiratory health. To provide context for the review, we first describe key respiratory health outcomes and potential exposures relevant to the military and deployed environment, and how these could be associated with respiratory health of MEAO deployed Service members. Following this, the available evidence regarding the association between military deployment risk factors and respiratory health will be reviewed.
Methods
A systematic literature search of library databases was undertaken in May 2016, including, Embase, PubMed and Scopus. Emtree and MeSH Indexing languages were used in Embase and PubMed databases respectively (there is no indexing language available for Scopus).The following keywords were searched in titles, abstracts and texts: respiratory, respiratory tract diseases, lung disease, acute lung injuries, lung function test, respiratory function, veterans, veteran’s health, military, military personnel, defence, deployment, armed conflicts, Afghan campaign 2001, Operation Enduring Freedom (OEF), Iraq wars 2003-2011,Operation Iraqi Freedom (OIF), air pollutants, environmental exposure, inhalational exposure, air environmental pollutant, combat disorder, trauma and stressor related disorder, and tobacco smoking.
To broaden the search, the reference lists of all included studies were examined to identify any other potentially relevant papers (pearling). Results were limited to studies published in English from the year 1997 to 2016.
Exclusion criteria from the initial search included:
- Editorials or correspondence
- Items that were not journal articles, reviews, clinical trials, government publications or observational studies
- Languages other than English
- Published prior to 1997
- Items not published in peer-reviewed journals
- Included ages less than 18
- Items that did not involve military, veterans or servicemen
- Items that did not report respiratory problems.
Included studies were assessed on their design and level of evidence according to the Australian National Health and Medical Research Council (NHMRC) hierarchy of evidence.12 Inclusion criteria were further refined to focus on:
- Deployed Service members or Veterans of military forces
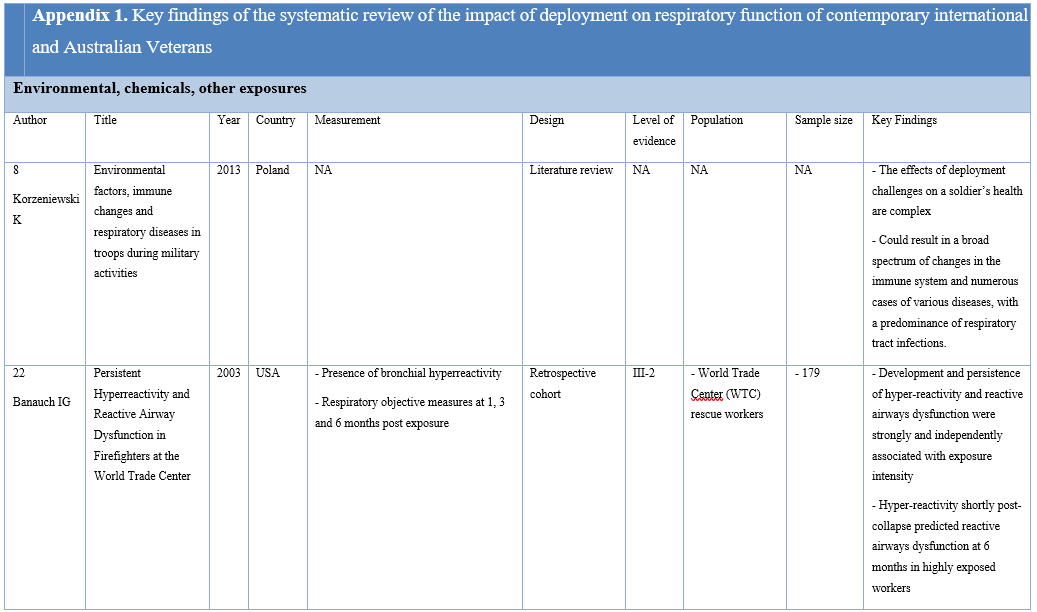
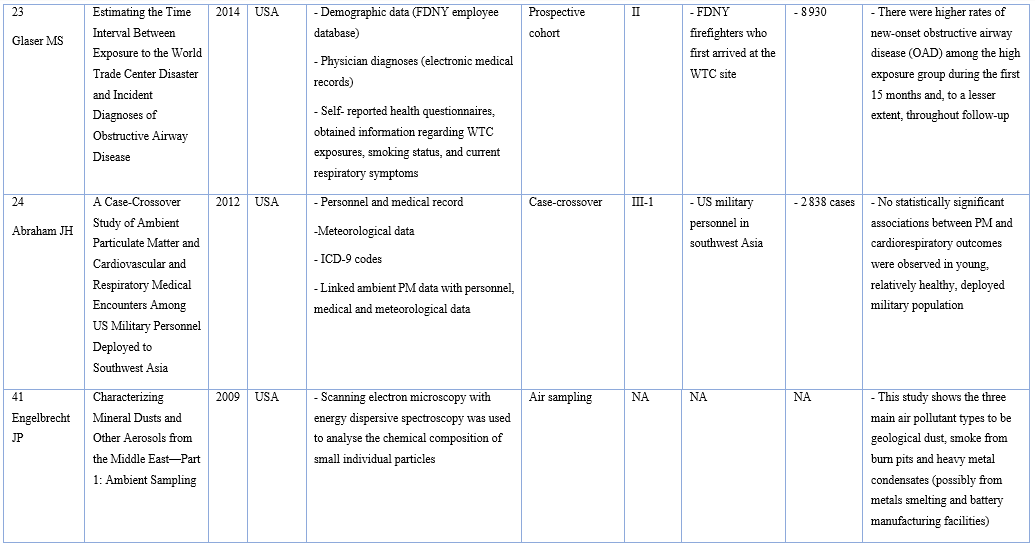
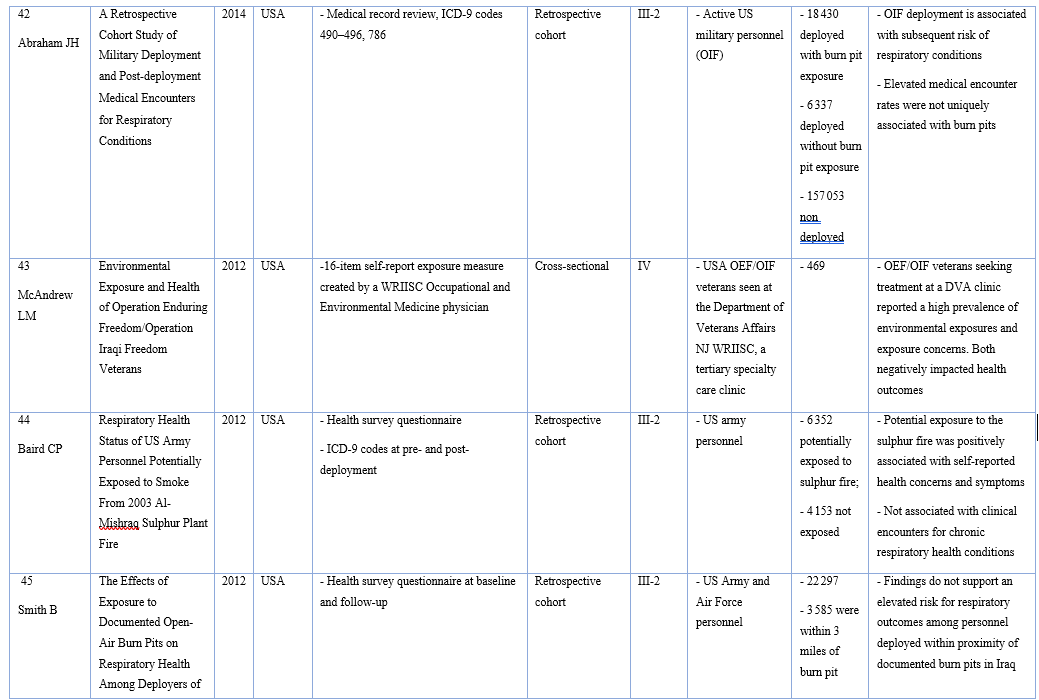
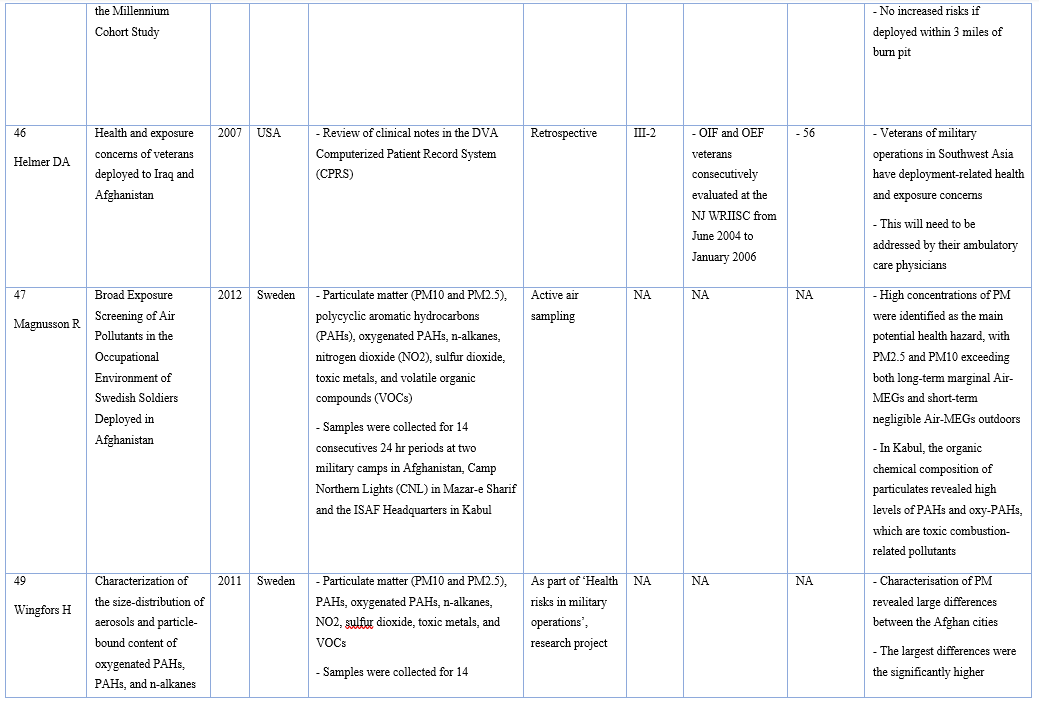
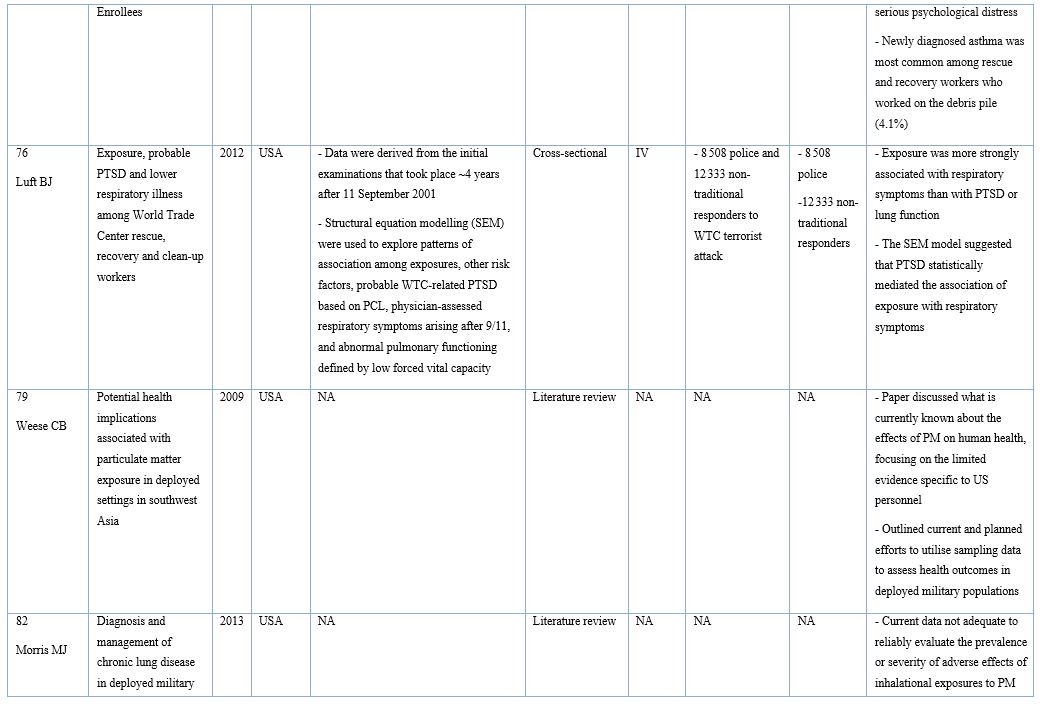
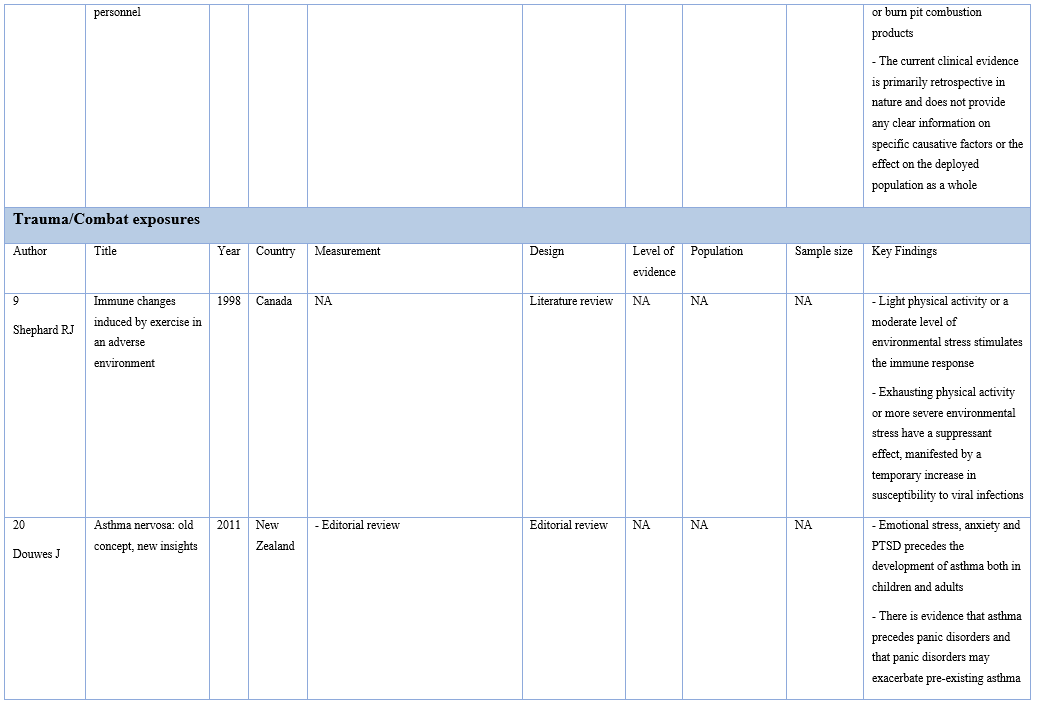
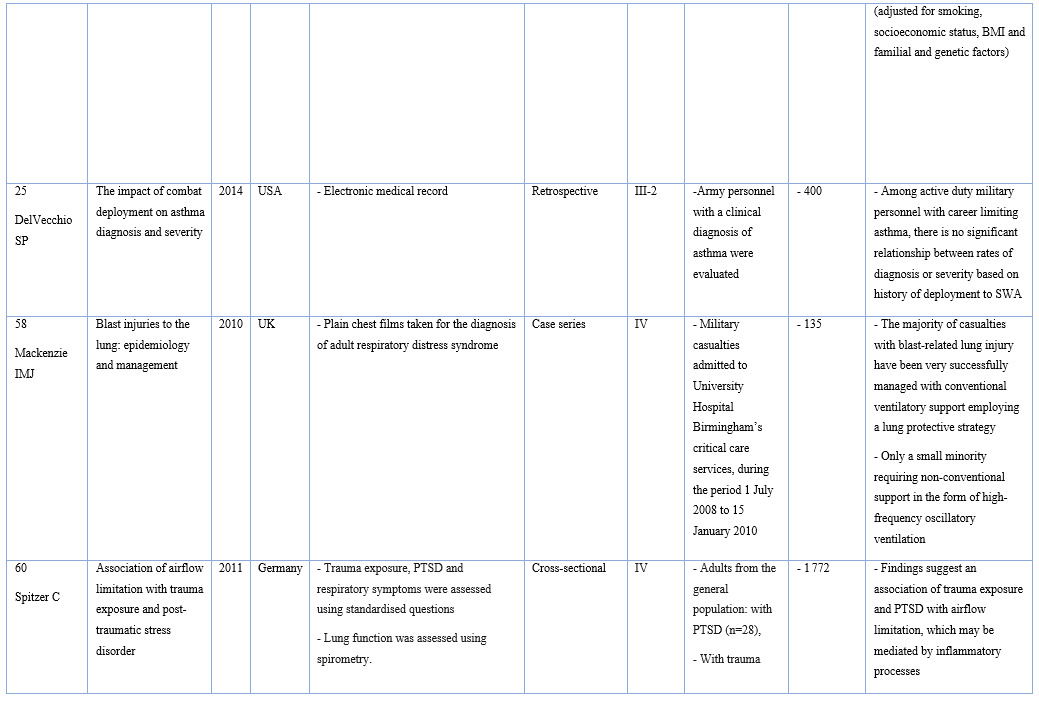
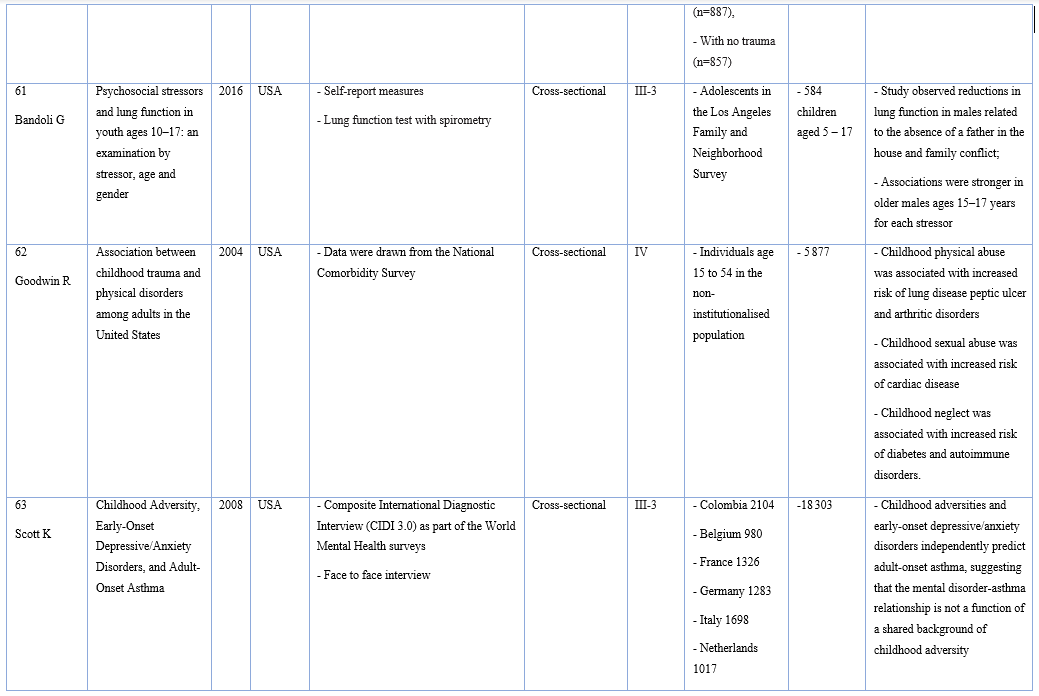
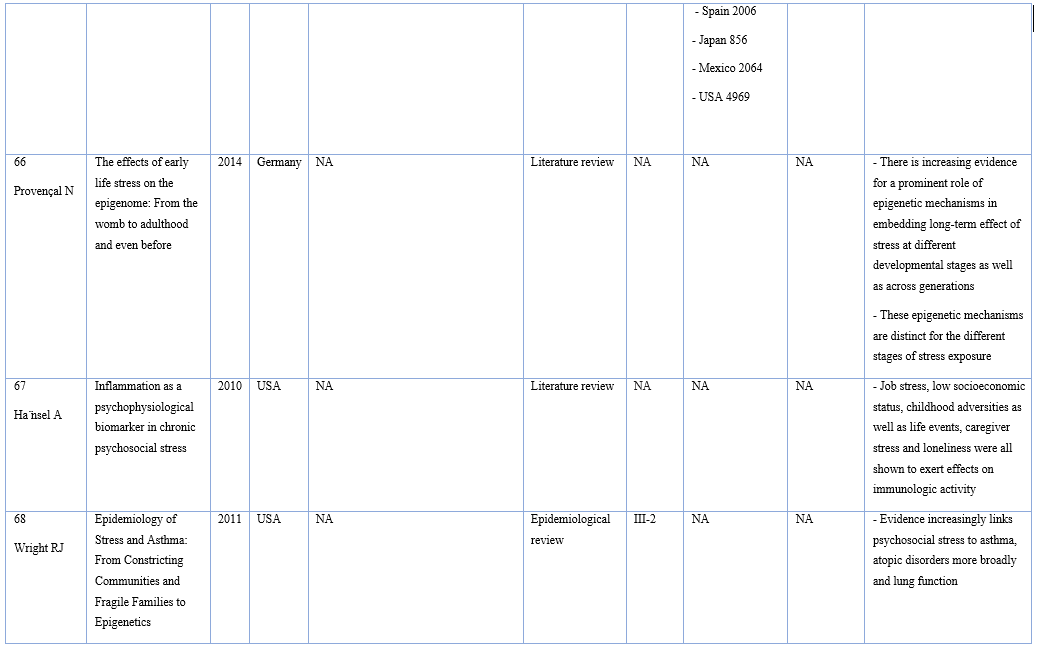
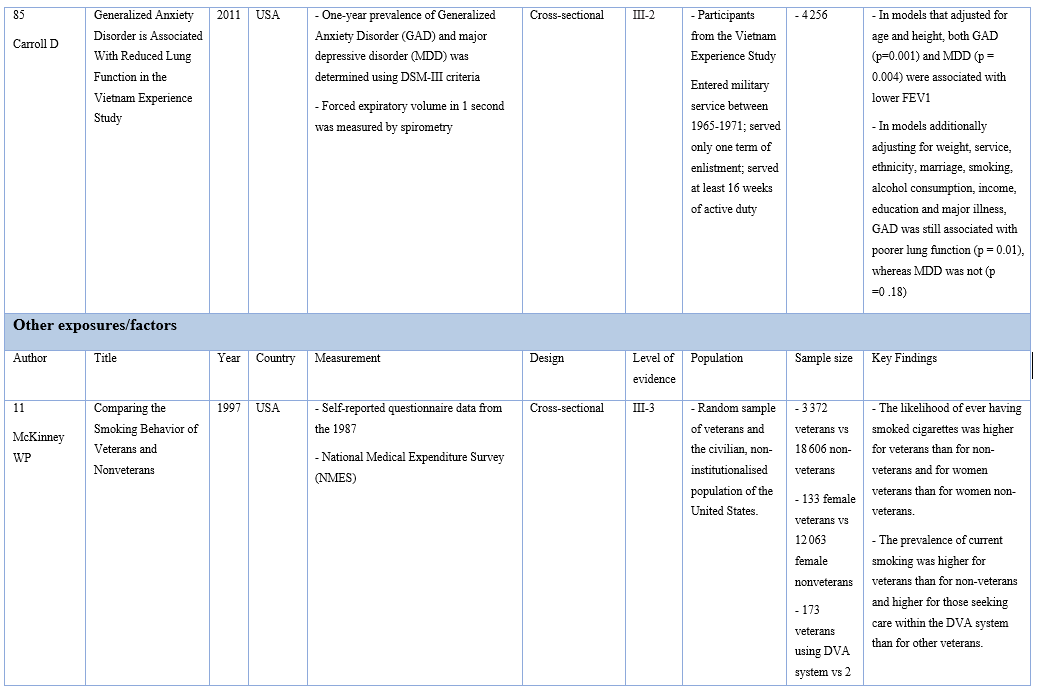
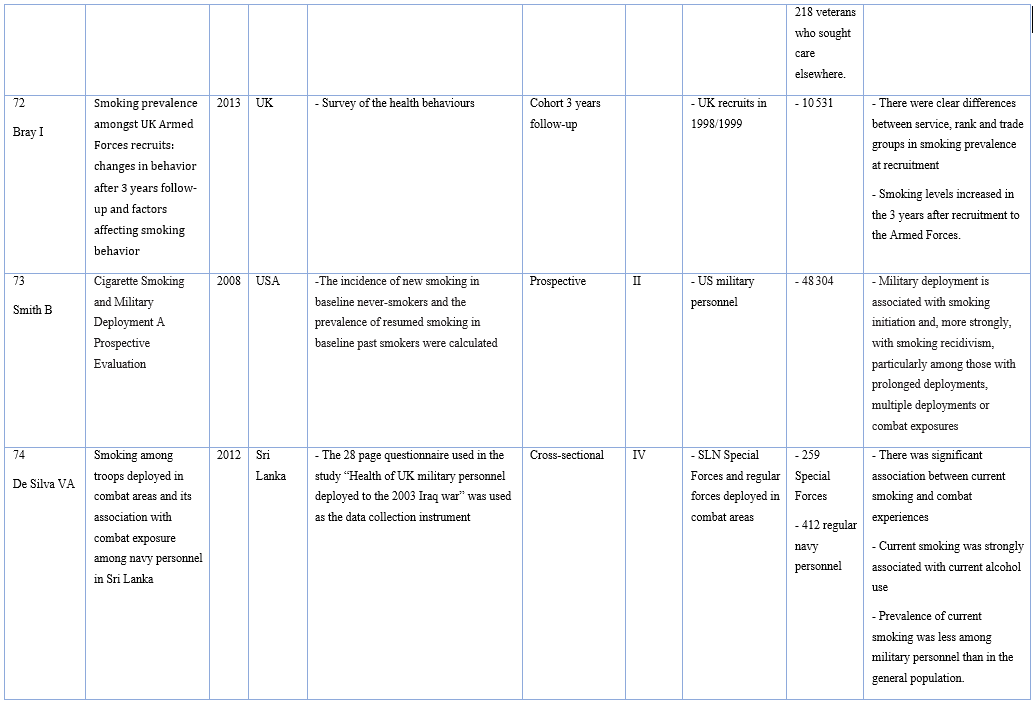
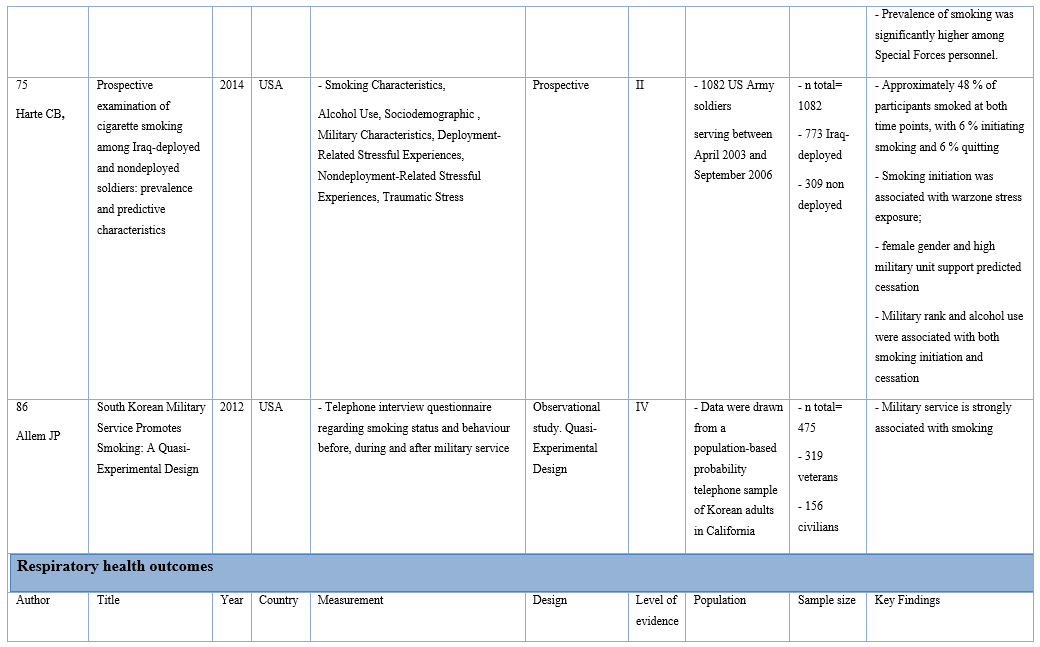
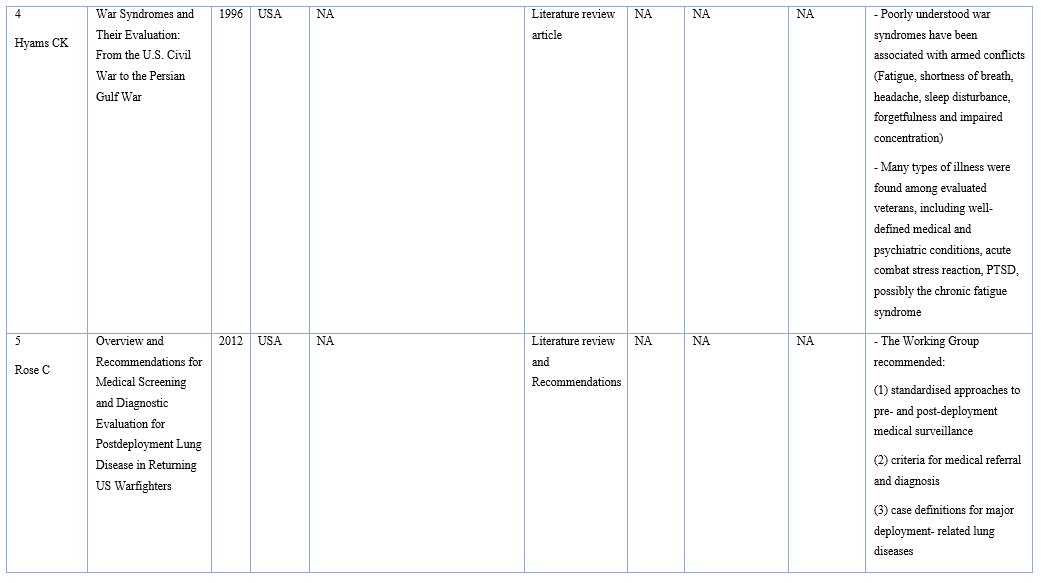
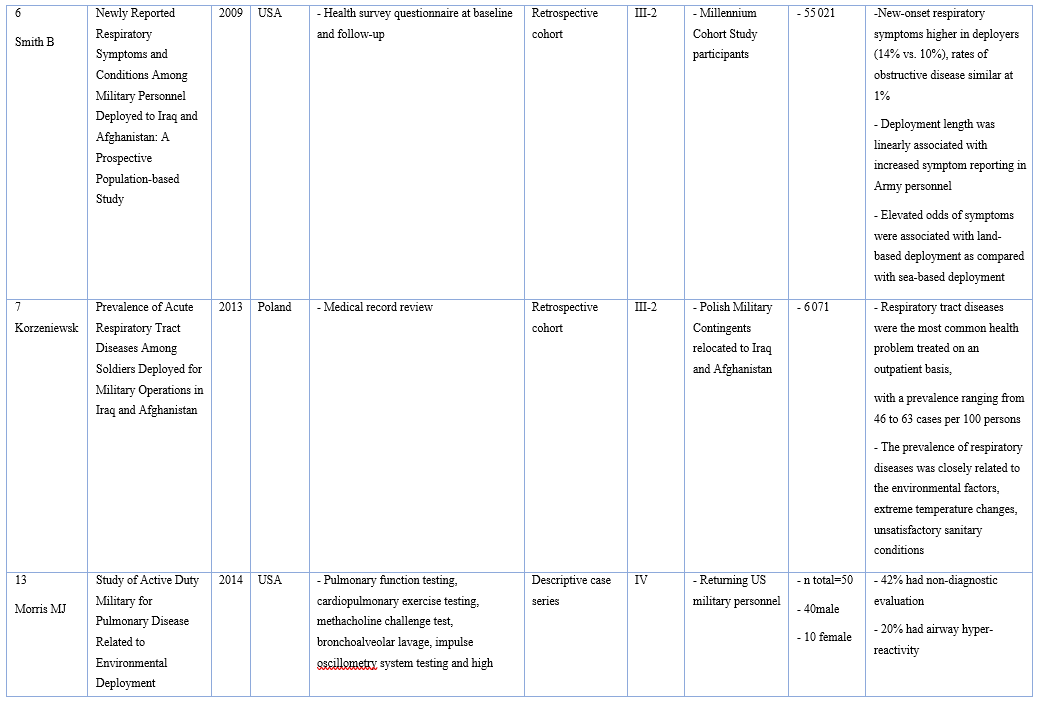
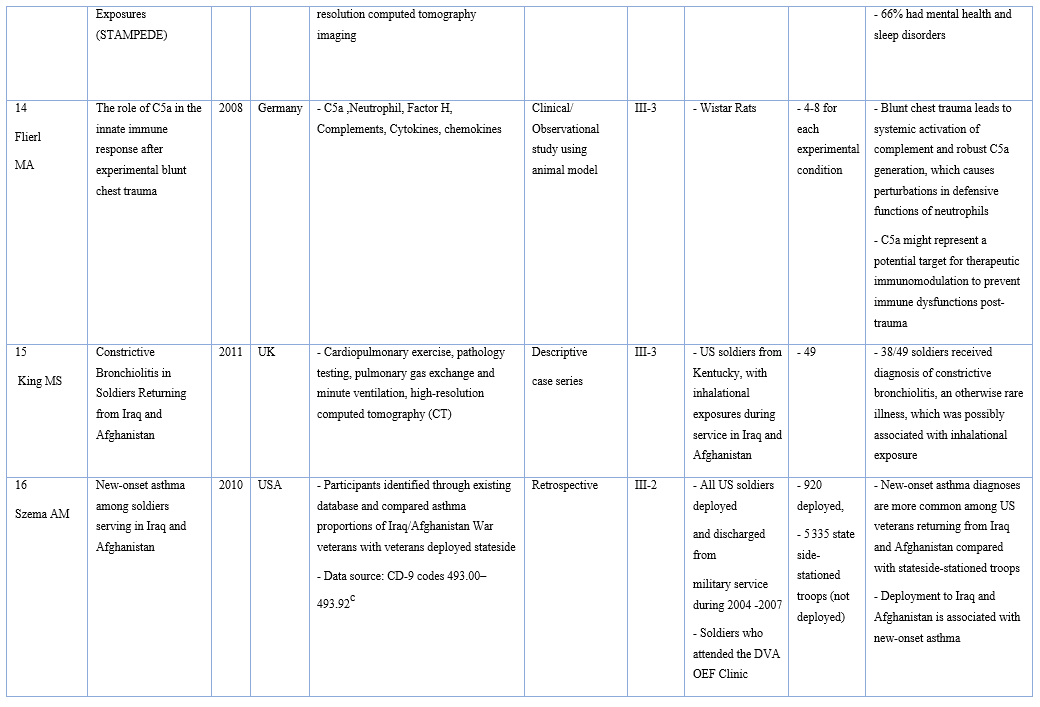
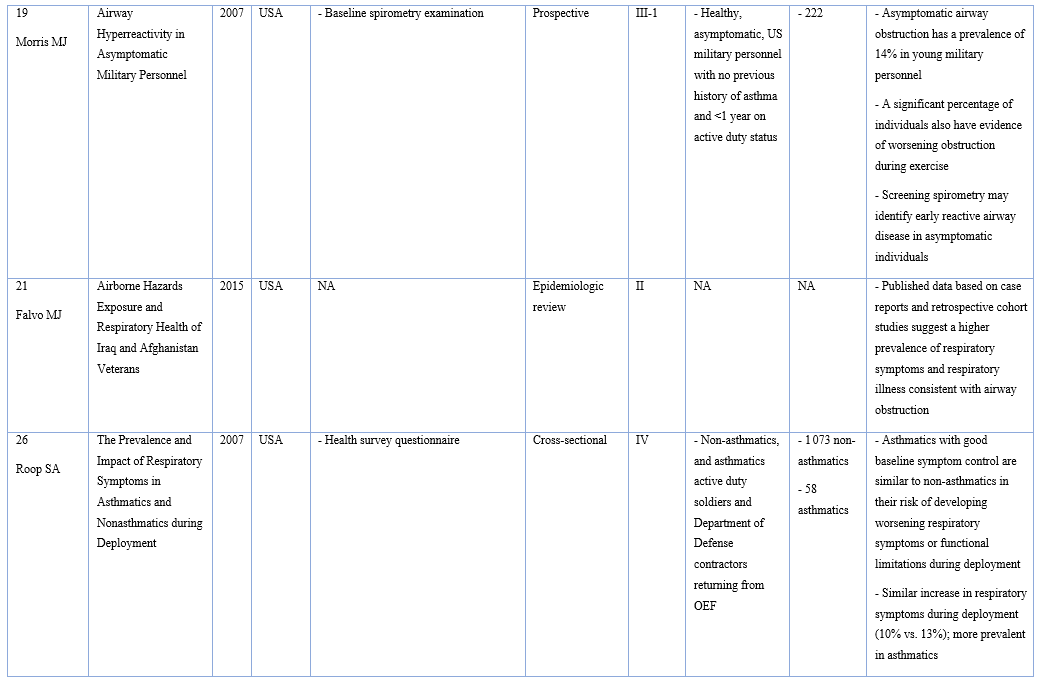
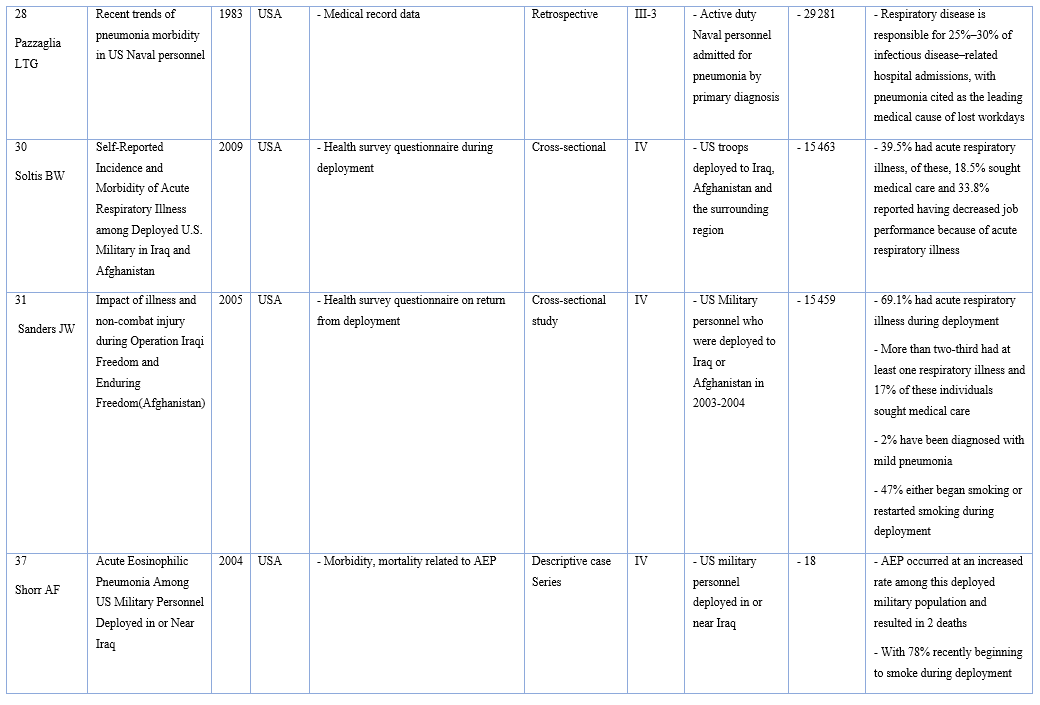
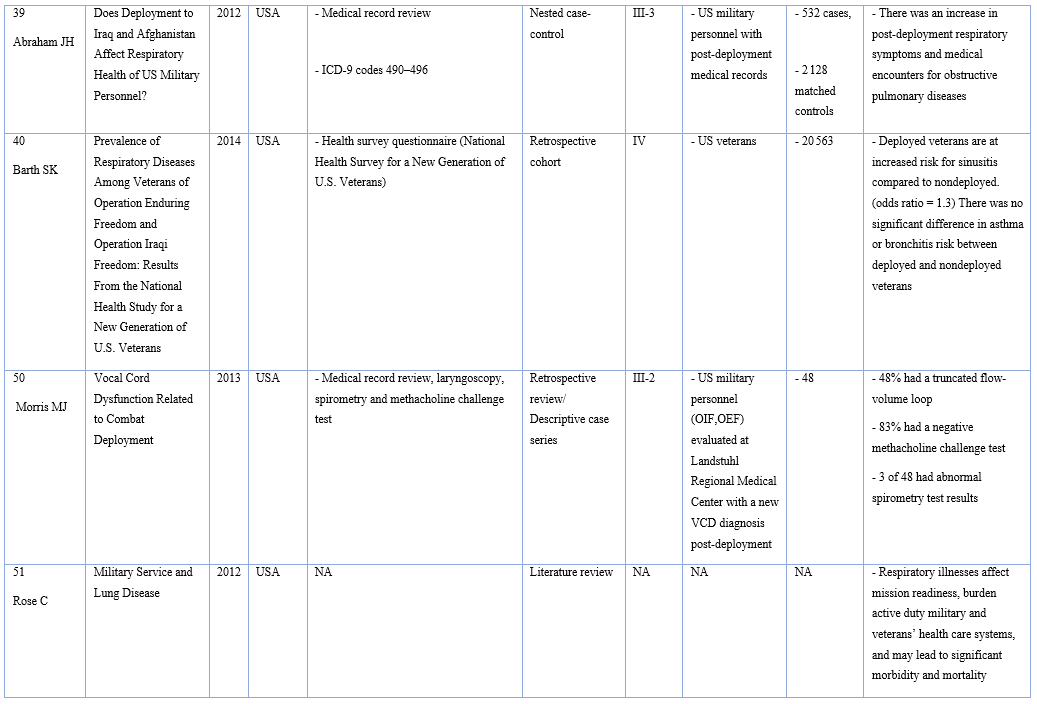
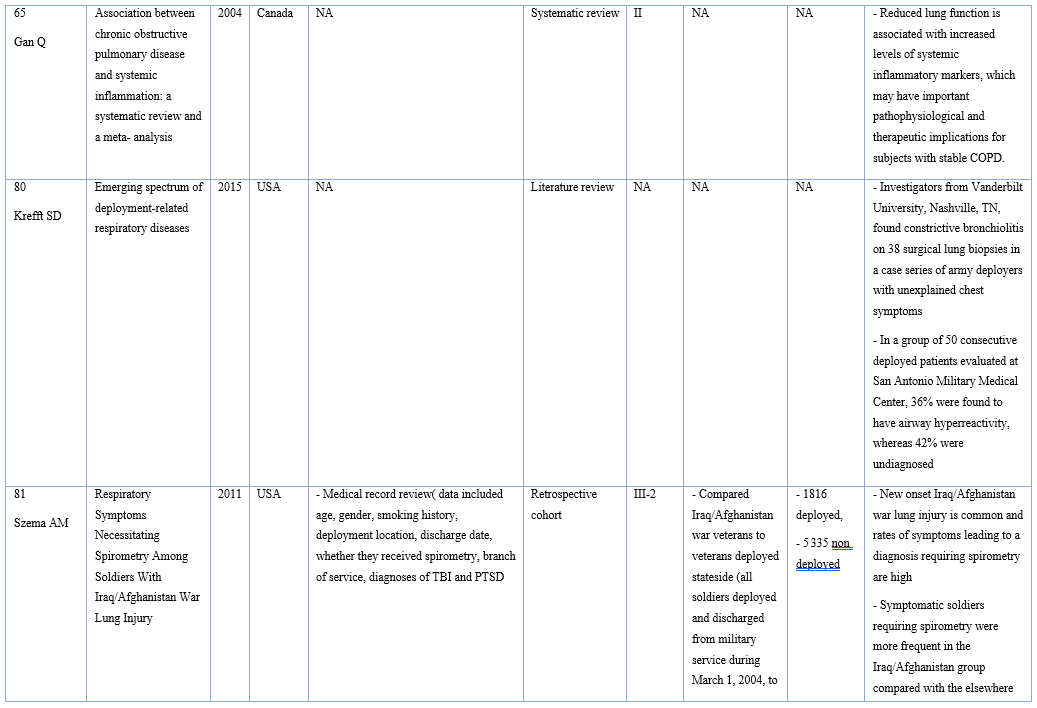
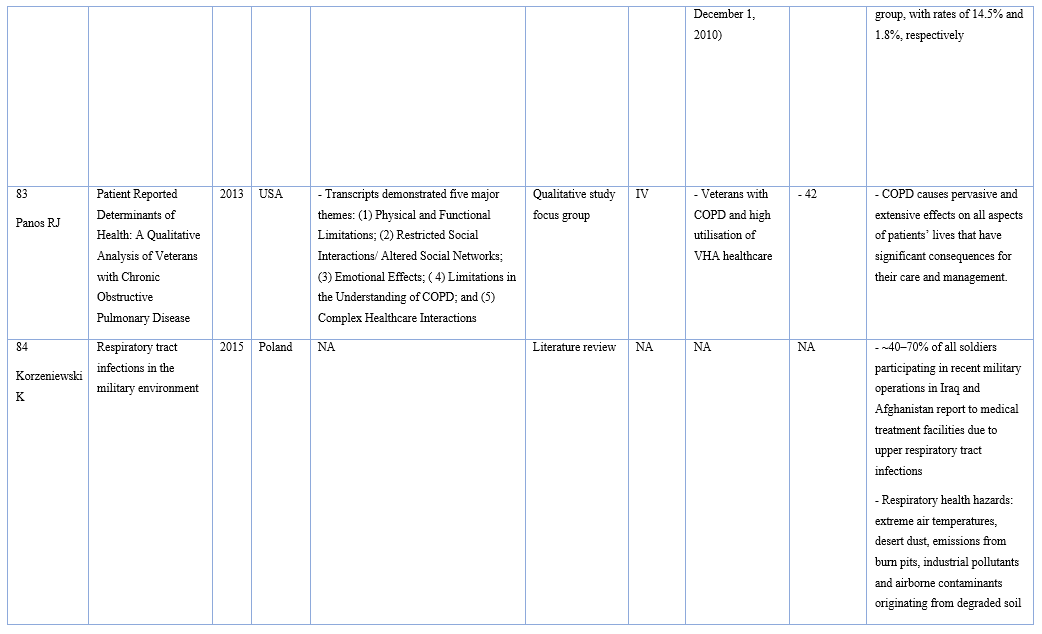
- The impact of deployment exposures and associations with respiratory health. Key findings of articles, country of origin, measurement, population and sample size are presented in Appendix 1. Where possible a military comparison group was preferred; however, broader criteria were used to provide the most comprehensive overview of available published research. Due to the limited research in this area, studies of lower levels of evidence addressing issues of interest were retained, although findings were interpreted with caution and used as supporting rather than primary evidence sources. A total of 172 papers were evaluated by the lead author, with ~50% n=87) also evaluated by the second author. Following this process, a total of 85 papers were included in this review (see Figure 1).
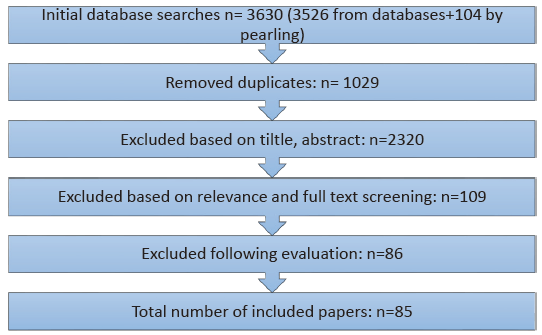
Figure 1: Studies obtained from initial database searches
Results
Preliminary assessment of studies identified the following key areas where the impact of deployment on these respiratory outcomes could be examined.
- Environmental and/or chemical exposures including; particulate matter (including metal particles), burn pits and air pollution
- Trauma and combat exposures including; blast, trauma/stress
- Other exposures/factors including; physical activity, smoking and individual susceptibility factors.
Papers were grouped accordingly. An assessment of the available evidence was summarised for each outcome, and conclusions regarding the state of evidence in the area as a whole presented, including an overview of notable gaps. Key study information and findings, organised by topic, are summarised in Appendix 1.
Respiratory health outcomes in deployed military populations
International studies have documented an increased incidence of respiratory disorders in military personnel who served in the Middle East compared with non-deployed populations.5-7 Overall, studies have reported increased rates of non-specific respiratory symptoms, asthma and constrictive bronchiolitis in deployed military personnel, with evidence that exposures while on deployment contribute to this via direct actions and by disturbance of the immune system.
In a study of the causes underlying respiratory symptoms in military personnel returning from duty in Iraq and Afghanistan by Morris et al.(2013), 42% of US Veterans reported non-specific respiratory symptoms, although most did not reach the threshold for a specific clinical diagnosis.13 The majority of patients who did receive a specific diagnosis had evidence of asthma or nonspecific airway hyper-reactivity. This may have reflected aggravation of pre-existing disease13 or hyper-activation of the immune system.14 Smith et al.(2009) also reported that deployment was associated with respiratory symptoms in both US Army and Marine Corps personnel, independent of smoking status and deployment length was positively associated with increased symptom reporting in Army personnel. This study concluded that specific exposures rather than deployment in general are determinants of post-deployment respiratory illness.6 Further recent US studies have also implicated inhalational exposures during deployment as predictors of constrictive bronchiolitis and new-onset asthma in Veterans.15, 16
In this review, we describe the most prevalent respiratory health outcomes reported among military personnel including asthma, constrictive bronchiolitis (CB), chronic obstructive pulmonary disease (COPD), respiratory infection and acute eosinophilic pneumonia (AEP).
Asthma
Asthma, a form of reversible bronchospasm, is usually connected to allergic reaction or other forms of airway hypersensitivity. Given the nature of deployment exposures, deployed populations may be at risk of increased inflammation, which in turn can impact on respiratory function.17 Since 2004, US military candidates diagnosed with asthma after the age of 13 have been excluded from military enlistment unless exempted via medical waiver.16 Entry to the Australian Defence Force (ADF) for people with asthma similarly changed post 2007.Currently candidates with mild asthma may be considered for entry to the ADF subject to certain criteria, including normal spirometry and negative bronchial provocation testing.18 However, rates of asthma among serving military personnel are generally low, in comparison to the general population. Despite low asthma rates at intake into the military, asthma diagnoses have increased in the US military since the beginning of the Iraq Afghanistan war.6, 19 The US Department of Defense reported that 13% of US Army Medical visits in Iraq were for new-onset acute respiratory illness.16
Recently, an increasing number of studies have reported consistent positive associations between psychosocial stress and asthma6, 13, 16, 20 suggesting that, in the context of military service and deployment specifically, both environmental exposures and also the psychological stress of deployment should be considered as important contributing factors. In relation to deployment specifically, several studies provide evidence of an association between deployment and new-onset asthma and other respiratory symptoms.6, 16, 19 A retrospective review of medical diagnoses by Szema et al.(2010) of more than 6 000 US military personnel deployed and subsequently discharged from military active duty, reported that deployment to Iraq was associated with a higher risk of having a new International Classification of Diseases-9 (ICD-9) diagnosis of asthma post deployment.16 Similar findings were documented in occupationally exposed first responders to the World Trade Center disaster.21-23
In a case control study, Abraham et al.(2012) reported an increase in post-deployment respiratory symptoms and medical encounters for obstructive pulmonary diseases, relative to pre-deployment rates, in the absence of an association with cumulative deployment duration or total number of deployments, indicating that it may be more specific exposures having an impact rather than deployment alone.24 However, in contrast, Del Vecchio et al.(2015) evaluated 400 US Army personnel with a clinical diagnosis of asthma and found that there was no significant relationship between rates of diagnosis or severity based on history of deployment.25 The findings from this retrospective study may indicate that deployment-related lung conditions are subtle and require careful evaluation over time to determine the long-term impacts of deployment on the development of respiratory disease. Furthermore, this study did not focus on deployment-related environmental exposures, which may explain why no association was found.
Despite screening processes in many international militaries, pre-existing disease may also play a role in the development of respiratory symptoms. In a prospective study Morris et al.(2007) examined airway hyper-reactivity in asymptomatic US military personnel.19 Asymptomatic airway obstruction had a prevalence of 14% in young military personnel with evidence of worsening obstruction during exercise. This suggests that rates of asymptomatic asthma may be higher than previously recognised. Results of a cross-sectional study by Roop et al.(2007) suggested that asthmatics with good baseline symptom control are similar to non-asthmatics in their risk of developing worsening respiratory symptoms or functional limitations during deployment.26
Overall some studies show increased rates of asthma, which may or may not be related to deployment. There are also suggestions that asymptomatic asthma may be underestimated, therefore deployment could possibly be exacerbating, rather than causing the condition. However, in the absence of mandated pre-enlistment lung function testing, it is difficult to determine the true prevalence of asthma or hyper-reactive airways in the enlistment population.
Constrictive bronchiolitis (CB)
Constrictive bronchiolitis (CB) is a recognised form of non-reversible obstructive lung disease in which bronchioles are compressed and narrowed by fibrosis and/or inflammation. In a descriptive case series by King et al.(2011), 49 soldiers that returned from the Middle East with unexplained respiratory symptoms underwent lung biopsy.15 Thirty-eight of these soldiers subsequently received diagnosis of CB, an otherwise uncommon diagnosis. The majority of biopsy samples showed polarisable material consistent with the inhalation of particulate matter, even though most of the soldiers were lifelong non-smoker. In addition, thickening of the arteriolar wall or occlusion in adjacent arterioles was observed, which may have been the result of toxic inhalation.
Chronic obstructive pulmonary disease (COPD)
A small number of participants in a prospective study of Australian military personnel deployed to the MEAO were found to meet the global initiative for COPD criteria. A slight but statistically significant change to lung function between pre-and post-deployment was also observed among this group, specifically between small decreases in the lung function and reported exposure to different chemical and/or environmental exposures.1 In a retrospective review by Matthews et al.(2014), military personnel diagnosed with COPD were investigated. Despite evidence of increased respiratory symptoms in deployed military personnel, this study reported that the impact of deployment on increased diagnosis or severity of COPD appears minimal.27
Infection
Respiratory infections are the leading cause of outpatient treatment during deployment and account for 25–30% of infectious disease hospitalisations in US Army personnel.28, 29 Soltis et al.(2009) found that 39% of soldiers have had at least one respiratory infection while on deployment.30 The deployment environment may facilitate transmission of respiratory infections, thereby accounting for higher incidence rates than comparable civilian populations. Service members may be exposed to high level of stress, contagious novel pathogens, harsh environmental conditions31 as well as overcrowding and inadequate hand-washing facilities.32 Respiratory bacteria and viruses are transmitted person-to-person via respiratory droplets, and typically result in acute self-limiting infections.33 However, highly virulent and transmissible strains of pathogens can lead to morbidity and mortality.34
Combat training programs are demanding, involving not only prolonged periods of physical activity but also exposure to psychological stressors, sleep deprivation, shifts in daily rhythm, and exposure to thermal extremes and high-altitude environments. The effects of such challenges on a soldier’s health are complex, resulting in a broad spectrum of changes in the immune system, which may predispose to various diseases, predominantly of the respiratory tract.8 Although recent attention has been directed towards acute morbidities as a result of respiratory infections, the adverse long-term effects of respiratory infections are not well understood, specifically in military populations. Given the potentially high rates of respiratory infection in deployed personnel, this is an important area for further research.
Acute Eosinophilic pneumonia (AEP)
Acute eosinophilic pneumonia (AEP) is an uncommon, idiopathic lung disease. The diagnosis is typically based upon clinical testing that include bronchoalveolar lavage, blood test or smear and chest radiograph. Lung biopsy is rarely necessary. AEP is characterised by general respiratory symptoms, alveolar and or blood eosinophilia, and peripheral pulmonary infiltrates on chest imaging.35 In most cases the acute illness lasts less than four weeks. Dry cough, dyspnoea and fever are present in almost every patient. Associated symptoms and signs can include malaise, myalgia, night sweats, chills and chest pain.35 Some studies suggest that AEP is an acute hypersensitivity reaction to an unknown inhaled antigen in an otherwise healthy individual.36 Eighteen cases of AEP (including two fatalities) were reported among over 180 000 military personnel deployed in or near Iraq between March 2003 and March 2004.All AEP patients were smokers with 78% recently beginning to smoke during deployment and all but one patient had significant exposure to fine airborne sand or dust; no other common source exposure could be identified. The study concluded that ‘recent exposure to tobacco may prime the lung in some way such that a second exposure or injury, eg, in the form of dust, triggers a cascade of events that culminates in AEP’.5, 37 AEP was also reported in at least one firefighter following the collapse of the World Trade Center towers in 2001.38
As outlined above, current literature, including case reports and retrospective cohort studies, suggest a potentially higher prevalence of respiratory symptoms and respiratory illnesses including asthma,5, 16, 26 CB,15 COPD,1, 39 and AEP37 among deployed military personnel. Specific deployment-related exposures such as environmental (particulate matter, metal particles, burn pit, air pollution), combat (blast, stress) and other exposures (smoking, physical activity, military living conditions) may relate to these impairments in respiratory function5, 10, 11, 15, 37, 40-44 and are discussed below.
Environmental and/or chemical exposures
Military personnel who have served in Iraq and Afghanistan have expressed concern about possible long-term health effects associated with environmental exposures during deployment, including toxic industrial chemicals, local combustion sources and poor air quality.5, 41, 42, 45-47 US Veterans seeking treatment at Department Veterans Affairs (DVA) clinics after deployment, have reported a high prevalence of environmental exposure and exposure concerns, although whether this concern translates to actual adverse respiratory health outcomes is unclear.
In line with these concerns, researchers have hypothesised that there may be a relationship between deployment exposures and respiratory symptoms.21, 43, 46, 47 Korzeniewski et al.(2013) reported that the prevalence of respiratory diseases was closely related to environmental factors on deployment, such as exposure to sand and dust storms, extreme temperature changes and poor public health measures.7 A medical research working group formed to consider lung disease in US soldiers returning from Iraq and Afghanistan identified a number of potential risks for developing lung disease post deployment. These include type, severity and duration of exposure to environmental hazards, such as desert dust storms, proximity and duration of exposure to burn pits or fires, and frequency of exposure to air pollution.5
Air pollution
Air sampling studies, conducted by US researchers suggest that multiple sources of air pollution including smoke from oil well fires, sand and dust storms, and not exclusively burn pit emissions, contribute to poor air quality in the deployed environment.46, 48 These findings are supported by independent work from investigators outside of the US;47-49 however, there is no data available from longitudinal research studies with objective pulmonary assessments comparing lung function between those deployed to the Middle East and non-deployed personnel. A review article by Falvo et al.(2015) summarised current knowledge about the impact of service and environmental exposures on respiratory health of military Service members deployed to Iraq and Afghanistan.21 The report reviewed 19 studies published from 2001 to 2014.While studies of environmental exposures, in particular airborne pollutants, have shown an association with an increased burden of acute respiratory symptoms, studies reporting chronic respiratory diseases do not provide conclusive results, mainly because of the non-representative sample of the study populations. Data associating airborne hazard exposures to respiratory disease are similarly inconclusive. Therefore, there is insufficient evidence to support any association between air pollution in the deployed environment and respiratory health of military personnel.21
Particulate matter (PM)
US data suggests that deployment to both Iraq and Afghanistan may pose additional risk factors to respiratory health because of the high levels of airborne PM and geologic dusts inherent in those regions.50 A majority (94%) of US Service personnel deployed to OIF and OEF reported exposure to high levels of airborne PM from a range of sources that may have exceeded environmental, occupational and military exposure guidelines,43, 51 indicating that these pose a real risk to health. McAndrew et al.(2012) reported that among MEAO deployed personnel, the most prevalent exposures were air pollution (94%), vaccines (86%) and petrochemicals (81%).43 Exposures and concern about exposures were both related to greater somatic symptom burden, and concern about exposure was highly correlated with symptom burden.
Metal particles
Another exposure of relevance to the deployed environment is metal PM. Biopsied lung tissue from selected deployed US soldiers with unexplained respiratory symptoms and history of inhalational exposure, identified the presence of metals including iron, titanium and crystalline material. This deployment’s inhalational exposure was thought to be the cause of unexplained exertional dyspnoea and diffuse CB conditions in these soldiers.15 Exertional dyspnoea is excessive shortness of breath and mainly reflects poor ventilation or oxygen deficiency in circulating blood.CB is a rare, small airway fibrotic respiratory disease. The cause of this condition is still unknown, although it is thought that environmental factors and genetic susceptibility could be major contributors to the development of the disease.52 King et al.(2011) found that in 38 of 49 previously healthy soldiers with unexplained exertional dyspnoea and diminished exercise tolerance after deployment, an analysis of biopsy samples showed diffuse CB, possibly associated with inhalational exposure.15
Burn pit
A further identified exposure for respiratory insult, again common in the MEAO, is open-air burning of rubbish and other waste. Although the extent of the chemicals released in burn pits is unknown, ambient air sampling performed in selected Middle East regions has revealed that smoke from burn pits is a major source of air pollution.42 Some air pollutants such as dioxins, carbon monoxide, volatile organic compounds from burning of trash, vehicle/generator exhaust, oil well fires, gases from industrial facilities, and contaminants from dust containing silica, asbestos, lead, aluminium and manganese are well recognised carcinogens. Other agents may irritate the respiratory system causing acute cough or shortness of breath, hypersensitivity pneumonitis, irritant induced asthma and CB, especially when exposures are repetitive or exceed recommended concentrations.45
Evidence to support long-term adverse effects of exposure to burn pits is controversial. Although some studies have found that deployment may be associated with a subsequent risk of developing respiratory conditions. Abraham et al.(2014) suggests that elevated medical encounter rates (visits to medical centres for respiratory outcomes including general respiratory system and other chest symptoms, asthma, COPD, bronchitis, emphysema, bronchiectasis and extrinsic allergic alveolitis) were not uniquely associated with burn pits.42 In this study, medical encounter rates among personnel deployed to burn pit locations were compared directly to those among personnel deployed to locations without burn pits. No significant differences in respiratory outcomes between these groups were found.
Furthermore, findings from Smith et al.(2012) do not support an elevated risk for respiratory outcomes among personnel deployed within proximity of documented burn pits in Iraq.45 Comparing burn pit exposed and non-exposed groups, this study observed similar proportions of newly reported CB and emphysema (1.5% vs 1.6% respectively), newly reported asthma (1.7% vs 1.6%), and respiratory symptoms in 2007 (21.3% vs 20.6%).Similarly, a study by Baird et al.(2012) reported that while potential exposure to sulphur plant fires was positively associated with self-reported health concerns and symptoms, it was not associated with an increase in clinical encounters for chronic respiratory health conditions.44 Powell et al.(2012) found no increase in chronic multi-symptom illness (CMI) symptom reporting in military personnel deployed to three selected bases with documented burn pits compared with other deployment sites.53 However, limitations in standardising exposures may have biased these results.
Toxicological, epidemiological and clinical data are limited and prevent reliable evaluation of the prevalence or severity of adverse effects of inhalational exposures to PM or burn pit combustion products in military personnel deployed to Iraq and Afghanistan. The current clinical evidence on the effect of deployment on respiratory health is primarily retrospective and does not provide clarity regarding specific causative factors or the effect on the deployed population as a whole.21 Taken together, these findings suggest that environmental exposures including burn pits and air pollution may be associated with subjective physical health symptom reporting, but there is no evidence of increased rates of objective respiratory health outcomes.
Regardless of the source, it seems likely that higher levels of air pollution are common in many deployment areas and could contribute to future pulmonary and other health effects not yet identified.48 Together, these findings indicate that while deployment appears to be associated with adverse respiratory outcomes, this cannot be reliably attributed to environmental exposures. Other deployment exposures that should also be considered include trauma, particularly blast trauma and psychosocial stress associated with a combat environment.
Combat exposures
Blast
In addition to air pollution and smoke from burn pits, military Veterans who have served in Iraq and Afghanistan may have been exposed to other significant respiratory stressors, such as aerosolised metals and chemicals from improvised explosive devices (IEDs), or to traumatic respiratory insult such as blast overpressure or shock waves to the lung.54
Concern about the effects from embedded metal fragments from IEDs used in the Middle East conflicts has been raised among Service members. As a result, the US DVA established a special registry in 2008 for medical surveillance and management of Veterans with retained metal.51 Some of the embedded metal contaminants, including aluminium, arsenic, cobalt, chromium and nickel, may have immunogenic respiratory health effects. In a recent report from the Toxic Embedded Fragment Surveillance Centre, of 89 urine samples tested, 47% exceeded the reference value for aluminium and 31% for tungsten.55
Recently, publication of an unusual case report of chronic beryllium disease (CBD) was described in a 41-year-old Israeli soldier who suffered mortar shell injury with retained shrapnel in the chest wall. This report raised the possibility of shrapnel- induced CBD from long-term exposure to the surface of retained aluminium shrapnel fragments in the body.56
It has been proposed that Service members who sustained subclinical blast injury may be susceptible to long-term sequelae. Apart from direct consequences of blast injuries such as blast pressure wave, fragments of debris or injuries due to acceleration or deceleration, there are also less obvious injuries caused by a blast including psychological trauma, burns and toxic-substance exposure from inhalation of hot contaminated air.57,58 Such injuries can have unpredictable long-term outcomes including permanent fibrosis of the bronchial mucosa.59
Despite the high plausibility of long-term adverse effects following acute pulmonary blast injury, there is an absence of data on the long-term outcomes. Furthermore, the possibility of other long-term pulmonary consequences of blast exposure, such as the effect of explosion-related dust exposure, and other exposures such as smoking, has not been adequately examined. Overall there is limited data to support a conclusion regarding an association between exposure to blast and long-term respiratory outcomes.57
Trauma/stress
In addition to the frequent and proximate exposures to ambient airborne hazards, factors unique to military service that may make military personnel more vulnerable to greater respiratory health risk include high levels of psychological stress.21 Vocal cord dysfunction (VCD) refers to abnormal closing of the vocal cords when inhaling or exhaling. It is often misdiagnosed as asthma in the clinical setting and has been reported in military personnel.50 A study of exertional dyspnoea in US military personnel demonstrated that 12% of patients evaluated had evidence of VCD, most of which was exercise related. Morris et al. suggested that the development of VCD in the deployed environment might be related to nonspecific upper airway irritation, underlying psychiatric conditions and/or significant stress attributed to the combat environment.50
There is also growing evidence for an association between exposure to traumatic stress, including childhood maltreatment or combat experience and pulmonary diseases such as asthma, CB and COPD.60-63 This relationship was also demonstrated in adult research populations exposed to the 11 September 2001 World Trade Center terrorist attack. More specifically, moderate associations between probable post-traumatic stress disorder and respiratory symptoms have been observed in first responders to the World Trade Center disaster.22, 23, 60, 64
A cross-sectional study conducted by Spitzer et al.(2011), analysed the associations between lung function, trauma exposure and post-traumatic stress disorder (PTSD) in 1 772 adults from the general population using standardised questions and spirometry test.60 Those with a diagnosis of PTSD had a significantly greater risk of having asthma symptoms than those without PTSD. However, those with a history of psychological trauma, but no diagnosis of PTSD, did not have an elevated risk, suggesting the association is specific to disorder status rather than symptomatology or trauma exposure. Analyses indicated that subjects with diagnosed PTSD had a significantly increased risk for airflow limitation independent of its definition.
One possible mechanism underpinning the association between stress and reduced respiratory function could be increased levels of systemic inflammatory markers.20, 65-68 Excessive pro-inflammatory responses may cause airway damage and consequently structural and functional pulmonary changes.31 Hypothetically, higher levels of stress during deployment among personnel may, in part, explain the increased rate of respiratory symptoms reported in recent studies. There is increasing evidence of associations between stress related mental disorders such as PTSD and altered immune responses, and elevated circulating inflammation. The direction of this association is not conclusive, however. Regardless, low level inflammation and altered immune response provide plausible mechanisms by which trauma exposure may be associated with respiratory symptoms.20, 60, 65-68
Other exposure factors
In addition to deployment specific risks, evidence suggests other military factors such as physical activity, increased tobacco use and other individual susceptibility factors may increase the risk of respiratory symptoms and enhance susceptibility to environmental and trauma exposures in this population.
Physical activity
Researchers have suggested that physical activity performed in stressful environments alters immune function.17 Light physical activity or moderate environmental stress stimulate immune responses, but exhausting physical activity or severe environmental stress can have immune suppressant effects, manifested by a temporary increase in susceptibility to respiratory infections.9 Multiple physical and psychological stressors, such as those encountered on deployment, may induce alterations in immune parameters (as discussed above) and/ or neurological and endocrine responses; these common exertion-induced pathways could result in respiratory tract syndromes.8
Smoking
Cigarette smoking has been associated with morbidity and mortality in a number of studies.5-7, 21, 31, 69, 70 Pathological mechanisms of smoking and its adverse health effects generally overlap with environmental air pollution. Smoking has also been related to increased susceptibility to respiratory insult from airborne hazards.70 Interestingly, there is no clear evidence of direct effects of smoking on respiratory outcomes in deployed military populations. For example, Sanders et al. found that approximately 70% of US military personnel deployed to Iraq and Afghanistan reported at least 1 episode of an acute respiratory illness and 15% reported 3 or more incidents of respiratory illnesses during their deployment.31 There was, however, no observed relationship between cigarette smoking and self- reported respiratory illnesses during deployment; suggesting that factors other than tobacco use were likely to contribute to the observed respiratory symptoms and morbidity.
Findings from a prospective study of Australian military personnel deployed to the MEAO showed that those respondents who began or resumed smoking while on deployment were also likely to have more co-morbidities compared to those who did not smoke on deployment.1 Similarly, those who smoked more than usual were likely to have more co-morbidities compared to those who did not smoke.1 However, the relative impact of different exposures and other non-smoking related risk were not examined in this population.
Since the 1960s, the rate of tobacco smoking has declined in the US including in the military.71 However, the rate of tobacco smoking among active duty military personnel remains higher (32%) compared to the general population (~20%).71 Within the US military population, the prevalence of smoking is approximately 40% higher among Veterans and 50% higher among deployed military personnel compared with their non-deployed counterparts.71 In a cross-sectional study by Sanders et al.(2005), it was reported that 47.6% of US military personnel deployed to Iraq and Afghanistan began or resumed smoking while deployed and ~40% smoked half a pack of cigarettes or more per day.31 High rates of tobacco smoking are not restricted to US military personnel but are also increased 40%–60% among coalition militaries.72
While specific factors contributing to smoking rates have not been ascertained, the significant smoking uptake observed in a number of studies is thought to relate to deployment stress particularly among those with prolonged deployments, or combat exposures.73 Combat exposure, military stressors and PTSD have all been identified also as predictors for cigarette smoking.74, 75 As discussed above, these psychological risk factors and mental health disorders have also been associated with respiratory symptoms, abnormal lung function and diseases such as asthma.20, 76 Although tobacco smoke may differ in many respects from the ambient air pollution in deployed settings, the contribution of tobacco smoke exposure to military personnel’s cumulative exposures to airborne hazards while on deployment cannot be underestimated, given the prevalence and intensity of tobacco use in stressful combat situations.21 The potential for smoking to interact with and/or exacerbate other environmental or stress exposures is of importance to examine.
Individual susceptibility factors
Studies regarding the association between respiratory health conditions and individual factors (age, sex, BMI, blood pressure, physical fitness, pre-existing conditions and personal characteristics) in general the population and deployed military personnel generally focus on single respiratory outcomes and are usually assessed using different methods.
In a cross-sectional study, data collected from a European Community Respiratory Health survey of 16 countries were examined. The aim of this study was to estimate the age and sex-specific incidence of asthma from birth to the age of 44 in men and women across several countries, and to evaluate the main factors influencing asthma incidence in young adults. This study demonstrated that there are different patterns of asthma incidence in men and women. During childhood, girls had a significantly lower risk of developing asthma than did boys. Around puberty, the risk was almost equal in the two sexes, while after puberty, the risk in women was significantly higher than that in men.77
In a case control study of active duty and retired US military members, increasing BMI, younger age, gender, non-active duty beneficiary status and arthritis were significant independent predictors of asthma in this population.78 Similarly, Abraham et al.(2012) reported that gender, enlisted and Army personnel remained independent predictors of having a new obstructive pulmonary disease encounter.39 Age and combat occupations were not statistically significantly associated with a post-deployment obstructive pulmonary disease diagnosis. The way in which these factors might interact with deployment exposures to influence respiratory health outcomes has not been thoroughly studied. This deserves further attention in larger epidemiological studies, particularly given emerging evidence of their influence on physical and psychological health.
Limitations
Due to the limited research regarding respiratory health of MEAO deployed Service members, studies of lower levels of evidence addressing issues of interest were discussed in this review, although findings were interpreted with caution and used as supporting rather than primary evidence sources.
A number of studies in this review were of cross-sectional design; consequently, any respiratory health issues in existence before an exposure were not accounted. Without baseline data, it is not possible to accurately assess the impact of specific deployment exposures on a person’s respiratory health. Cross-sectional studies are carried out at one period and do not indicate the series of events, therefore it is difficult to determine the relationship between exposure and outcome as it lacks the time element.
Previous studies have largely relied on self-report data to measure the impact of exposures on respiratory health. This type of measurement is open to recall bias, particularly when data is collected well after exposures have occurred.31, 26 Medical record reviews are predominantly retrospective7, 16, 39 and therefore also subject to potential biases (reflected in documentation and health care seeking).
Discussion
Long-term psychological and physical health effects following deployment are of concern to Veterans, healthcare providers and the community. While some international literature suggests a higher prevalence of respiratory conditions in military personnel during and following deployment to the Middle East, findings are equivocal and the exact reasons underpinning any elevated respiratory health consequences are not well understood. Some inconsistencies in findings could be due to difficulties retrospectively standardising for exposure; reliance on self-reported symptoms or conditions, or inconsistent application of ICD codes, making it difficult to say with certainty which conditions are increasing in incidence or prevalence. Furthermore, many studies have focused on limited exposure and outcome variables. The potential interaction of these factors, and their effects on multiple respiratory outcomes, has not been thoroughly considered.
Current evidence (mainly from US studies) indicates that deployment-related environmental (PM, burn pit, air pollution, metal particles), combat (blast, stress) and other exposures (smoking, physical activity, military living conditions), and psychological trauma more generally, may be associated with several respiratory conditions in military personnel, such as asthma,5, 16, 26 CB,15 COPD,1, 39 sinusitis,40 and AEP37.These associations may be via direct actions and by disturbance of the immune system. Psychological stress, while highly prevalent in relation to deployment, is a less investigated risk factor for respiratory health outcomes and its contribution to respiratory health outcomes and potential mechanisms underlying associations, as well as potential predictors of good or poor health over time, are not well understood.61, 68, 79-85
Taken together, further prospective and cross-sectional analyses are needed to clarify relationships between the individual and combined impacts of environmental and psychological exposures on deployment, and any potential moderating or mediating effects of other factors on respiratory outcomes.

Corresponding author: Honey Ighani, honey.ighani@adelaide.edu.au Authors: H. Ighani 1,2, E. Lawrence-Wood 1,2, S. J. Neuhaus 1, A. McFarlane1,2
Author Affiliations:
1 The University of Adelaide
2 Centre for Traumatic Stress Studies






