Introduction
This paper—and the series to date and to follow—is based on conclusions reached in a previous series by the author regarding occupational and environmental medicine in the ADF.61,2,3,4,5,6,7,8,9,10,11 The previous series describes why high workplace illness and injury rates confirm the need to improve the management of hazards associated with ADF workplaces, with better emphasis on prevention. To this end, a submission by the Royal Australasian College of Physicians to the 2019 Productivity Commission inquiry into veterans’ health advocated that this would be best achieved by premising the ADF’s health services on a systems-based occupational health strategic model.12
Doing so would require reassessing the Fundamental Inputs to Capability (FICs)13 for both Joint Health Command (JHC) and Defence’s Work Health and Safety Branch. The previous series explained how the current state of the ADF’s occupational and environmental health services and the small number of civilian specialist practitioners within the Australasian Faculty of Occupational and Environmental Medicine (AFOEM) indicate that implementing a mature holistic and sustainable model would take 10–15 years’ sustained effort.To that end, this new series explains how the ADF’s FICs should be adapted to support health services founded on a systems-based occupational health strategic model. In so doing, it refers extensively to the previous series.
This paper aims to provide an overview of the three elementally distinct yet intrinsically interlinked missions of military health services, the functions and roles necessary to conduct these missions, and the FICs required to enable these functions and roles.
The elemental missions of military health services
A previous paper describes what the distinguished WWI veteran and medical historian Colonel Arthur Graham Butler referred to as the three ‘allegiances’ of military health services and how and why these would now be referred to as their elemental and enduring ‘missions’:
- The ‘alleviating suffering’ allegiance, or what we would now call the ‘treatment services’ mission
- The ‘command’ allegiance, or what we would now call the ‘enabling operational capability’ mission
- The ‘national’ allegiance, what we would now call the ‘civilian reintegration’ mission.14
Military health services have three missions rather than one because of how they interact with each other. This explains why the functions and roles of all health personnel at all levels within military health systems entail managing patients—not just treating them.
For example, consider LSET Bloggs, who presents with ear pain and discharge. The tasks to be conducted by her primary health care provider are not limited to taking a history, examining the ear, diagnosing her burst tympanum and prescribing her antibiotics; were that the case, a military health service would not be required. Rather, the healthcare provider also needs to think about the impact of Bloggs’ diagnosis on her ability to do her job and the effect of her job on her diagnosis and treatment. This is problematic unless the healthcare provider comprehensively understands what her job entails. Although this can be straightforward, matters rapidly start becoming complicated if Bloggs’ ship is sailing in an hour’s time, which is where the second mission—enabling operational capability—becomes relevant, especially if her job (such as maintaining an obscure combat subsystem), renders her a ‘ship-stopper’. The relevance of the third mission—facilitating her eventual return to the civilian community—pertains to documenting the work-relatedness of her otitis, such as having recently undertaken her secondary ship’s diver job in filthy water.
For another example, let us consider an Air Force aeromedical evacuation team that has just landed in a remote part of Vanuatu to evacuate an injured civilian as part of a humanitarian aid/disaster relief mission. They only have 20 minutes to prep and load him—and his wife they know nothing about, who refuses to leave him—before their aircraft becomes fuel-critical. Although their treatment mission comes first, and their clientele’s status renders the civilian reintegration mission moot, the operational constraints—as opposed to capability—make matters more challenging.
As a final example, consider a surgeon working out of a tent, debriding a patient’s lower limbs following a mine incident. The surgery to save their life is technically somewhat different to the motor vehicle multi-traumas she usually deals with; these wounds are dirtier, the amount of viable tissue to work with is reduced, and she lacks comparable resources. Hence, the additional clinical training she received before deploying would prove exceedingly useful. Even so, operational pressures (e.g., holding policies and intensive care bed states) will likely influence the surgery she performs. Furthermore, she also needs to think ahead regarding her patient’s rehabilitation and probable civilian transition, not just regarding the surgery itself but also comprehensively documenting what it entails.
The fact that military health services have three separate but inextricably linked missions has three implications:
- The existence of the operational capability and civilian reintegration missions explains why military health services have to contend with rather more documentation than most civilian practices.
- Enabling operational capability—in particular (but not limited to) ensuring that a member’s job will not exacerbate their medical condition(s), and vice versa, that is, their medical condition(s) does not unduly impede job performance—explains why the ADF’s health services have three different coloured uniforms. Previous articles explain why health staff with the same environmental experiences as their clientele are more likely to successfully employ a risk management approach to uncertain cases—not only to prevent those from deploying who should not, but also to allow those to deploy who can—compared to those without such experience.15,16
- The issues of ‘work-relatedness’, per the operational capability and civilian reintegration missions, explain why military health services should be based on a systems-based occupational health strategic model.
Military health service functions and roles
Previous papers have described the following military health service functions and roles necessary to conduct these missions. These are summarised as follows, in ascending priority order, based on the level of military expertise they require:
- Treatment services.17 At the bottom of the list is treatment services: this acknowledges the extent to which the expertise acquired in civilian practice—however, distinguished—still only constitutes a baseline for undertaking this function in the military Furthermore, as in civilian settings, military treatment services should be based on the demographics of the target population: who they are, where they serve, what they do and why they do it. Pending better data, for now, the ensuing clinical presentations can most likely be characterised as musculoskeletal injuries split between workplace accidents and sports injuries, and mental health disorders split between people for whom joining the ADF has not been a wise career move, and people who heretofore have been fine working in Defence, but are struggling in their current job. This has two implications: first, the ADF should be considered a discretely different population compared to the general Australian civilian community, somewhat analogous to the indigenous and LGBTIQ+ populations. Second, although most service medicine lacks clinical interest, it is the context that makes it challenging, in particular, juggling patient needs against the other two missions in a way that—among others—is honest, ethical, transparent, empowers them as far as possible and complies with the Law of Armed Conflict (LOAC).
- Health promotion.18 The ADF needs to maximise its personnel’s general health and wellbeing: this reduces the number requiring treatment, enables operational capability and reduces the civilian transition workload. However, the scope of military health promotion is far broader than civilian practice: the RACGP ‘Red Book’ only provides a baseline for what ADF members need. Besides ensuring compliance with the Work Health and Safety Act, the ADF’s health services must also provide targeted military- and mission-specific vaccination programs, effective field and shipboard hygiene, and vector-borne infectious disease prevention. They should also provide military health education programs on first aid, personal hygiene and dental care, heat and cold stress management, sun exposure and insect bite prevention, alcohol and other drug awareness, and diet and weight control. There is also a need to provide military workplace mental health promotion programs that, besides enhancing mental resilience during deployments, enable mentally healthy, non-deployed workplace and personnel management practices. A pivotal consideration to all these interventions is that healthy lifestyle interventions—such as those in the ‘Red Book’—should not prevent personnel from deploying if they are elective and/or do not prevent them from performing their regular duties. Another consideration is that military workplace physical fitness programs should not create preventable new injuries or exacerbate old ones.
- Occupational and environmental health.19 The ADF population is medically selected, mostly young working age, geographically highly mobile, has high turnover rates, and—for now—is still predominantly male. That means, rather than reflecting a typical civilian dependency, the ADF is, first and foremost, a workforce Furthermore, ADF members are probably exposed to the broadest range of physical, biological, chemical, ergonomic and psychosocial workplace hazards of any Australian workforce, even before considering the operational hazards posed by weapons designed to cause harm, such as small arms, grenades, mortar and artillery rounds, sea-, land- and air-launched missiles, sea and land mines, and torpedoes, to which can be added chemical, biological, radiological and nuclear (CBRN) weapons. Although it also pertains to all the other functions and roles per this list, this bespoke occupational and environmental health component enables the operational capability mission by preventing people from getting injured in the first place; it also provides targeted workforce treatment services and actively facilitates the civilian transition mission.20,21
- Assessing medical suitability for military service.22 Ensuring that personnel managers, commanders and supervisors are aware of the health status of their personnel pertains to the operational capability and civilian reintegration missions. However, finding a clinically or operationally significant new medical condition at a routine medical usually implies a reasonably egregious failure regarding the patient’s primary health care. As previously described, medical suitability determinations are intrinsic to that care, from recommending light or excused duties to conducting Medical Employment Classification Reviews. Even so, this does not preclude bespoke periodic and targeted occupational health assessments, even if they only need to entail health record audits regarding vaccinations, cervical screening and the like.
- Military medicine capabilities.23 These capabilities include aviation, underwater and CBRN medicine. The need for these services not only pertains to preventing or treating casualties caused by the unique physiological hazards to which aircrew, divers and submariners are exposed, but also to giving them an operational capability edge vis-a-vis their opponents. Hence, the ADF health services provide these services in-house because they do not otherwise exist in forms that facilitate this mission. It also complicates the military health support function referred to below, noting that aircrew, divers and submariners each constitute subpopulations (totalling about 12.5%) that the ADF medical services must plan for. The same applies to ADF members who may have to perform their duties in CBRN environments.
- Humanitarian Aid/Disaster Relief (HA/DR).24 A previous paper explains why HA/DR should not be a primary role for the ADF’s health services: their focus should be on conducting its missions to support ADF members and other entitled personnel. That does not mean they have no HA/DR role; it is, however, a subset of military health support (see below). First, this is because, unlike other operations where they support other ADF agencies, the ADF health services may be the ADF agency being supported by these assets. Furthermore, HA/DR operations require different medical assets for vulnerable populations such as women, children, seniors and people with disabilities, who will most likely get better healthcare from Non-Government Organisations (NGOs) and other agencies. This means the ADF health services can be expected to liaise with such agencies far more during HA/DR operations.
- Medical evacuation.25 The fact that ADF personnel end up in odd places means that the ADF health services must be able to evacuate them from wherever they are ill or injured within a clinically and operationally suitable timeframe. While this has typically only been considered relevant for deployed personnel, the ADF’s need to insert its patients into the civilian health system necessitates appropriately holistic and targeted elective and emergency patient transport services. Examples include getting patients to and from specialist appointments; using civilian ambulance services in major population centres; or service vehicles, civilian aeromedical services or military aircraft for bases in remote locations; or civilian helicopter services for ejected aircrew or ships at sea; or civilian aircraft for interstate patient transfers; or military aircraft for mass casualty events within Australia.
- Military health support.26 As previously described, ADF members’ health support must reflect the population(s) being supported, their location and their activities. For example, the population at a particular base may include trainees, headquarters or support staff and/or members of one or more operational units. The latter might be working up to deploy, reconstituting after deploying or performing operational roles that do not entail deploying. Such bases may be overseas, at a remote location within Australia, where access to civilian health services may be problematic, or at a major urban centre where access is not an issue. The resources (i.e., FICs) that every ADF health element needs to conduct their missions depend on all of the above, which takes some planning and forethought. As examples, the health services for a remote operational base like Tindal will differ from those for a remote training base like Kapooka, or a support base for deployed units at a major urban centre like Stirling. Assessing, planning, implementing and monitoring these services against the FICs they require to conduct their missions is a health function for which military (including environmental) expertise becomes at least as important as clinical expertise.
Fundamental Inputs to (health) Capability
FICs refers to a standardised list used by the ADF to identify the resources required—except for the finances to pay for them—to undertake government-directed tasks.27 However, the ADF applies its FICs either as a whole or by elements within; at present, there is no publicly available evidence suggesting that its health services does so. While future papers will describe these in more detail, fulfilling the aforementioned functions and roles would arguably include the following considerations regarding each ADF health services FIC:
- This paper explains why military health services are far more complex than similarly-scaled civilian counterparts, whose only remit is to treat patients. Although having a relatively young and highly medically selected population helps, ADF members’ locations, what they do and why exacerbates this complexity, in the context whereby the ADF’s health services are part of a larger organisation for which health care is not the primary focus. Future papers will explain why this complexity is best managed—especially in a resource-constrained environment—by basing their organisational structure on an occupational health systems model.
- ADF health staff recruiting and entry training needs to reflect the functions and roles they are required to undertake, which begin with providing care within their scope of clinical practice in, at times, exceptionally remote and/or austere situations where casualty evacuation may be delayed. This refers to the skills, knowledge, expertise and currency to manage (not just treat) clinical conditions that are usually only encountered overseas, as well as being beset by mass battle casualties and/or disease and non-battle injuries. However, this paper also explains why these clinical skills only constitute a baseline: ADF health personnel need additional military skills as part of their career progression to conduct all the aforementioned functions and roles. These considerations also explain why the ADF’s health services must be based on its uniformed staff.
- Collective training. Like the rest of the ADF, its health personnel need their clinical and military skills to be shaped into teams for broader integration into the units (whether deployable or non-deployable) in which they serve. It should also be noted that they may have to train for a discrete health subunit or unit or a non-health unit for which they provide the health component.
- Civilian industry support. Notwithstanding the previous assertion that uniformed health personnel must be the bedrock of the ADF health services, the support they provide is complicated by the extent to which the technological health advances over recent decades have led to increasing levels of specialisation.28 As this precludes the ADF from organically providing the full range of health services, its services are utterly dependent on the clinical skills and expertise available only from the civilian health system. However, this does not mean the ADF can entrust the military aspects of managing its sick and injured members to these providers. Health reservists in particular, therefore, have an essential bridging role between the civilian and military health settings.29
- Other support. Besides the support provided by civilians, the ADF health services also require various forms of non-clinical health support that they cannot provide in-house. Examples include ships’ first aid parties, patient catering and laundry services for Navy, engineering support to provide electricity or piped water for Army, and providing aircraft for Air Force AME teams.
- Facilities. All ADF health services need facilities to work from, including fixed health centres in the base setting, deployable facilities in ships, on the ground or in the back of aircraft, down to the ship’s messdeck, half-demolished building or fighting pit, in which they can set up to treat patients with whatever they have available in a backpack or bumbag. Although the purposes they are needed for are broadly similar, these facilities need to reflect the supported clientele and the environments they work in; for example, divers and submariners, in particular, need their own additional deployable and non-deployable hyperbaric facilities.
- Supplies. The scope of this FIC extends beyond pharmaceuticals and other consumables to instruments and equipment. The complexities inherent in getting the right amounts of the correct items (and their spares) to the right place(s) at the right time(s) while ensuring they are properly serviced, maintained within the cold chain, remain sterile and/or in-date, indicate the need for a bespoke medical supply system. It also means personal equipment preferences are not likely to be met.
- Major systems. The ADF typically uses this term to refer to large and/or expensive items such as ships, planes and vehicles, which is less applicable regarding skill-based than equipment-based capabilities such as health services. However, this FIC in this setting arguably refers instead to health information technology systems for tasks such as patient records, telehealth, casualty regulation and medical store management. The biggest constraint in the operational setting is bandwidth; even without emission control limitations, it will never be sufficient, even without jamming or other forms of cyber warfare from opponents whose compliance with LOAC may be marginal or non-existent.
- Command and management. Finally, the ADF health services require structured health command and administrative processes that interact with each other and the relevant commanders consistent with their advisory roles. As previously described, this also explains why those in health leadership roles need escalating levels of military expertise as part of their career progression.
Finally, it is essential to note that, as all of these FICs are finite and limited, the ADF health services must employ a risk management approach to conduct their missions, to do the greatest good for the most significant number with the resources allocated, as part of an organisation for which healthcare is not its primary purpose. The need for a risk management approach in this setting is entirely consistent with a systems-based occupational health strategic model.
Conclusion
There has been a longstanding misperception within Defence (including elements within its health services) that, as they only exist to provide treatment services, its health services are an obvious exemplar of something that can be easily unified or contracted out. This fails to recognise the other two missions of health services that support military workforces rather than civilian populations, enabling operational capability and facilitating their eventual transition to the civilian community.
The previous series of papers explained why excessive workplace illness and injury rates confirm the need to improve the management of hazards associated with ADF workplaces, with better emphasis on prevention. This is summarised in Figure 1, which shows the relationships between ADF operational capability, the three health service missions necessary to enable that capability, the eight health service functions and roles to enable those missions, and the nine FICs needed to conduct them. It also demonstrates how occupational health is intrinsic to all the holistic military healthcare system components.
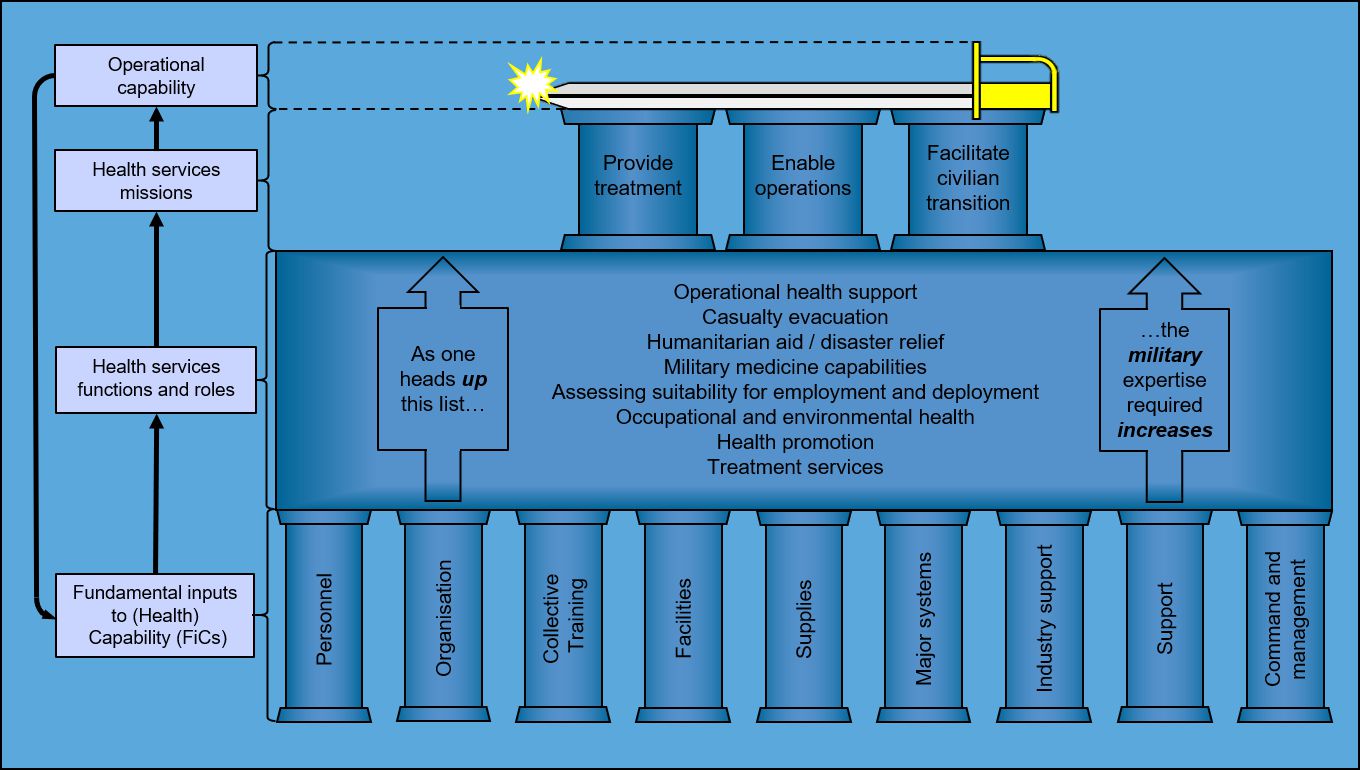
Figure 1: Operational capability and its relationship to military health services missions, functions and roles, and FICs
It is also suggested that, as applied to the ADF health setting, Figure 1 is consistent with the meaning of the word ‘joint’ as defined by the then CDF in 2017:
‘I look at where we’ve come to now from back then [1999] and we are well ahead, with a far better understanding that joint isn’t doing everything the same. Joint is about bringing the best of the three services and the public service together to get the best combination you can for that particular operation.’ [underlining added].30
Disclaimer
The views expressed in this article are the author’s and do not necessarily reflect those of the RAN or any other organisations mentioned.
Corresponding Author: Neil Westphalen, neil.westphalen@bigpond.com
Authors: N Westphalen1,2
Author Affiliations:
1 Royal Australian Navy – Directorate of Navy Health
2 University of New South Wales Canberra at ADFA






