Abstract
Introduction
This study was designed to document the morbidity of a population of Australian military servicemen and women.
Methods
The study was conducted in the outpatient departments of No 6 RAAF Hospital, at Laverton, Point Cook, and Defence Force Health Centre, Melbourne. The patients studied were male and female members of the Royal Australian Air Force (66%), Army (25%), and Navy (9%), who were almost all working in office occupations.
The doctors coded the problems managed at all consultations during 1993-94, using a sub-set of ICD-9 (CM), based on the International Classification of Health Problems in Primary Care.
Results
Information was recorded from 19,981 consultations. At 1808 consultations, two problems were managed and at 202 consultations, three problems, giving a total of 21,993 problems. There was a high incidence of respiratory disease, medical examinations and musculoskeletal disorders and a low incidence of blood, reproductive and congenital/perinatal disorders.
Discussion
The study has shown that a wide range of disease is present in the Services, providing a good breadth of experience for Defence Force doctors. A number of recommendations are made regarding the process of coding morbidity.
Key Words
Morbidity. Health Surveys, Defence Forces, Military Medicine, General Practice, Disease Classification Systems, Primary Care.
Introduction
In 1983, the Australian National Health and Medical Research Council recommended increased collection of health care information on which policy decisions could be based and development planned. In 1985 the Australian and New Zealand Society for Epidemiology and Re search in Community Health identified information on morbidity as a key requirement for planning of improved health care and continuing education for medical practitioners.
The Defence Forces are well placed to carry out clinical research related to morbidity. They have a well-documented population with baseline data recorded at the time of recruitment. It should, therefore, be possible to assess incidence and prevalence of disease and injury and identify occupational risk factors. The effectiveness of preventative medical strategies in conditions such as obesity hyperlipidaemia and hearing loss could also be studied.
The implications of this data collection for future planning are considerable. This could include analysis of time lost through accident and illness, the effectiveness of recruit medical examinations in screening out significant problems and the effect of conditions such as asthma on the member’s fitness for deployment. Without recording morbidity accurately for a lengthy period, any conclusions drawn from data collection are at best only an impression.
Studies of morbidity among the military forces of the world have been carried out over the years but most have looked at isolated incidents. Examples include an outbreak of diarrhoea in Dutch servicemen in Zaire, 1 and streptococcal disease among US Army trainees. 2 Another study recorded morbidity and medical supply usage during deployment of 1159 troops to Thailand for 6 weeks, to aid planning for future exercises.3
Injuries and illnesses, occurring in a group of 649 completing their basic training over a period of six weeks, demonstrated that cigarette smoking and lack of physical fitness were related to increased morbidity. 4 Studies of morbidity during the Gulf War included a comparison of the incidence in each sex of seven general conditions such as acute gastrointestinal disorders. 5
There is however little published data on the overall health of serving members and few longitudinal surveys. Three recent studies aim to address this question.
Fitzpatrick documented 5,793 consultations over a one-year period in an aviation brigade of 1220 persons, comparing medical attendances by aircrew and supporting staff. S Zwart analysed the records from 15 275 medical consultations with aviators recorded over several years at 18 United States Air Force bases. 7The British Army Morbidity Surveillance study (J95), launched in 1996, is a universal comprehensive sickness monitoring system. It aims to collect data on the reasons for sickness and injury attendances. working days lost, referrals and admissions to military or other facilities (personal communication – Lt Col S A St J Miller, Royal Defence Medical College London).
Our study was conceived after an audit was carried out in 1990 of 100 randomly selected medical records of patients presenting to the Outpatients Department of 6 RAAF Hospital. 8 This revealed a wide range of complaints and stimulated a large-scale study of all patients presenting to the Department.
The aim of this ongoing study is to ascertain morbidity patterns and help identify key health problems in serving members. This paper presents the results of our study. A separate paper will compare our findings with Australian general practice.
Methods
Setting and Patients
The project was undertaken by the doctors working at 6 RAAF Hospital in 1993-94. The hospital has an inpatient unit of 35 beds and an outpatient unit which functions as a general practice for the service personnel on the Laverton Base. The hospital also has outpatient branches at Defence Force Health Centre, Melbourne and RAAF Base Point Cook.
During the study, medical care was provided for 3 350 staff, of which 66% were Air Force, 25% were Army and the balance Navy members. Males accounted for about 76% of the personnel. The members who formed the study population worked mainly in office-based occupations, in contrast to personnel at operational bases, where there are more industrial occupations.
Unlike the defence forces of the United Kingdom and the United States of America, family members in Australia are not treated by service medical practitioners, so our patients are aged 18-55 years.
Data Collection
After each consultation, the doctor selected a diagnostic code for each problem managed. A maximum of three codes was then written on the appointment sheet and later added to a computer database.
The coding system was a subset of the International Classification of Diseases – Clinical Modification (ICD-9-CM). 9 Which is used for all medical coding in the Defence Forces.
Because it would be used by doctors unfamiliar with the complexities of coding, a brief list of codes was considered desirable. The subset chosen was based on the International Classification of Health Problems in Primary Care (2nd Edition).10
A number of ICD-9-CM codes were added to cover sporting injuries and medical examinations in more detail, as these diagnoses are common in the services.
The list used contains 376 codes and was printed on a laminated double-sided A4 sheet, with a copy for each doctor. Training sessions were conducted to encourage uniformity of coding. The authors were available to discuss any coding queries.
Results
Number of Problems Managed
There were 21 993 problems managed at 19 981 consultations. At 1,808 consultations, two problems were recorded, and at 202 consultations three problems. There was a wide range of problems with 347 different problems selected from a list of 376.
The data was analysed by sex and by the age groups 18-24, 25-44, and 45-55. The distribution of the problems among these groups is shown in Figure l. Although 76% of the study population is male, they represented only 67% of the problems.
Problem Groups
The distribution of the problems managed across the ICD-9 (CM) chapters is shown in Figure 2.
A list of the commoner problems managed is shown in Table 1. These were selected because the percentage of each was equal to or greater than 0.5% of all problems managed in the whole study. The numbers shown under each sex-age group represent the percentage of the problem in that particular group.
Note that the term “Med/Surg Procedure without diagnosis” includes wound dressings and cosmetic surgery.
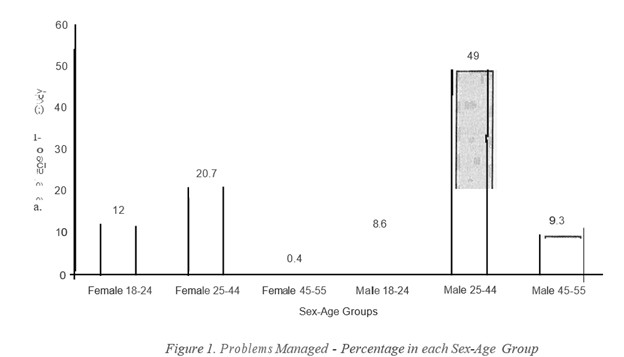
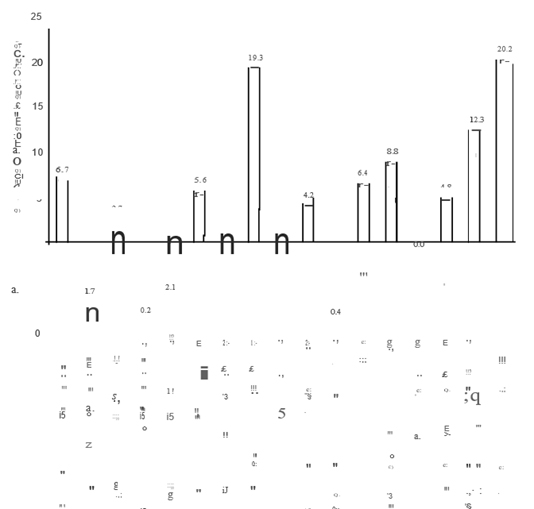
Figure 2. Problems Managed – Percentage in each JCD – 9 (CM) Chapter
| ICD-9(CM) Chapter | Problems Managed | Female Age Groups (percent) | Male Age Groups (percent) | ||||
|---|---|---|---|---|---|---|---|
| (where incidence for “All Groups” >= 0.5%) | n=2636 | n=4557 | n=83 | n=1888 | n=10777 | n=2052 | |
| Infectious Diseases | Presumed Infectious Intestinal Disease | 3.3 | 4.1 | 0.0 | 4.1 | 2.5 | 1.4 |
| Warts, All Sites , including genital | 1.6 | 0.6 | 0.0 | 1.1 | 0.9 | 0.9 | |
| Dermatophytosis & Dermatomycosis | 0.6 | 0.2 | 0.0 | 1.5 | 1.1 | 0.9 | |
| Viral Infection NEC | 0.6 | 0.6 | 0.0 | 1.2 | 0.9 | 0.3 | |
| Neoplasms | Benign Neoplasm Skin, inc!Naevi | 0.9 | 0.9 | 0.0 | 0.7 | 0.8 | 0.9 |
| Endocrine, Metabolic | Ovenveight (BMI > 26.9) | 0.8 | 1.3 | 6.0 | 0.8 | 1.7 | 2.1 |
| Lipid Metabolism Disorders | 0.0 | 0.1 | 0.0 | 0.2 | 0.7 | 3.5 | |
| Mental Disorders | Depressive Disorder | 0.0 | 1.6 | 0.0 | 0.1 | 0.4 | 0.7 |
| Nervous System | Refractive Errors | 1.2 | 0.9 | 1.2 | 0.8 | 1.5 | 2.5 |
| Migraine | 0.6 | 0.6 | 0.0 | 0.6 | 0.4 | 0.8 | |
| Conjunctivit is & Ophthalmia | 0.6 | 0.5 | 0.0 | 0.5 | 0.7 | 0.6 | |
| Other Eye Diseases | 0.3 | 0.4 | 0.0 | 0.5 | 0.6 | 0.5 | |
| Circulatory Disorders | Hypertension, Uncomplicated | 0.2 | 0.3 | 7.2 | 0.2 | 1.4 | 7.1 |
| Resph’3tory | Acute Upper Respir Tract Infection | 8.1 | 8.7 | 12.0 | 10.2 | 10.4 | 7.1 |
| Hay Fever | 2.3 | 2.4 | 2.4 | 2.3 | 2.6 | 2.3 | |
| Bronchitis & Bronchiolitis, Acute | 1.3 | 1.1 | 4.8 | 2.4 | 2.0 | 1.6 | |
| Sinusitis, Acute & Chronic | 1.4 | 1.5 | 2.4 | 1.5 | 1.8 | 2.1 | |
| Asthma | 1.6 | 1.1 | 0.0 | 1.7 | 1.2 | 2.0 | |
| Laryngitis & Tracheitis, Acute | 1.1 | 0.9 | 0.0 | 0.6 | 0.9 | 0.7 | |
| Acute Tonsillitis & Quinsy | 0.9 | 0.6 | 0.0 | 1.1 | 0.8 | 0.5 | |
| Genitourinary | Vaginitis, Vulvitis NEC | 2.5 | 1.9 | 1.2 | 0.0 | 0.0 | 0.0 |
| Skin | Other Skin Disease NEC | 0.9 | 0.6 | 1.2 | 1.3 | 1.0 | 0.8 |
| Eczema & Allergic Dermatitis | 1.1 | 0.9 | 3.6 | 0.8 | 0.9 | 0.7 | |
| Keratosis (Solar, Seborrh, Senile) | 0.2 | 0.2 | 0.0 | 0.2 | 0.8 | 1.4 | |
| Boil & Cellulitis Inc!Finger & Toe | 0.6 | 0.5 | 0.0 | 0.7 | 0.8 | 0.6 | |
| Other Infections Skin/Subcutaneous | 0.4 | 0.2 | 1.2 | 0.6 | 0.6 | 0.6 | |
| Musculoskeletal | Back Pain W/0 Radiating Symptoms | 1.0 | 1.3 | 3.6 | 1.4 | 1.8 | 2.1 |
| Back Pain With Radiating Symptoms | 0.5 | 0.7 | 0.0 | 0.4 | 1.3 | 1.4 | |
| Pain Or Stiffuess In Joint | 0.4 | 0.5 | 0.0 | 1.0 | 1.1 | 0.9 | |
| Chronic Internal Knee Derangement | 0.5 | 0.3 | 0.0 | 2.2 | 0.6 | 0.4 | |
| Shoulder Syndromes | 0.1 | 0.2 | 0.0 | 0.1 | 0.7 | 1.2 | |
| Cervical Spine Syndromes | 0.5 | 0.4 | 1.2 | 0.3 | 0.5 | 0.8 | |
| Sign, Symptom, IU-defmed | Headache | 1.3 | 0.9 | 0.0 | 0.5 | 0.7 | 0.2 |
| Abdominal Pain | 1.4 | 0.7 | 0.0 | 0.5 | 0.6 | 0.4 | |
| Injuries, Adverse Effects | Sprain/Strain All Sites | 6.4 | 5.7 | 3.6 | 10.8 | 8.5 | 3.6 |
| Fracture, Any Site | 0.9 | 0.5 | 1.2 | 2.3 | 1.1 | 0.5 | |
| Bruise, Contusion, Crushing | 0.9 | 0.6 | 1.2 | 2.3 | 1.0 | 0.3 | |
| Lacerations | 0.5 | 0.3 | 0.0 | 1.2 | 0.8 | 0.5 | |
| Pl’eventive, Social | Medical Examination | 4.9 | 6.2 | 2.4 | 10.0 | 8.0 | 6.2 |
| Advice & Health Instruction | 2.4 | 2.8 | 1.2 | 2.8 | 2.7 | 3.2 | |
| Prophylactic Immunisation | 0.8 | 1.7 | 1.2 | 1.6 | 3.3 | 2.1 | |
| Med/Surg Procedure W/0 Diagnosis | 0.6 | 1.0 | 1.2 | 0.7 | 2.8 | 3.0 | |
| Oral Contraceptives | 6.2 | 4.5 | 1.2 | 0.0 | 0.0 | 0.0 | |
| Pap Smear | 4.0 | 4.2 | 4.8 | 0.0 | 0.0 | 0.0 | |
| 1.5 | 1.6 | 0.0 | 0.0 | 0.0 | 0.0 |
Notes: NEC = not elsewhere classified W/O = without
Blood, Digestive, Perinatal and Reproductive Chapters are not shown in this Table because of low numbers
Table I. Common Problems Managed
Discussion
Problems Managed
The most common group of problems managed was Preventive & Social, which comprised mainly medical examinations. In the Services, these are carried out on recruitment, re-engagement, change of employment trade, application for a license to drive heavy vehicles, and discharge from the service. Also, all RAAF members have a periodic medical 5-yearly, while Army members have one 3-yearly until age 35 and thereafter annually, and Navy members 3-yearly.
Examinations range in complexity from checking blood pressure, height and weight, vision and hearing through to the RAAF Periodic Medical which includes a full physical examination, ECG. spirometry and a serum lipids/liver function/glucose/urate screen.
The second most common group was Respiratory. These conditions may have a higher consultation rate in the Services than in the community because members must see a doctor to obtain a prescription for common medications used for symptomatic relief of respiratory infections. This requirement is partly to ensure rapid recovery of the patient through supervision of treatment, and also to control costs because medications are free.
The third and fourth most common group of problems were Musculoskeletal and Injuries & Adverse Effects. The prevalence of these conditions reflects the requirement by the Services for high levels of physical fitness. This results in a high frequency of sporting injuries particularly ankle, knee and spinal strains.
Sex-Age Groups
Analysis of the data by sex-age groups reveals a similar pattern of problems managed with some notable exceptions.
In young males, the commonest problems managed were sprains and strains. Upper respiratory tract infection (URTI) was almost as common and was the commonest problem in all other groups. Other infectious diseases, particularly gastrointestinal, tinea, warts and other viral infections figure prominently in this group.
The 25-44-year male group formed the largest subset and produced almost 50% of all problems managed. Major complaints were respiratory infections and physical injury.
In older males, whilst respiratory infections are still the commonest cute problem, chronic conditions are more frequent than in younger members. Hypertension ranks with URTI as the major cause for attendance. Eye refractive errors were three times more common than in the youngest group. Lipid disorders and obesity were also prominent. In contrast, visits due to physical injury, viral and gastrointestinal infections were much less frequent than in the younger groups.
Young females, like young males, attended mainly with URTI, physical injury and gastrointestinal infection. Visits for contraception and vulvovaginitis were more common than in the older group.
As in the case of males, the 25-44-year-old females attended more frequently than the older and younger groups combined. The three commonest problems were similar to the younger members, whilst high fever, troublesome in all groups, was also a common reason for presenting. Attendances were similar to the younger group except for headache and abdominal pain, which were less common.
Older women presented only 83 problems in total. Whilst no significant conclusion can be drawn from this group, attendances mostly related to respiratory infections and conditions associated with ageing – hypertension, overweight and back pain. In addition, skin diseases were a cause of frequent consultation. Cervical spine syndromes – perhaps related to poor posture – were also more commonly seen, whilst sporting injuries were less frequent.
Summary
In summary, it is interesting to note the changes across age groups for certain conditions. In males, there was a noticeable decrease in frequency with age for infectious disease, chronic internal knee derangement and injuries. There was an increase with age for excessive weight, lipid disorders, hypertension, refractive errors, keratoses, back pain and cervical spine syndromes.
In females, excessive weight, hypertension, sinusitis and back pain increased with age, whereas vaginitis, sprains/strains and oral contraceptive usage declined. Changes in prevalence for other conditions were not as marked.
When all groups of both sexes are combined, we note that the largest group of problems were acute respiratory infections. Sprains and strains, medical examinations, advice and health instruction and immunisations were the next most common, reflecting the emphasis on preventive medicine by the services.
The study has shown that a wide range of disease is present in the Services, providing a good breadth of experience for doctors working in the Defence Forces. It has permitted a com parison with morbidity in similar age and sex grouped individuals in the community. which will be reported separately. Further, it will enable us to identify at-risk groups, permit critical evaluation of our treatment and hopefully will ultimately lead to improved health status in Defence Force personnel.
Classification Systems
The authors noted a number of problems with classification systems. For example, some conditions such as headache, skin naevi, respiratory infection, and viral illness can be classified under a number of different codes, depending on the preference of the doctor choosing the diagnosis. It is a problem which can be reduced by careful attention to classification systems, and education of the doctors in coding nuances.
Classification is best done by the doctor seeing the patient, so it is important that the system be as simple as possible, to reduce time spent coding. It would also be preferable for the doctor to code the problems directly into a computer in the consulting room. This may be best achieved by adding diagnosis coding to computer prescription systems which are likely to be used by doctors because of the excellent drug interaction and advice systems available today.
Another problem was the high number of patients with no sex and/or birth date recorded. The missing data was late added by the authors. This source of error could be reduced greatly if a CD-ROM was provided each month with a full list of Defence Force members, including their sex and date of birth.



