D Shanks, M Waller
Abstract
The 1918–1919 influenza pandemic was the greatest mortality event in recent history whose specific origins and mechanism remain largely unexplained. Wide ranges of mortality were observed in otherwise identical groups for unclear reasons. The 49th (n=1363) and 50th (n=1243) Battalions (BN) of the Australian Imperial Force (AIF) respectively had one of the highest and lowest influenza mortality rates of any Australian infantry unit. All non-combat mortality, specific pneumonia/influenza mortality and morbidity due to influenza-like illness were collected from both battalions 1916-1919.Mortality during the 1916-1917 epidemic of ‘purulent bronchitis’ was similar (8 deaths in both) whereas the 49th BN had 18 and the 50th BN had one pneumonia deaths during the influenza pandemic of late 1918-early 1919.Influenza morbidity was similar in both units except during mid-1918 when the 50th BN experienced more cases of a mild influenza-like illness (69 vs 103 cases in June).The 49th BN had more recorded cases of influenza than the 50th BN during the late 1918 pandemic (116 vs 62 cases in October).Recent influenza-like illness appeared to markedly decrease influenza mortality without greatly changing influenza morbidity in 1918.
Key words: influenza, pandemic, mortality, World War I
Introduction
Pandemic influenza can stop military operations when a large number of soldiers suddenly become ill. High mortality due to influenza in otherwise healthy adult males has only been observed during the 1918–1919 pandemic for uncertain reasons.1 More people died during the influenza pandemic than during World War I, including greater than 1 200 Australian soldiers in the Australia Imperial Force (AIF) deployed to Europe and the Middle East.2 The unexpected and still unexplained propensity of the 1918 influenza virus to kill young adult men remains a unique observation thought to be linked to the massive population disruptions associated with World War I.
In the absence of effective influenza vaccines, one’s immunity depends on previous influenza infections producing immunological memory in the form of either specific antibody or lymphocytes capable of killing infected respiratory cells. Influenza has certainly existed for centuries, but it did not cause annual epidemics until after 1918, likely due to limited population movements.3 Influenza rapidly changes its surface proteins (hemagglutinin H; neuraminidase N) requiring adaption of the host and/ or annual revisions of influenza vaccine to respond to viral evolution. An individual’s particular lifetime experience with influenza virus largely determines how well the host is able to resist infection.
Although reliable mortality data have been collected for over a century, it is extremely difficult to link historical mortality with previous morbidity records due to influenza. Military medical systems are one of the few circumstances where one can confidently measure influenza morbidity and subsequent mortality in individuals using prospectively collected data over more than a single season. Only with this level of detail is it possible to suggest why the 1918 pandemic’s lethality was so different from all other known pandemics. We have examined the Australian National Archives online collection of AIF soldier records linked to both the AIF Database Project of the University of New South Wales and the Honour Roll of the Australian War Memorial in order to determine if previous influenza illness changed a soldier’s mortality risk during the 1918–1919 influenza pandemic.2 The specific question asks how might co-located infantry units, appearing otherwise identical, have such different influenza mortality rates?
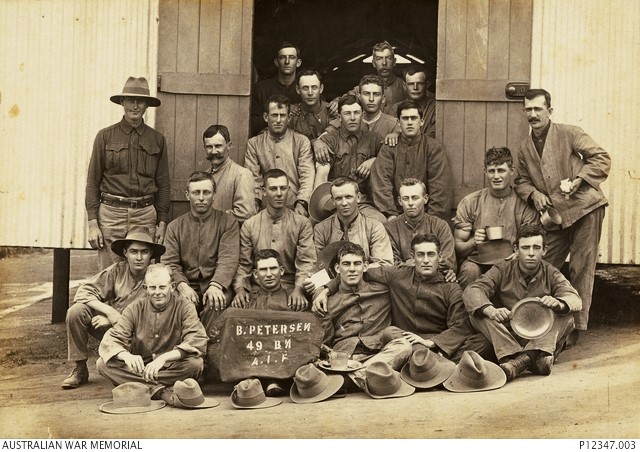
Figure 1: Group of Australian soldiers from the 49th Battalion Australian Imperial Force in Brisbane circa 1916 prior to deploying to France. (Source: Australian War Memorial, photo P12347.003)

Figure 2: Group of Australian soldiers from the 50th Battalion Australian Imperial Force in a trench near Ypres, Belgium in 1917. (Source: Australian War Memorial, photo E00761)
Methods
This study is a part of a much larger effort originally reported in 2010 which the reader is referred to for details of the data collection methods and analytic approach used.2 During this previous work it was noted that 1 363 men of the 49th Battalion (BN) and 1 243 men of the 50th BN, despite being located in the same 13th Infantry Brigade in France in 1918, had very different influenza mortality rates (See Figures 1 and 2).Given the uniformity of infantry units, especially when co-located in the same brigade, detailed study of these two battalions was conducted to determine if previous influenza experience was a key determinant of subsequent mortality risk. The National Archives online (www.naa.gov.au) medical and administrative records of the men in these two infantry units were examined in detail collecting all recorded instances of influenza-like illness to which the reader is referred. Very accurate mortality information was available from the Roll of Honour from the Australian War Memorial (www.awm.gov.au) as well as detailed demographic information from the AIF Database Project of the University of New South Wales to which we were graciously given access by Prof Peter Dennis.2 Epidemic curves were constructed from these named individual soldier records measuring non-combat mortality, pneumonia/influenza specific mortality, and influenza-like illness morbidity 1916–1919. Denominator data required considerable estimation due to the near constant movement of soldiers within the AIF.
Results
Figure 3 displays the resulting information gathered from both AIF infantry battalions. Influenza mortality was primarily seen during two periods of World War I in late 1916, early 1917, when it was labelled as ‘purulent bronchitis’ and in late 1918, early 1919, during the influenza pandemic.4 Most modern observers consider both episodes likely to have been caused by the same influenza virus that did not manage to spread globally until 1918.Pneumonia/ influenza mortality in late 1916, early 1917, was identical (8 deaths) in both battalions (See Figure 3A).However, in late 1918, early 1919, there were 18 influenza deaths in the 49th BN and one death in the 50 BN, giving a calculated mortality rate of 7 out of 1000 men vs 0.8 of 1000 men. Figure 3B shows that half of all non-combat (mostly due to other infectious diseases but including accidents) mortality was due to pneumonia/influenza in 1916–1919.Non-combat deaths that were not caused by pneumonia/influenza were similar (23 vs 25) between the two units. Influenza morbidity was similar in both units except during mid-1918 when the 50th BN experienced more cases of a mild influenza-like illness (69 vs 103 cases in June) (See Figure 3C). The 49th BN had more recorded cases of influenza than the 50th BN during the late 1918 pandemic (116 vs 62 cases in October).
Discussion
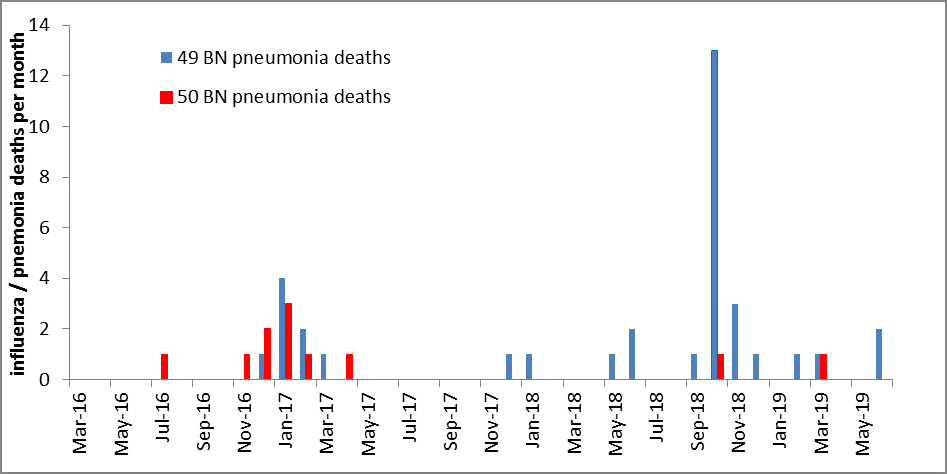
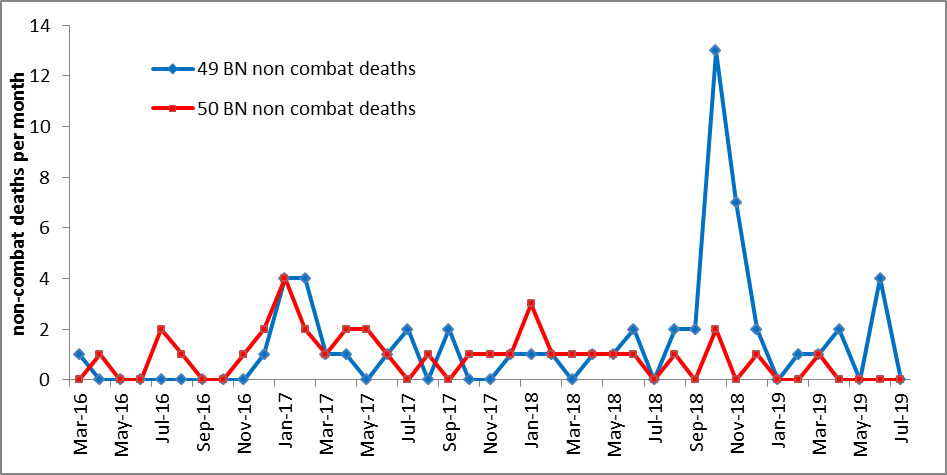
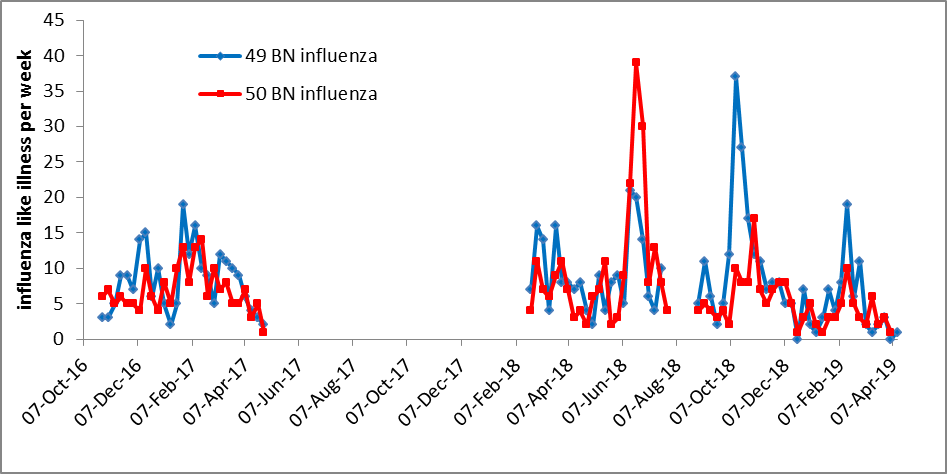
Figure 3A–C: Epidemic curves in two co-located infantry battalions showing A. pneumonia/influenza deaths by month; during pandemic period this was a total of 18 deaths in 49th BN vs 1 in 50th BN B. all non-combat deaths by month; 23 deaths in 49th BN vs 25 in 50th BN and C. influenza-like illness by week during 1916–1919 in France/Belgium during World War I.
Comparison of two co-located AIF infantry battalions showed that although influenza mortality was identical in the first epidemic in late 1916, early 1917, during the main wave of the influenza pandemic occurring in late 1918, early 1919, a ninefold difference in mortality was observed. There were no differences in non-combat deaths that were not attributable to pneumonia/influenza. Influenza morbidity differed during mid-1918 when the 50th BN had more cases of non-lethal illness. The situation was reversed in late-1918 when the 49th BN experience more influenza cases.
Could mild influenza infections occurring during mid-1918 have protected soldiers against death later in the same year? This was true when a larger dataset (n = 8840), which included both the 49th and 50th BN as well as medical officers, military nurses, engineers and flying corps, were studied using a Cox proportional hazards model.2 When a further case-control analysis was done with all known influenza deaths (n=1238) during the 1918–1919 pandemic matched to an equivalent number of surviving controls who joined the military at the same time, earlier influenza-like illness was protective against mortality (odds ratio, 0.37, 95% CI, 0.25 to 0.53).2
These data have been previously reported. The remaining question was whether the same conclusion could be sustained when looking only at two co-located infantry battalions over time. The epidemic curves presented in this sub-study show that the only difference that can be discerned between the two units was due to increased influenza morbidity in the 50th BN around mid-1918.This fits multiple descriptions made during the war of the widespread nature of non-lethal influenza in mid-1918 serious enough to cause such concern that sufficient well soldiers would not be available to stop the final German offensives on the Western Front.5 The French Army (approximately 4 million men) estimated their mortality during the two waves at less than 100 in mid-1918 and 28 000 deaths during late 1918, early 1919.6
However, infection with mild influenza in mid-1918 did not protect against influenza morbidity in late 1918, a finding which has since been confirmed in two US military academies.7 The most parsimonious explanation requires the existence of at least two influenza viruses causing different pandemic events in 1918; one mild, the other lethal.8 Cross-protection occurred for mortality but not morbidity indicating the viral surface proteins were likely different. This interpretation is supported by mortality data from the different Australian states in 1919.Victoria and New South Wales had much greater mortality (two to threefold) in 1919 compared to the previous 1891 pandemic. In Tasmania, however, where the lethal pandemic arrived after nearly a year of mild influenza circulation through the island, influenza related mortality in 1919 was not greatly different from the previous 1860 and 1891 pandemics; particularly muted was the unique young adult mortality signature of 1919.9 Across the world, highly variable influenza mortality at the country and city level suggests that these otherwise similar social units had recent exposure to an influenza virus different than the lethal H1N1 virus of late 1918, early 1919.10
The utility of military records to address historical epidemiological questions is obvious. What might these findings mean for the next influenza pandemic? Taken together, the severe mortality seen in 1918– 1919 appears to have been driven by distinct epidemiological events which are very unlikely to reoccur. The global spread of influenza through the modern transportation network insures that many different viruses are simultaneously circulating; all humans, other than infants, likely have some immunity from a previous infection. The same globalisation that brings seasonal influenza is also what may be protecting us against severe mortality during the next pandemic.
Contributors
GDS was responsible for designing the epidemiological project, initiating this particular report as well as the writing of the first draft of the manuscript.MW was in charge of data collection and analysis. Both authors participated in writing the final manuscript.
Conflicts of interest statement: The authors do not claim any conflict of interest.
Funding: The lead author is a member of the Australian Defence Organisation but did not receive any specific funding for this report.
Corresponding Author: Dennis Shanks, dennis.shanks@defence.gov.au Authors: D Shanks 1,2, M Waller 2 Author Affiliations:
1 Australian Defence Force Malaria and Infectious Disease Institute, Enoggera, Australia
2 University of Queensland, School of Public Health, Brisbane, Australia






