D Randell, M Fett, H Jenner, S Frances, D Shanks
Abstract:
Not all epidemics are due to infectious diseases. We report an epidemic of processionary caterpillar dermatitis occurring in military officer cadets participating in a field exercise. The risk of caterpillar dermatitis was unappreciated by those on a map exercise near Majura, despite seeing such insects in the field. At least 103 ADFA and RMC cadets were affected with large areas of dermatitis with an urticarial rash, about 30 seriously enough to require topical steroids. Caterpillar dermatitis occurs commonly but only rarely does it present as a unit incapacitating epidemic of severe dermatitis with urticaria.
Key words: dermatitis, epidemic, processionary caterpillars
Introduction:
Many illnesses can rapidly incapacitate a military unit but it is particularly disturbing when the agent is unknown or unsuspected. Outbreaks of gastroenteritis trigger a search for enteric infections; as outbreaks of respiratory symptoms trigger screening for infections such as influenza. In a similar way, an outbreak of dermatitis triggers a search for some contact exposure and is usually limited to one or only a few persons with a fairly obvious source to incriminate. Causes of epidemic dermatitis with urticaria and pruritus are few and can usually be traced to some natural source. Psychological problems may arise during war time if such outbreaks are imagined to be due to blister
agents such as mustard gas or other toxic exposures. Accurate diagnosis coupled with symptomatic treatment is usually sufficient to calm an affected unit and get them back to duty.
Epidemic:
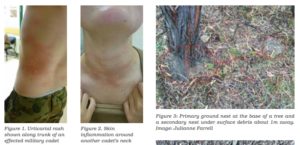
We report an epidemic of processionary caterpillar dermatitis with urticaria which occurred in officer cadets at the Australian Defence Force Academy (ADFA) and the Royal Military College (RMC), Duntroon ACT in February 2016. A company of officer cadets were participating in a field training exercise without troops. They were occupied with maps while in the open air under trees at the Majura Training Area. Suddenly several of the cadets began to develop severe itching and skin irritation. Figures 1 and 2. This rapidly spread to involve 54 ADFA and 49 RMC cadets (a majority of those present) and some of the directing staff. At least 21 of these cadets required an after-hours clinic visit at the Duntroon Health Centre due to intractable pruritus and insomnia, excoriation and pain. None of the cadets claimed direct contact with any insects or disturbed any possible nesting sites. On examination, large areas of urticaria and inflammation were seen as shown in the first two figures. Caterpillar dermatitis with urticaria was assigned as the likely diagnosis and the cadets were given symptomatic treatment with oral antihistamines and topical steroids. Pruritus severe enough to disturb sleep gradually resolved over a few days.
Dermatitis:
Caterpillar dermatitis was formerly called “erucism” deriving from the Latin eruca (caterpillar). It is caused by brittle hairs (setae) on the caterpillar which may readily break off and embed in skin on contact1. Each caterpillar may produce greater than a million setae2. The hairs can be direct mechanical irritants and can be broken, releasing
a wide variety of chemical irritants containing enzymatic compounds and protein toxins 2,3 These proteins can cause both immediate and delayed type hypersensitivity reactions. Direct contact with caterpillars is not required and aerosolised spines in heavily contaminated areas near bag-nests do, if rarely, cause epidemic urticaria. Indeed, a massive outbreak occurred in Shanghai, China in which 500,000 cases of dermatitis were attributed to airborne hairs of the Asian mulberry moth
caterpillar settling on garments hanging on clothes lines4. Forty-two of ninety persons became ill by such indirect contact with the oak processionary caterpillar in Germany5.
The most common moths implicated in caterpillar dermatitis seen in Australia are Ochrogaster lunifer – the bag moth, Euproctis edwardsii – the mistletoe browntail moth, and euprotis lutea – the freshwater mangrove moth6. A four-month outbreak of dermatitis in 2001 was eventually traced to mistletoe browntail moth caterpillars in a tree within three meters of a community centre in New South Wales7. A wide range of moths can cause such outbreaks globally with symptoms usually ranging from mild pruritus to dermatitis with urticaria8. Rarely severe events are noted such as osteomyelitis or corneal injury9. In Australia, Bishop and Morton (1968), reported 86 cases of eye injury due to setae of Anthela nicothoe, the hairymary caterpillar10. In Brazil, Lonomia caterpillars can rarely cause hemolysis and internal bleeding which can lead to death11.
Previous outbreaks:
The only previously described outbreak in the Australian army we were able to locate occurred in 1944 when ten soldiers became ill from contact with Ochrogaster lunifer caterpillars in a north Queensland bivouac area12. The Israeli army reported the largest outbreak of military caterpillar dermatitis in 1959 when 600 of 3000 soldiers camped in a pine grove were affected by contact with Thaumetopoea wilkinsoni, a relatively recent importation from Europe13. An outbreak of caterpillar dermatitis in a US military community in Germany in 1995 affected 144 soldiers and civilians2. The US military in Lavorno, Italy regularly monitors and controls for processionary caterpillars.
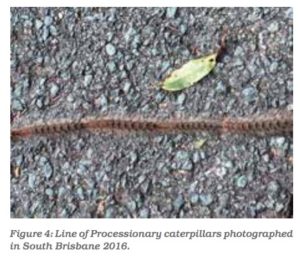
Processionary caterpillars are those that move in files of up to six metres in length, each caterpillar head to tail from their nests – found at the base of a tree, on the trunk, or in the canopy – to feed on forage before returning to their nests. Figure 3. They generally feed at night, leaving the nest in late afternoon or early evening and returning to the
nest around dawn. Figure 4. Although specimens were not available to make a positive identification, the most likely insect involved is the coastal bagshelter moth or inland bagmoth (Ochrogaster lunifer) based on insects known to produce such epidemic urticaria historically1,3. A single contact is enough to discourage any future contact with such larval insects but unapparent contamination around their bag-shelters does occur14.
Differential Diagnosis:
While most cadets presented with a papular urticarial wheals, a few presented with a more petechial rash and pin-size papules. Scrub-itch mite (‘kangaroo mite’) was considered a possible causal agent and some directing staff sought topical insecticides to ensure that they were ‘mite-free’ after return to barracks. The distribution of these rashes tended to be on the chest and abdomen, unusual for mite bites that usually occur predominantly in the lower half of the body and particularly ankles. Close inspection failed to reveal any sign of mite activity and this was
thought an unlikely cause. The Majura Training Range is mostly grassland and lightly wooded eucalypt and there are few reports of biting midges or fleas. The urticarial lesions were flat-topped and not typical of mosquito bites.
There are relatively few epidemic agents capable of incapacitating a military unit. Other non-infectious natural exposures besides caterpillars include a variety of trees and plants such as “poison wood” (Metopium brownei) and “blinding tree” (Excoecaria agallocha) in Central America with toxic excretions (e.g. sap) that contaminate soldiers resting under such vegetation. Noxious substances or toxins (e.g. jellyfish) to protect the organism are common
in nature but most require direct contact and are obvious to the observer. Prevention of future caterpillar-caused epidemics depends on identifying the threat from the presence of bag-shelters in canopies, on tree trunks, or at the base of trunks or lines of caterpillars and carefully avoiding such areas likely to be contaminated.
Key Points:
• The military medical importance of caterpillar
dermatitis is poorly appreciated
• Urticarial wheals are commonly reported from
exposure to processionary caterpillars
• History of exposure can be vague
• Treatments are largely based on symptoms
• Topical steroids and oral antihistamines have
good success
Those exposed to caterpillars, or their nest material should not scratch their face because they risk rubbing the setae (spines) into their eyes, which may cause severe pain.
First aid consists of using sticky tape over the skin to remove the setae
Contributors:
DCR, MJF and HRJ were the treating physicians, SPF was the consultant entomologist and GDS was responsible for initiating the report as well as the writing of the first draft of the manuscript. All authors participated in writing the final manuscript.
Conflicts of interest statement: The authors do not claim any conflict of interest.
Funding: Some of the authors are employees or contractors of the Australian Defence Organization or members of the Australian Defence Force but none received any specific funding for this report.
Acknowledgements: The authors thank the affected officer cadets at the Australian Defence Force Academy and the Royal Military College, Duntroon as well as the staff of the Duntroon Health Centreparticularly Dr Geoffrey Lucas for their cooperation. Julianne Farrell of the University of Queensland is thanked for providing photos and commenting on the draft manuscript.
Disclaimer: The opinions expressed are those of the authors and do not necessarily reflect those of the Australian Defence Force.
Corresponding author: G. Dennis Shanks
Dennis.Shanks@defence.gov.au
Authors: D Randell1, M Fett1, H Jenner2, S Frances2,3,
D Shanks2,3,
Author Affiliations:
1 Royal Military College of Australia – Medical Centre,
Duntroon, Australian Capital Territory, Australia
2 Army Malaria Institute – Vector Surveillance and
Control, Gallipoli Barracks Enoggera
3 University of Queensland – School of Public Health,
Herston Queensland






