G. D Shanks, N Marsh
Abstract
Acute respiratory infections due to a variety of viral pathogens can incapacitate entire military units. During World War II, recruit camp epidemics of respiratory infections at Woodside Camp South Australia and Puckapunyal Victoria caused considerable morbidity with up to 44% attack rates but little if any mortality. Camp hospitals were filled with hundreds of recruits in 1940. An infantry battalion (2/9 BN AIF) experienced an epidemic of respiratory disease during its transit from the UK to Suez, Egypt, on a troopship. Although there were no deaths, 30% of the battalion became suddenly ill, and 17% were hospitalised over a single week in December 1940. COVID-19 has drawn modern attention to the casualty-producing potential of epidemic respiratory infections in military units, especially those crowded together for training or during transit to operational areas.
‘Hospital facilities broke down and sleeping huts within the unit were turned into temporary wards with Australian Imperial Force nurses and members of voluntary Aid Detachments in charge.’
CAPT S L Seymour 19411
Acute respiratory diseases are one of the few infectious diseases that can rapidly incapacitate an entire military unit. Although influenza is typically most associated with military operations following the lethal 1918–20 pandemic, other respiratory viruses, such as adenovirus, rhinovirus and coronavirus, are also of great military interest.2,3 The advent of COVID-19 has particularly focused the minds of military planners on military unit’s vulnerability, especially those deployed globally, to respiratory viruses other than influenza.4 We review the Australian Imperial Force (AIF) experience with acute respiratory infections (ARI) during 1940 as a historical example of what is possible when a new respiratory virus moves into a non- immune population of otherwise healthy soldiers. Although 80 years in the past, the basic biology of exposure and infection has not changed and today’s Australian Defence Force (ADF) remains vulnerable to disruptions from new respiratory viruses.
Typically ARIs have been the greatest problem of military recruit camps during mobilisations when large groups of civilians from diverse backgrounds and locations gather together for initial military training.5 Such was the case at the beginning of World War II when in 1940, a series of ARI epidemics were described in the AIF. These were variably named ‘Woodside throat’ in South Australia, ‘Ingleburn cough’ in New South Wales or ‘dog’s disease’ (presumably due to a barking cough).1 In May 1940, Seymour reported that 400 (44%) of 900 men in a training battalion in Victoria became ill in a single month. Up to 200 were in the hospital or incapacitated in barracks at one time (see the introductory quote to this article).1 The epidemic was over within another month but not before massive disruptions of training schedules. Illnesses during the epidemic were characterised as pharyngitis, ‘burning fire in the throat’ and ‘as if the head was going to be lifted off’ from coughing. Many soldiers were acutely ill, but there were few if any secondary pneumonia cases, as is common with influenza. The illness was rapid with elevated fever for 2–3 days before passing suddenly. There was little nasal discharge at first but became more profuse with nasal obstruction over time.1 This epidemic occurred at the dawn of virology, and Burnett was eventually able to isolate influenza in eggs during subsequent epidemics in 1941–42.6,7 The consequences were serious enough for the war effort to initiate a major medical research program at the University of Melbourne, eventually leading to an attenuated, live influenza vaccine. Although one cannot know the viral pathogen involved in 1940, it was unlikely to have been influenza. A possible cause was adenovirus, notable for causing large outbreaks of influenza-like illnesses in military recruit camps.2
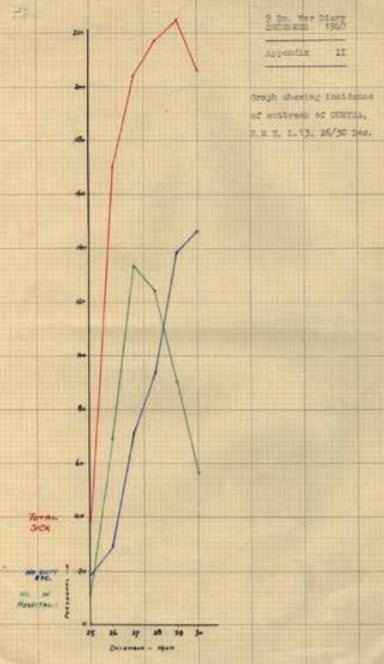
Late in 1940, a troopship epidemic occurred within the 2/9 Infantry Battalion AIF while en route between the UK and the Middle East. The troopship HMT L13 (SS Dunera) was forced to travel via South Africa because of war in the Mediterranean. After a 14-week voyage between Durban, South Africa (16 Dec) and Suez, Egypt (28 Dec), 224 of the 738 (30%) soldiers developed ARI over a single week8 (see Figures 1 and 2). No cases of pneumonia were reported from illnesses that were generally characterised as ‘coryza’. Officers and enlisted ranks were equally affected, and most were in the ship’s hospital for only 2–3 days. By the time the ship arrived in Alexandria, Egypt (31 Dec), there were still 28 men who had to be transferred to 8th Australian General Hospital. After 10 days, eight of these men re-joined the unit in the desert, indicating that in some cases, the illness continued over more than a week.8 Nonetheless, the unit had continued to function as the enforced convalescence largely occurred on the ship prior to deployment in Egypt.
Figure 1: Acute respiratory infection epidemic in the 2/9 BN AIF in December 1940 while onboard the troopship HMT L13 (SS Dunera) while transiting from Durban, South Africa to Suez, Egypt.8

Figure 2: Original data from the same epidemic as it appeared in the Unit War Diary of the 2/9 BN AIF for October-December 1940 from the Australian War Memorial Collection https://s3-ap-southeast-2.amazonaws.com/awm-media/collection/RCDIG1023070/bundled/RCDIG1023070.pdf 8
Troopships are inherently risky environments for ARI due to the high concentration of soldiers/sailors within limited ventilation areas. The 2/9 BN AIF escaped relatively lightly and continued its deployment to Egypt in January 1941. Classic examples of ‘death ships’ occurred as recently as World War I when troopships were infected during the 1918 influenza pandemic. HMNZT Tahiti was transporting the 40th Infantry Battalion of the New Zealand Expeditionary Force in August 1918 and experienced 7% overall mortality and 67% morbidity after influenza came aboard in Freetown, Sierra Leone.9 The 40th BN was immediately placed in quarantine on arrival in the UK and was never able to reconstitute itself into a fighting force before the armistice three months later. Lest one thinks these events are only of historical interest, the US Navy aircraft carrier USS Roosevelt was incapacitated in 2020 by a ship-board epidemic of SARS-CoV2 (COVID-19). The vessel became immobilised in Guam for two months, and a series of crew diagnostic screens eventually found more than 1000 sailors (20% of crew) infected.10 One death resulted from COVID-19, but the important military outcome was no active US Navy carrier battle group in the Western Pacific for a time. This was due to the incapacitation of the USS Roosevelt and to the quarantine of potential replacement units. Despite strenuous efforts using non-pharmacological public health interventions, military deployments involve large numbers of personnel where social distancing is impossible and irreducible risks of ARI epidemics remain.
80 years after the 1940 epidemics, recruit camp and troopship epidemics are no longer common occurrences. This is largely because of the ADF size and because its overseas deployment are usually carried out by aircraft.9 However, influenza outbreaks often isolate entire training companies at Puckapunyal for weeks, and ARI infections following international flights are common. ARI are ubiquitous infections caused by a wide variety of viral pathogens against which we have both imperfect public health procedures and few vaccines. In our globalised world, newly evolved viruses can disseminate rapidly and, as COVID-19 has rudely reminded us, cause severe human and economic damage. Today, ADF soldiers are much more likely to see mass mortality in aged care facilities in Victoria, Australia, from COVID-19 than on the battlefield from artillery fire. Part of the ADF’s adaptation to an uncertain future needs to come from learning from its rich history.5
ARI is part of the ADF’s military experience that previous generations have learnt to manage with practical public health measures aided by new vaccines, which have been the product of targeted medical research. We must aspire to do the same in our current situation.
Contributors:
GDS and NM are jointly responsible for the entire manuscript.
Conflicts of interest statement:
The authors do not claim any conflict of interest.
Funding:
The first author is an employee of the Australian Defence Organisation and a retired US Army medical officer but did not receive any specific funding for this study.
Disclaimer:
The opinions expressed are those of the authors and do not necessarily reflect those of the Australian Defence Force or the US Department of Defense.
Corresponding author: G. Dennis Shanks Dennis. Shanks@defence.gov.au
Authors: G. D Shanks1,2, N Marsh3
Author Affiliations:
- Australian Defence Force Malaria and Infectious Disease Institute
- Univeristy of Queensland, School of Public Health
- The University of Adelaide, Faculty of Health and Medical Sciences




