Introduction
This article follows previous papers by the author, regarding occupational and environmental medicine in the Australian Defence Force (ADF).1,2,3,4,5 They assert that high rates of workplace illness and injury indicate the need to improve the management of hazards associated with ADF workplaces, with better emphasis on prevention. This assertion has been independently supported by a recent Productivity Commission report, indicating that the current compensation and rehabilitation system for both current- and ex-serving ADF members requires
fundamental reform.6
The author’s previous papers advocate that the ADF’s health services should be premised on an occupational health-based systems model. This would require reassessing the fundamental inputs to capability7 for both Joint Health Command (JHC), and Defence’s Work Health and Safety Branch. The current state of the ADF’s occupational and environmental health services, and the small number of civilian specialist occupational and environmental physicians, suggest that a mature holistic and sustainable model would take at least 10–15 years’ sustained effort.
This article expands on the author’s previous papers, with respect to the ADF’s rehabilitation services for ill and injured ADF members, prior to acceptance of their work-related conditions by the Department of Veterans’ Affairs (DVA).
Vocational rehabilitation in Australia
The Macquarie Dictionary defines ‘rehabilitation’ as: ‘the use of medical, social, educational or vocational measures or a combination of these to train or retrain someone who has a disability as a result of illness or injury’.8
The 2011 AFOEM Position Statement: Realising the Health Benefits of Work sets out the economic and social imperatives to ensure that everyone who is capable of working should be supported to do so.9 It reflects the fact that being at work has been recognised to be an important social determinant of health. The nature of that work is discussed in the 2013 AFOEM companion Position Statement What is Good Work?10
To date, the AFOEM Health Benefits of Good Work Consensus Statement has over 200 Australian signatories. These include organisations such as the Australian Federal Police, the Business Council of Australia, Comcare, Qantas, the NSW State Insurance Regulatory Authority and Virgin Australia.11 These signatories do not include the ADF.
Additional evidence since the 2011 Position Statement reinforces its assertion that work is good for optimising people’s health and wellbeing, and work absence because of illness or injury is not. Furthermore, it documents emerging evidence of the growing adverse effects that a lack of ‘good’ work has on mental health. It highlights the need for an emphasis on promoting recovery at work practices, which require better integration between health services and employers.12
The Royal Australasian College of Physicians (RACP), and its Faculties of Occupational and Environmental Medicine (AFOEM), Rehabilitation Medicine (AFRM), and Public Health Medicine (AFPHM), therefore, advocate the implementation of the RACP National Vocational Rehabilitation Policy.13 This document notes that there is a strong scientific evidence base for many aspects of vocational rehabilitation: in fact, it states that there is more evidence of its positive cost-benefits than for most health and social policy areas, which contributes to a sound business case for this approach.
The policy also describes how vocational rehabilitation is an idea and an approach as much as a formal intervention or service, based on the concept that being at work can be therapeutic and have a positive impact on health. This suggests that the barriers to vocational rehabilitation do not pertain to particular impairments, but to the lack of guaranteed access to customised plans of timely support and development.
As participation in the workforce requires ongoing good health and management of illness, injury and disability, the RACP National Vocational Rehabilitation Policy states that treatment services have an essential but not isolated role alongside vocational rehabilitation programs, as an enabler for workforce participation and productivity.14
Furthermore, the policy states that the principles and practice of vocational rehabilitation are fundamentally the same for work-related and other comparable health conditions, irrespective of whether they are classified as injury or disease. Work is not only a goal, it is generally therapeutic and an essential part of rehabilitation.
Finally, the RACP National Vocational Rehabilitation Policy refers to the urgent need to improve vocational rehabilitation interventions for mental health conditions, which have become the largest and fastest growing cause of long-term civilian incapacity. Promising approaches include healthcare that incorporates a focus on return to work, workplaces that are willing to accept such cases, and early intervention to support workers to stay at work in order to prevent long-term incapacity.
Civilian rehabilitation
As common health problems account for about two-thirds of civilian long-term sickness absence and incapacity benefits, the RACP National Vocational Rehabilitation Policy states that they should receive high priority. Among other considerations, this would mean that every health professional who treats patients with common health problems (such as musculoskeletal and mental health conditions) should also assume responsibility for their rehabilitation and occupational outcomes. This implies that general practitioners in particular should be at the forefront of civilian vocational rehabilitation.
Yet, the author has previously noted that neither the RACGP nor the Australian College of Rural and Remote Medicine (ACRRM) refer to a role for general practitioners with respect to rehabilitation, in particular, assessing the limitations posed by workplace hazards when returning ill and injured workers to work, or to assessing and monitoring their patient’s return to normal employment, or if this is not possible, ascertaining their suitability for alternative employment.15
The author has also previously noted that the ‘2016 Core Skills unit’ of the RACGP’s Curriculum for Australian General Practice, has very limited rehabilitation guidance. Although the ‘contextual units’ in military medicine and occupational medicine both refer to rehabilitation, it has also been noted that these documents only consist of 2–3 page summaries, with very limited guidance as to the actual skills required. Furthermore, as previously indicated, only 2.4 per cent of all presentations to civilian general practitioners in 2013–14 were work related.16
Hence, it seems reasonable to assert that even in the civilian setting, general practitioners lack the skills, experience and currency required to provide vocational rehabilitation. They can, however, identify patients who require specialist hospital- or workplace-based rehabilitation expertise, on the same terms as their other patients who require specialist treatment.
To this end, the author has previously described how specialist occupational and environmental physicians can not only set the pace and direction of workplace-based rehabilitation, but also negotiate with employees, employers, clinicians and other stakeholders to achieve optimal return-to-work outcomes.17
In addition, the mission of the AFRM is to train, accredit and support medical practitioners in the management of functional loss, activity limitation or participation restriction arising from illness and injury.18 Rehabilitation physicians have an essential role with respect to providing specialised hospital based rehabilitation services, following admission and treatment for acute illness or injuries resulting in significant disability, such as strokes, spinal cord damage and limb amputations.
The ADF Rehabilitation Program (ADFRP)
The ADF’s Defence Health Manual has extensive policy guidance for the provision of rehabilitation services for ill and injured ADF personnel. These references describe the ADFRP,19 the relevant governance arrangements,20 the health procedures for its delivery21 and the management processes for entitled ADF reservists.22
These references indicate that the attributes of a personalised rehabilitation plan for an ADF membermay include one or more of the following:
- Case management, utilising a Rehabilitation Activities Schedule, which is an agreement between the member, a Program Case Manager (PCM), and a Workplace Rehabilitation Representative (WRR).
- Functional capacity evaluations.
- Vocational assessment and rehabilitation.
- Clinical and psychological measures, such as in- and outpatient clinical services, aids and appliances, physical training, physiotherapy, counselling and psychosocial training.
However, a striking characteristic of all these references is that they describe the ADFRP as an occupational rehabilitation program, without any references to occupational and environmental physicians. It is therefore inferred that the ADFRP is premised on its clinical rehabilitation services being delivered by general practitioners, despite their aforementioned limitations.
Furthermore, rather than conceptualising vocational rehabilitation as an idea and an approach as much as a formal intervention or service (per the RACP National Vocational Rehabilitation Policy), these references are almost exclusively process-driven, and thereby reliant on large numbers of PCMs and WRRs. These processes are not only highly bureaucratic (and therefore expensive): they also preclude giving common health problems high priority per the RACP National Vocational Rehabilitation Policy, even though they may account for about two-thirds of preventable long-term sickness absence and incapacity benefits, in this case funded by DVA.
Regarding the latter, DVA spent $5.3 billion on treatment services for Service-related conditions in 2017–18, plus another $7.4 billion on non-health disability services and compensation.23 The RACP policy document therefore implies that effective rehabilitation services for current and ex-serving ADF members could save DVA up to $4.9 billion per year.
Rehabilitation and medical suitability for deployment
Before 2000, each Service had their own processes for assessing their members’ medical suitability for employment and deployment. In Navy’s case, all its members were assigned to one of eight Medical Categories (MEDCATs) such that:
- MEDCATs 1 to 4 were suitable for sea / deployment; MEDCATs 5 to 8 were non-deployable
- personnel with at least one medical restriction for more than 28 days were MEDCAT 2 to 8.24,25
All three single-service processes were replaced by the ADF Medical Employment Classification (MEC) System in 2000, which was last revised in 2011. ADF members with medical restrictions for more than 28 days now undergo a MEC Review, which assigns them to one of five MECs (divided into 20 sub-MECs), in accordance with the relevant joint and single-Service references.26,27,28,29
Although the current ADF MECs and previous Navy MEDCATs are not all directly comparable, they can be used to accurately ascertain the overall deployability status of Navy members, and the existence of at least one medical employment restriction for more than 28 days. Figure 1 describes the Navy MEDCAT status of all Navy members as of 30 June 1996, while Figure 2 describes the ADF MEC status of all Navy members as of 1 March 2019.
Figure 1: Navy Personnel MEDCAT Status as of 30 June 1996 (Per Cent)30
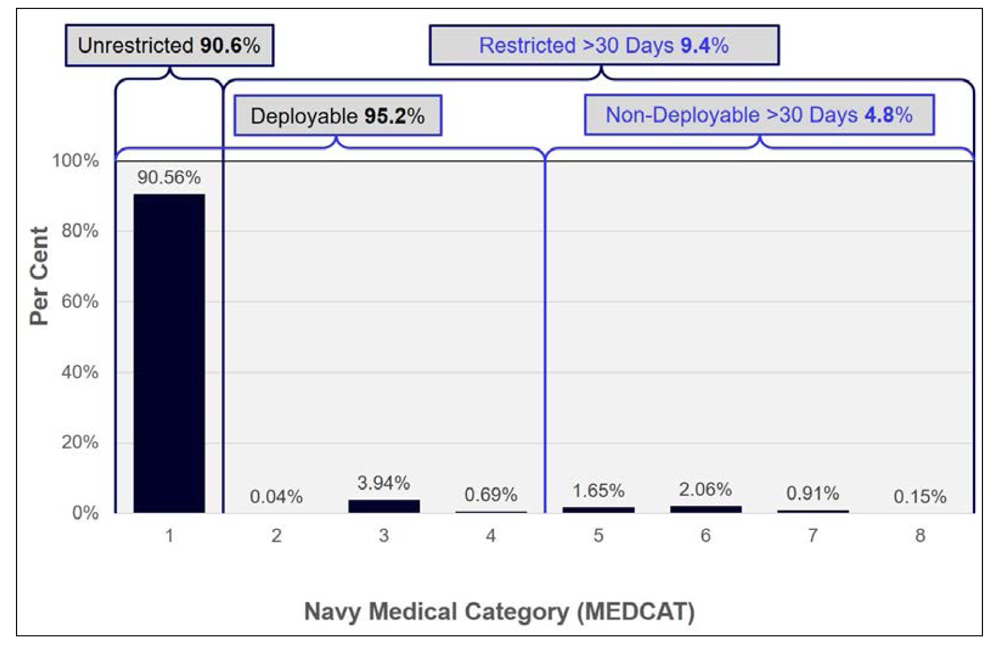
Figure 2: Navy Personnel MEC Status as of 1 March 2019 (Per Cent)31
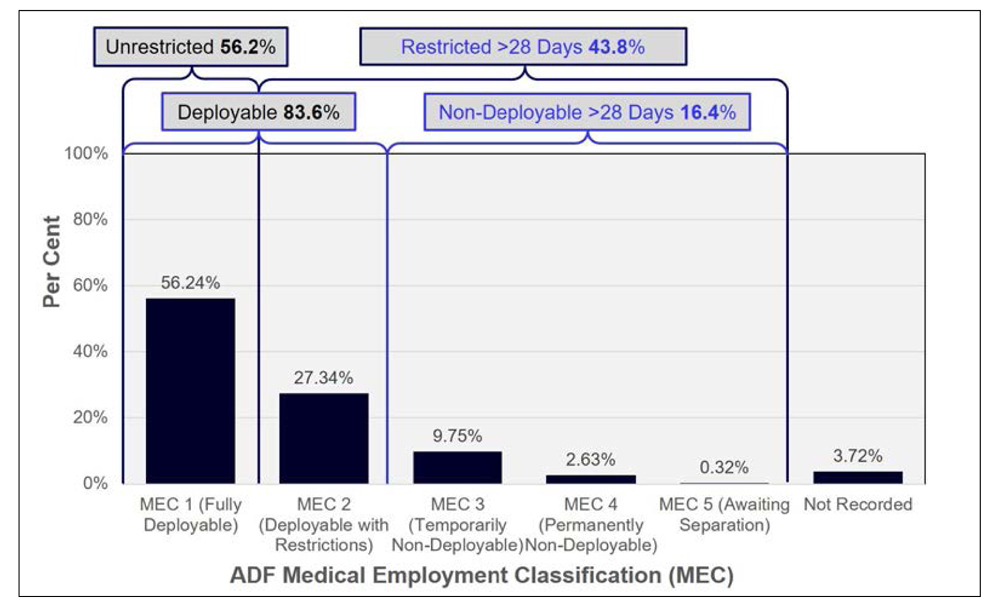
In short, Figures 1 and 2 indicate that the proportion of Navy personnel deemed not medically suitable for sea for more than 28 days increased from 4.8 per cent in 1996 to 16.4 per cent in 2019, while the proportion of Navy members with at least one medical restriction for more than 28 days increased from 9.4 to 43.8 per cent.
Though the reasons why clearly merit further investigation, they do suggest that the introduction of the ADFRP in 2006 and its subsequent iterations have not been particularly successful with respect to actually returning ill and injured Navy personnel to normal seagoing duties. Although comparable historical data has not been found for the other two services, it also seems likely that their medical deployability figures would be similar.
Rehabilitation and the ADF’s garrison health services
Previous papers describe how JHC provides primary health care and other health services for nondeployed ADF personnel, in accordance with the extant Garrison Health Service Level Agreement between the Vice-Chief of the ADF, and the singleService Chiefs.32 Although variations to the treatment services provided by the ADF can be authorised by the Defence Minister (in order to maintain fitness for duty while reflecting the facilities available), all Service Level Agreements to date have otherwise only specified compliance with the Health Insurance Act 1973, and the National Health Act 1953.
While this ensures that the standard of non-deployed treatment services for ADF personnel is comparable to that provided for the general civilian community, previous papers describe how JHC garrison health services did not include occupational and environmental physicians as part of their multidisciplinary rehabilitation teams: in fact, the garrison health service contract specified that all civilian primary care physicians require either a either a RACGP or ACRRM Fellowship. Although the contract has recently been amended to include occupational and environmental physicians, the shortcomings posed by the current ADFRP guidance, among the other deficiencies inherent to using a treatment-service-based health care model for a workforce population, will continue to preclude their utilisation at their full potential.
This is despite the author’s previous estimation (given the current absence of data),33,34 that:
- About 30–40 per cent of ADF clinical presentations are for generally preventable musculoskeletal injuries. Perhaps half of these cases are work related (typically related to manual handling or slips / trips / falls); the remainder are most likely sports-related.
- Another 30–40 per cent of ‘garrison’ clinical presentations are for generally preventable work related mental health issues. Perhaps half of these cases lack psychological robustness for whom the ADF has been a poor career choice; the remainder are quite likely to be just as psychologically robust as other ADF members are, but are not coping with excessively demanding or otherwise dysfunctional workplaces or personnel management practices.
Hence, perhaps half of all ADF primary care presentations are for work-related conditions, compared to this paper’s earlier statement that only 2.4 per cent of civilian primary presentations are work-related.35
In summary, the ADFRP has significant limitations in its current form, in particular its reliance on general practitioners to provide clinical rehabilitation services. Its effectiveness is further limited by bureaucratic processes that generally preclude their timely application to common health conditions that may account for about two-thirds of preventable long-term sickness absence and incapacity benefits funded by DVA. The three-to-fourfold increase in the proportion of Navy members with at least one employment restriction and/or considered non-deployable constitutes further evidence that the ADFRP is not working effectively with respect to returning them (and probably their Army and RAAF peers) to normal duties.
However, given the appropriate policy support among other enablers, military and civilian occupational and environmental physicians can complement garrison general practitioner colleagues with respect to the diagnosis and treatment of workplace-related musculoskeletal and mental health disorders, assessing medical suitability for employment and deployment, and managing workplace-based ADF rehabilitation. The same applies to AFRM practitioners regarding hospital-based ADF rehabilitation.
Conclusion
With ADF personnel arguably exposed to the most diverse range of occupational and environmental hazards of any Australian workforce, high rates of preventable workplace illness and injury indicate the need to improve the management of occupational and environmental health hazards, with better emphasis on prevention than treatment.
This suggests that the ADF’s health services should be premised on an occupational-health-based systems model, with revised fundamental inputs to capability that would lead to a range of genuinely holistic, sustainable and fit-for-purpose health services over the next 10–15 years.
Among its other attributes, the proposed model would reflect the National Vocational Rehabilitation Policy instituted by the RACP and its rehabilitation, public health, and occupational and environmental medicine faculties. This would entail including occupational and environmental physicians in the garrison health contract in order to complement garrison general practitioner colleagues, not only regarding the diagnosis and treatment of workplace related musculoskeletal and mental health disorders, and assessing medical suitability for employment and deployment, but also managing workplace based rehabilitation.
The proposed model would also reflect the 2011 AFOEM Position Statement: Realising the Health Benefits of Work, which sets out the economic and social imperatives to ensure that every ADF member who is capable of working would be supported to do so, or, if this is not possible, facilitating their timely and empathetic transition to suitable civilian employment.
As far as possible, the nature of ADF employment should also reflect AFOEM’s companion Position Statement: What is Good Work? by joining other employers in accepting that being at work is an important social determinant of health. It is essential that this be pursued not just as an end unto itself, but also to enhance ADF operational capability through improved personnel utilisation.
Disclaimer
The author used some of the information in this article to lead a RACP submission to the aforementioned Productivity Commission’s veteran’s rehabilitation and compensation inquiry.36 However, the views expressed in this article are his alone, and do not represent those of the RACP, the RAN or any other organisations mentioned.
Corresponding Author: Neil Westphalen,
neil.westphalen@bigpond.com
Authors: N Westphalen 1,2
Author Affiliations:
1 Royal Australian Navy Reserve
2 Navy Health Service, C/O Director Navy Health






