Preface
This article is based on a presentation the author delivered at the annual conference of the Australasian Military Medical Association, Canberra, October 2018.
Introduction
The aim of this paper is to provide an infantryman’s perspective on how the Army trains its medical officers. It is written in the first person because it is my story and my opinion. I spent 19 years as an infantry officer before starting my medical training. I completed General Service Officer (GSO) training through the Australian Defence Force Academy (ADFA) and the Royal Military College (RMC) Duntroon; followed by the suite of courses under the Army all-corps officer-training continuum (ACOTC) and the infantry regimental officer-training continuum. At all stages of my career as an infantry officer I felt satisfied and confident that the training I was provided prepared me for the roles and tasks that I was expected to fulfil. I assumed that this would also be the case with my career as an Army medical officer. However, the closer I got to the end of my training, the more I realised that this was not the case. This worried me. So much so that shortly before re-entering the Army as a doctor, I felt compelled to express my concerns in writing:
‘As an infantry company commander, I assumed that the Battalion Medical Officer had the skills and knowledge necessary to competently provide an appropriate level of care to soldiers in a field/deployed environment. Now, having almost completed my junior medical officer training, I realise that this assumption is wrong. The current paradigm for medical officer training does not provide an appropriate level of capability to Army.’
In this paper I intend to discuss what I believe are shortfalls in the way that Army trains its medical officers. It is an Army-centric discussion because after 31 years of service in the Army, I feel comfortable talking about Army training issues, but confess to knowing only a little about the Navy and Air Force. However, I believe that the issues I raise are also applicable to Navy and Air Force medical officers.
Medical Officer Training Shortfalls
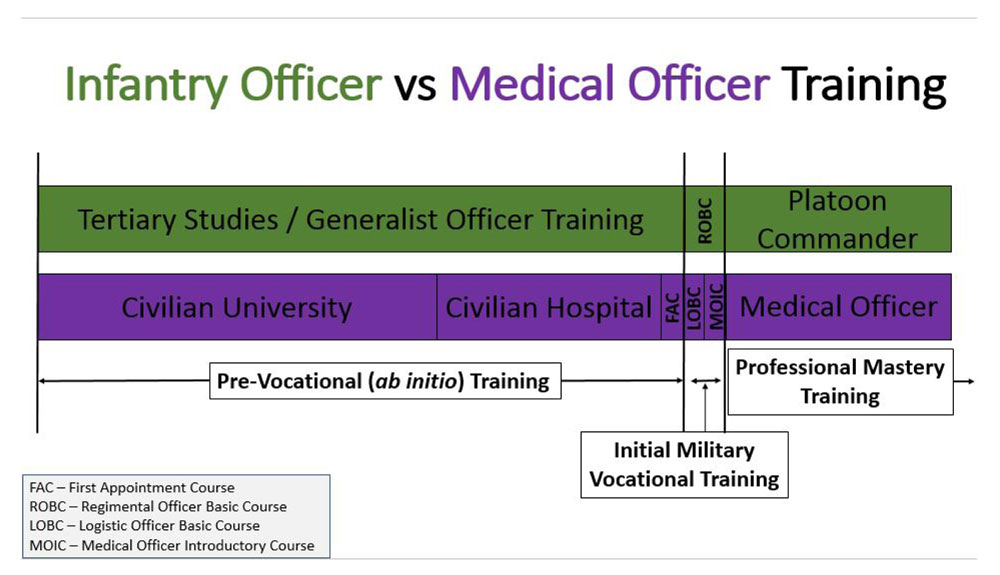
In general terms, infantry officer training and medical officer training follow a similar approach, illustrated in the schematic above. They both start with pre-vocational training—tertiary studies (for many GSO officers) followed by ab initio military training. The aim of pre-vocational training is to provide the knowledge and skills required to serve as a generalist officer within Army. This is followed by initial military vocational training, which provides training specific to your primary role within Army. Finally, professional mastery training is the ongoing professional training and development to make you an expert in your current and subsequent roles, and more broadly within the military. For medical officers, I believe there are shortfalls in each of these three important areas of training and development.
Pre-vocational Training Shortfalls
In 2015, the Australian Health Minister’s Advisory Council completed a review into the training of junior doctors in Australia. The review identified significant shortfalls and concluded that:
‘The weaknesses of the current internship model significantly undermine its longer term fitness for purpose. In the absence of meaningful structural changes, the internship will become further out of touch with modern health care practice and the quality of the learning experience further diminished, with implications for capability development, overall length of training and return on investment.’1
The review’s findings should have been of significant concern to Army (and the ADF) because this is the foundation training that Army medical officers receive. The Army medical officer’s workplace is far more demanding than the public health system. If the current model for training junior doctors does not meet the needs of the public healthcare system, it most certainly does not meet Army’s needs.
What has Army done about the findings of this review? Until recently, nothing. However, from 2020, it is intended that the Army (and ADF) medical officer-training paradigm will change, with all medical officers completing an additional year of pre-vocational training prior to commencing their service as a uniformed medical officer. From an infantryman’s perspective, this initiative was a long time coming. If an independent review of Army GSO officer training found that the Army’s officer-training continuum did not adequately prepare GSOs to be platoon commanders, the Army would not have waited five years to address the problem.
Within the pre-vocational training period, there are stark differences between how Army trains a GSO, and the training that medical officers receive. For Army trainees—soldiers and officers alike—training is scripted and micromanaged at an organisational level, based on a clear training endstate that is articulated in nested mission statements. Training is then directed towards capability, and facilitated through training agreements between training organisations. For example, between ADFA and RMC, and between RMC and the School of Infantry. Professional development opportunities are integrated into GSO pre-vocational training—adventure training, motivational training and various other training opportunities—to enhance the GSO officer’s development and, importantly, inculcate a sense of esprit de corps among trainees, and between the GSO and Army.
This does not happen for Army medical officers. Army assumes that the training provided by civilian universities and public hospitals meets Army’s capability requirement. We know this is not the case from the findings of the review into intern training. Further, with no training agreement in place between Army and the training hospitals, Army’s junior doctors find themselves randomly assigned to the geriatric or oncology wards, instead of gaining more relevant skills and experience in emergency medicine and anaesthetics. As an infantry company commander, I assumed the battalion medical officer could manage an airway and deal with trauma, not manage dementia and oversee chemotherapy. Finally, Army medical officers receive no professional development opportunities from Army during the pre-vocational training period.
In my opinion, Army’s pre-vocational training of its GSO officers represents world’s best practice. Why don’t we apply the same approach to medical officer training?
Initial Military Vocational Training Shortfalls
Initial military vocational training provides the necessary additional training so a junior officer is job ready when they assume their first appointment. As an infantry Lieutenant, upon completion of my Regimental Officer Basic Course (ROBC), I was trained to use every weapon and every piece of equipment I was expected to employ as an infantry platoon commander. For each weapon or piece of equipment, I spent hours learning about tabulated data, pulling it apart and putting it back together again, and using it in a variety of settings. I had participated in and led platoon attacks, platoon ambushes, defensive and stability operations tasks. I learnt to write range instructions and became qualified to conduct range practices. I was job ready, and seven days after marching into my first unit, I deployed with my platoon on operations in Somalia.
As a medical officer this did not occur. Before marching into my unit I had not been trained by Army to use the life-saving equipment that I was expected to use as a medical officer in a treatment team. I could operate a radio and call for artillery fire, but I could not use the ventilator or MRX heart start monitor/defibrillator. I could lead a platoon attack, but had not been taught how to establish and lead a treatment team in the field. Similarly, I received no training in performing a periodic health assessment, had not conducted a Unit Military Employment Classification Review (UMECR), or participated in a unit welfare board. I was not job ready. Under the current paradigm, it takes an Army medical officer about 12 months to become job ready (ML2) in a decentralised, disjointed and uncoordinated approach to gather mandated qualifications and training experiences. It takes Navy and Air Force
medical officers even longer!
Professional Mastery Training
In 2003, the ADF introduced a competency-based salary structure for its medical officers. In its submission to the DFRT, the ADF stated that, ‘The requirement to operate independently at a relatively junior level requires significant upskilling of ADF medical officers’.2
In my short time as an Army medical officer, compared with my civilian general practice (GP) registrar peers, I haven’t received ‘significant upskilling’. In fact, as an Army medical officer, I think I have experienced skills degradation. This is the paradox of being an Army medical officer. As an infantry officer, the more time I spent in the field, the better I became at my job. However, as a medical officer, the more time I spend in the field, the more likely it is that my knowledge and skills will degrade. The same can be said for prolonged periods of service in a garrison health centre. Working in garrison health is a key role for Army medical officers through which they gain very good exposure to occupational medicine and relevant experience in primary care. However, the depth and breadth of clinical presentations is not sufficient to meet the training and development requirements of Army GP registrars, or to maintain clinical knowledge and skills as a (relatively junior) recently Fellowed GP. It is for this reason that the Royal Australian College of General Practitioners (RACGP) changed its policy on the vocational training requirements for ADF GP registrars, limiting the amount of garrison health time that ADF GP registrars can count towards their GP training requirements.
As an infantry officer, I stepped through a logical sequence of all-corps and infantry-specific training courses, designed to enhance my professional mastery and prepare me for subsequent and more challenging appointments, both as an infantry officer, and more broadly as an officer in the ADF. Now, as a medical officer, I wonder why we teach Army doctors how to plan brigade offensive operations—a role that they are specifically prohibited from performing under the Geneva Conventions—but we don’t release the doctor to upskill in emergency medicine or anaesthetics. We teach them to be an Operations Officer (OPSO – G3), but not the Senior Medical Officer/Health Planner (G07). The Army has an excellent individual training system… if you’re a GSO. Frankly, there’s not much on offer that contributes to the professional mastery of medical officers, or prepares them for the workplace described in the Army Medical Officer Employment Specification.
In summary, I believe there are three significant problems with the current approach to Army medical officer training:
- The pre-vocational training that Army medical officers receive in the public hospital system is deficient.
- The initial military vocational training Army provides to medical officers is deficient.
- The clinical and military professional mastery training that Army medical officers undertake does not adequately meet the workplace requirement.
Improving Army Medical Officer Training How should we improve medical officer training? We should apply the same approach that is applied to GSO officer training. Just as we send all Army cadets to RMC, in the pre-vocational training period, we should cohort our junior doctors in a single hospital during PGY1 and PGY2, with a training agreement that provides them with the hospital terms that best meet the Army’s capability requirement. With the medical officers all in one place, it provides opportunities to build esprit, conduct professional development and military orientation activities, and even bring forward subsequent short military training courses.
More importantly, we need to fix the deficiency in prevocational clinical training, so that medical officers are adequately prepared to be military clinicians. There is a need to frontload clinical training into the training model, by using PGY3 to provide a full year of primary care training. This should be a mix of general practice and emergency medicine training completed under similar arrangements to the ROSO-neutral training conducted in PGY1 and PGY2. Doing so will mean that medical officers are better clinicians when they start in Army, which means our soldiers will get better care. [The proposal to introduce an additional pre-vocational clinical training year (PGY3) is a key recommendation arising from the recent strategic review of ADF medical officer training and retention.]
We should also provide professional development funding to medical officers during their hospital training years—this is the ideal time for them to gain skills and complete training courses that are directly related to the Army workplace, and/or mandated in Army’s policy on clinical readiness standards.3 To wait until a medical officer achieves ML2 before providing professional development funding results in three years of wasted opportunity.
Next, we have to expand our initial military vocational training so that medical officers join their unit job ready. Current initial military vocational training—the Logistics Officer Basic Course (LOBC) and Medical Officer Introductory Course (MOIC)—provides four weeks of training. However, to be deemed ‘deployable’, medical officers are then required to complete a number of other training courses and activities, delivered in a disaggregated and decentralised approach. From a resource perspective, this is grossly inefficient. From a capability perspective,
this approach delays progression to ML2, resulting in a poor return on investment for Army. The fundamental problem, however, is that these courses do not provide medical officers with the skills and knowledge required to do their job.
By way of comparison, initial military vocational training for medical officers in the British Army is six months duration. We don’t need a six-month course, but we need more than the four weeks we currently have. As a minimum, the MOIC should be expanded to incorporate all of the externally delivered training—both mandatory and desirable—
such as the Emergency Management of Severe Trauma (EMST) Course, Rotary Wing Aeromedical Evacuation (RWAME) Course, Acute Mental Health on Operations (AMHOO) Course and Occupational Medicine. However, military vocational training should also be expanded to address the shortfalls in Army medical officer training that I discussed previously. Intuitively, I believe initial military vocational training for medical officers requires about 10–12 weeks duration. This represents an additional six weeks of training, of which at least three weeks is currently delivered under a disaggregated, decentralised approach. I also firmly believe that this should be a Joint course—the training requirements listed above (and the shortfalls I identified in Army medical officer training) apply to all ADF medical officers.
Finally, with respect to professional mastery training, Army should formally recognise that its capability requirement is for a ‘rural generalist’. The Army medical officer-training continuum should incorporate completion of an advanced skill in a relevant extant discipline (e.g. Emergency Medicine, Anaesthetics, Mental Health, Obstetrics), or a bespoke advanced skill qualification in military medicine (e.g. Pre-Hospital and Retrieval Medicine). We also need to critically review whether Army medical officers should train under the RACGP or the Australian College of Rural and Remote Medicine (ACRRM). While both colleges are accredited for GP training, as
a dual-pathway registrar who has completed the key assessment requirements for each college, it is clear that ACRRM training is more closely aligned with the Army capability requirement. The reasons for this include a greater focus on pre-hospital care, the requirement to complete six months of emergency medicine experience during fellowship training, and ACRRM’s overarching goal to prepare doctors to work independently in a resource-constrained environment. These three features of the ACRRM curriculum epitomise the Army medical officer’s workplace beyond the garrison health environment. The additional requirement for ACRRM registrars to complete an advanced skills training year (prior to fellowship) would significantly enhance the capability of Army medical officers. In the past, the requirement to be released for a year of advanced skills training has prevented Army medical officers from completing training through ACRRM. However, proposed changes to ADF medical officer training (i.e. the PGY3 initiative and other changes that may arise from the strategic review of ADF medical officer training and retention) will allow Army medical officers to train as rural generalists and remove the barriers that have previously prevented Army medical officers training through ACRRM.
We also need a relevant training continuum for both military and clinical training—Army needs to professionalise and upskill its medical officer clinical workforce. The current military training continuum has medical officers completing the same training courses as GSOs, albeit that they don’t complete all modules in some courses. This approach is predicated on the assumption or assertion that health and logistics training meet a medical officer’s role-specific training requirement, as does GSO allcorps training. This is not correct. There is a need for a medical officer advanced course and this should (also) be a tri-Service course.
Similarly, we need a directed or guided clinical training continuum with a plan to achieve it. The current paradigm assumes that gaining a GP fellowship completes organisational and individual clinical development requirements. It does not. A clinical training continuum is not the Medical Specialist Program (MSP) or a fellowship in medical
administration. Both of these may be elements within a clinical training continuum, but we need to do something for the 90% of medical officers who won’t pursue either of these options. As a minimum, a clinical training continuum should include a year of advanced skills training—whether this is used to facilitate progression from FRACGP to FARGP (Fellowship in Advanced Rural General Practice), to meet the ACRRM training requirement, or simply to provide a level of capability that actually represents what we expect Army medical officers to be able to do.
Conclusion
To conclude, there are a number of similarities between infantry officer training and medical officer training. There is also a significant and fundamental difference. As an infantry officer, my training focused on the most dangerous role—conventional warfare—and was adapted for the most likely—stability, peacekeeping and humanitarian operations. The reverse is true for medical officers. Our training is focused on the most likely role—coughs, colds and sprained ankles—and does not adequately prepare us for the most dangerous role. In my opinion, this is a breach of the unwritten contract that we have with supported commanders. As I stated at the beginning of this paper, as an infantry company commander deployed on operations in East Timor, I assumed that the battalion medical officer was sufficiently trained to provide an appropriate level of prehospital emergency care to my soldiers. Now, having completed my training as an Army medical officer, I know that this assumption is wrong. Hopefully the strategic review into ADF medical officer training addresses the problems identified here.
Corresponding author: Robert Worswick robert.worswick@defence.gov.au
Authors: R Worswick






