S Harvey, D Bimler, D Dickson, J Pack, O Sievwright, D Baken, A Henricksen
Abstract
Acceptance and commitment therapy (ACT) is rapidly gaining recognition in numerous therapy settings as a treatment of choice. To date, however, research has neglected to investigate the suitability of ACT in military settings. The current investigation is an exploratory repeated-measures design evaluating an ACT wellbeing course with military personnel from the New Zealand Defence Force (NZDF). The sample consisted of soldiers (n=292), primarily referred by their units and medical personnel for anger, alcohol use and stress-related issues. At one- and three-month post-treatment, participants showed significant reductions in their levels of alcohol consumption, anger and aggression, perceived stress, anxiety and perceptions of others being responsible for their circumstances. Furthermore, the findings suggest that participants developed enhanced awareness and management of their emotions as a result of this intervention. While preliminary, these findings support the efficacy of ACT with military personnel in addressing issues they encounter.
Key words: Acceptance and Commitment Therapy, ACT, Group therapy, Anger and Aggression, Alcohol
Acceptance and Commitment Therapy Group Treatment with the Military: A Preliminary Study
Introduction
In recent times, major concerns have been identified regarding problematic alcohol use in military service personnel (MSP)(1). A corresponding awareness is emerging of the linkages between experiences of MSP and the development of mental health issues (e.g. combat deployments, conflicting family and work responsibilities, station changes) and alcohol use difficulties(2). Development of prevention and intervention initiatives must be, therefore, sensitive to the experiences of MSP(3). Unfortunately, there is little research investigating psychological and alcohol use treatment interventions or their suitability to this population(4, 5).
Military populations have a relatively high risk of developing alcohol-related difficulties compared with civilian populations(6). Work- and family-related stress, frequency and number of active service deployment (both during and after), and combat-related stress due to exposure to traumatic events are known contributors to alcohol abuse issues(2, 7, 8, 9). Additionally, the belief that alcohol enables coping by lifting morale, increasing unit cohesion and protecting soldiers from adjustment problems to civilian life is a widespread belief within the military(10). While sanctioned as a way to deal with the stressful demands of military life, when alcohol-fuelled behaviours become excessive (e.g. violence, binge drinking or alcohol dependency) and impinge on soldiers’ general functioning, it can result in major disciplinary actions. The current trajectory of alcohol abuse in the military services is argued to be unacceptably high and constitutes a public health crisis(1).
Empirical evidence is increasing for the treatment efficacy of workplace interventions in significantly reducing problematic outcomes of substance use disorders (SUDs) (e.g. SUD-related injuries and violations), and in simultaneously promoting healthful behaviours and stress-management(11, 12). Such interventions are aimed at changing individual behaviour and reducing environmental risk factors(6). Particularly promising are brief intervention wellbeing programs with an educative emphasis on the promotion of stress reduction and healthy lifestyle habits, as well as the reduction of risky behaviours, particularly problematic SUD consumption(6). Findings have indicated that SUD-focused interventions offering educative health-risk appraisal and brief counselling can reduce alcohol consumption and that such treatment approaches are practically and cost-effectively delivered by way of brief intervention format(11, 12).
Group therapy workshops are widely used with MSP for a variety of mental health and SUD concerns and have produced equivalent efficacy to individualised treatment(13, 14). Two marked advantages of group therapy interventions are their cost-efficiency and capacity to address greater numbers of MSP simultaneously. This has led to their increasing use by military psychologists and an increased research focus on this modality(13, 14).
A treatment approach that shows promise and is being applied in military settings is Acceptance and Commitment Therapy (ACT)(15). ACT is a ‘third-wave’ contextualistic behavioural therapy characterised by the adoption of mindfulness and acceptance processes(16). ACT is conceptualised as a transdiagnostic approach in the sense that it aims to weaken avoidance processes, which link various comorbid conditions at either the clinical or subclinical level(17). ACT does not explicitly attempt to reduce the presence of ‘symptoms’, but instead encourages the acceptance of psychological experience (e.g. unwanted cognitions and emotions whose presence or absence cannot be controlled) and commitment to personally meaningful value-driven behaviour(16).
Outcome research has accumulated for ACT’s effectiveness when targeting clinical problems such as depression, social phobia, generalised anxiety disorder, trichotillomania, borderline personality disorder, psychotic symptoms and chronic pain (for a review, see Ruiz, 2010)(18). ACT has also shown promise in treating individuals suffering from SUDs(18, 19), and comorbid psychological disorders, such as depression(17) and post-traumatic stress disorder (PTSD)(20).
ACT has the versatility to be used both as a brief therapy and as a long-term treatment(16) and is gaining recognition in military settings. ACT is endorsed by the US Department of Veteran Affairs as an evidence-based treatment for use with mood disorders(21). However, with the exception of Blevins et al.’s (2011) brief (2 hour) ACT-based intervention, research into the efficacy of ACT with MSP in addressing SUDs is largely lacking. As such, further work is needed to determine the effectiveness of ACT-based programs with MSP. The present study sought to address this with an investigation of the efficacy of an ACT-based intervention trialled with MSP at two army bases. We employed a brief one-week group course format/intervention, in line with established support for the impact and cost-effectiveness of brief interventions and delivery via group therapy(12, 18). We hypothesised pre- to post-intervention decreases in alcohol consumption, drug use and desire to use, anger, perceived stress, anxiety, and chance and powerful others as loci of control. Conversely, we hypothesised pre- to post-intervention increases in internal locus of control and emotion management.
Method
Participants
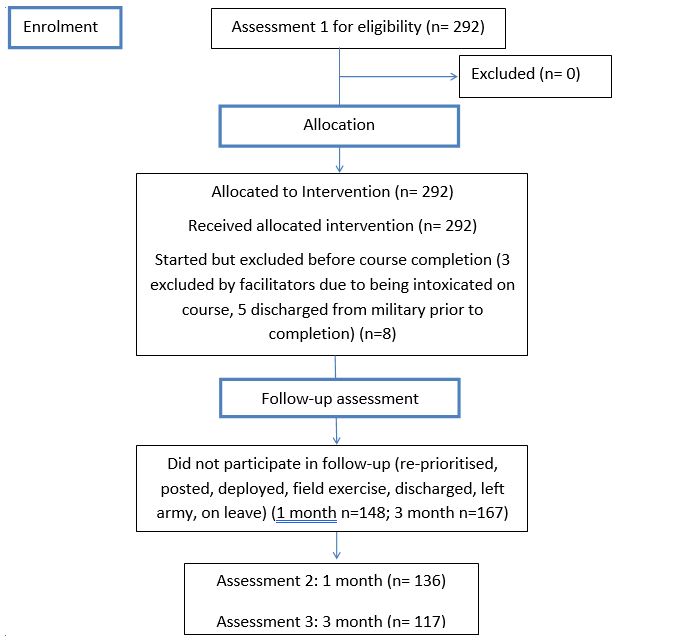
Assessment measures were administered to participants who enrolled in the course between April 2011 and November 2017 (N= 292; See Figure 1). The sample consists of 24 groups with approximately 5-15 participants in each group. Sample selection occurred by referral from the participants’ unit commanders, military health professionals, direct court orders or the participants themselves. Referrals were largely based on alcohol- and other drug-related difficulties (AOD) (e.g. dysfunctional use or alcohol-related behaviour involving psychological, social, occupational or legal difficulties). With other considerations deemed by unit commanders to be causing social or occupational impairment (e.g. stress, anger and aggression, or other-emotional issues such as depression and reintegration difficulties, or communication and relationship problems) also prompting referral to the course. Participants ranged in age from 18 to 46 years (M=23.86, SD=5.19), although the majority (57.2%) of participants were aged 20 to 29. Refer to Table 3 for a summary of the participants’ sociodemographic characteristics.
Two exclusion criteria were used regarding suitability for course admission: (1) likelihood of disruptive behaviour and (2) the presence of suicidal ideation. These were assessed during a brief interview around the time of each potential participant’s referral by one of the two clinicians who ran the course. In regards to informed consent, participants were selected and referred according to military protocol. The Massey University Human Ethics Committee judged the current study to be of low-risk status, as the investigation was a secondary analysis of existing, non-identifiable archival data resulting from the new NZDF AOD treatment protocol. Although workshop attendance was required for all those referred to the course, the evaluation (i.e. questionnaire completion) was voluntary; military superiors were not involved in evaluation recruitment and no incentives were offered.
Design
The present study is a real-world repeated-measures pre-post design. A baseline pre-treatment assessment was individually administered to participants the week prior to the commencement of the New Zealand Army Wellbeing Course (NZAWC) intervention. Follow-up assessments were individually administered at one- (T1) and three-months (T2) post-intervention to remaining participants.
Measures
Measures were selected based on established evidence of their validity and reliability, as well as ease of use and brevity. Scales were scored according to published methods, with higher scores representing more of the measured attribute. See Table 1 for references and descriptions of the measures used in the analyses.
Table 1. Assessment Measures and Associated Internal Consistency Cronbach’s Alpha Values.
| Domain | Measure | Description (and Cronbach’s alpha values) |
| Alcohol use | Alcohol Use Disorders Identification Test-Consumption (AUDIT-C; Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998)(22) | An internationally standardised and widely endorsed brief screen of drinking quantity and frequency on a normal day and the frequency of binge drinking (α=0.71). |
|
Drug use
|
Items derived from the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST; World Health Organization, 2010)(23) | Items assess the frequency of drug use and desire to use different types of drugs. Item phrasing was adjusted in order to assess pre/ post-intervention changes (i.e. ‘past three months’ was replaced with ‘past month’). |
| Aggression | 12-item short-form version of Buss and Perry’s (1992) Aggression Questionnaire (BPAQ-SF) (Diamond & Magaletta, 2011)(24) | Includes four sub-scales (physical aggression, verbal aggression, anger, hostility; α =0.83 0.83, 0.80, 0.82 respectively) as well as a combined total aggression score (α=0.91). |
| Perceived stress | Perceived Stress Scale-10 (PSS-10; Cohen & Williamson, 1988)(25) | A 10-item scale that has been used in numerous research investigations with AOD and military foci (α=0.83). |
| Anxiety | Brief Generalised Anxiety Disorder Screen (GAD-7; Spitzer, Kroenke, Williams, & Lowe, 2006)(26) | A seven-item anxiety screen that has been used extensively with pre- and post-deployment military populations and brief AOD-focused interventions (α=0.92). |
| Locus of control | Sapp and Harrod’s (1993) nine-item short-form version of Levenson’s (1974) Locus of Control Scale(27) | Comprises three locus of control dimensions: internal, chance and powerful Others (α=0.52, 0.65 and 0.82 respectively). |
| Emotion management | Salovey Mayer, Goldman, Turvey, and Palfai’s (1995) recommended 30-item version of their Trait Meta-Mood Scale (TMMS)(28) | Includes three sub-scales: attention (ability to attend to moods and emotions), clarity (ability to discriminate clearly among feelings) and repair (ability to regulate moods) (α=0.79, 0.82, and 0.65 respectively). |
Procedure
The procedure comprised participant referral and initial interview; baseline assessment on day 1 of the course; completion of the five-day NZAWC, and follow-up assessments one- and three-month post-intervention (with the same questionnaire battery administered at each assessment). The course was delivered in community centres on two New Zealand military bases.
To help standardise training, facilitate participant understanding and provide additional resources unable to be covered in-depth during the course, a participant manual was developed that incorporated relevant evidence-based strategies. Core areas targeted in the course included stress and reintegration, communication and relationships, anger and aggression, and AOD use (see Table 2 for details of course structure).
Table 2 The acceptance and commitment therapy protocol
| Day 1 | Theme: Introduction to ACT |
| Introduction and therapeutic agreement | |
| Orientation to ACT therapy | |
| Values exercises: army values; analysing values | |
| Commitment to behaviour change: setting therapeutic goals | |
| Homework: observing self | |
| Day 2 | Theme: Anger/aggression and communication |
| Understanding anger exercise: anger myths and control agenda; anger cycles | |
| Control agenda (exercises): white bears; suppressing emotion; what can you control? | |
| Creative hopelessness (exercise): personal cost of experiential avoidance | |
| Mindfulness and acceptance of anger emotions (exercises): mindfulness of anger; stare-down (adaptation of eyes on) | |
| Communication and anger: noticing emotion and function in communication | |
| Homework: observing emotion and function in communication | |
| Day 3 | Theme: Stress management |
| Self-as-context (metaphors/exercises): rugby field (adaptation of chessboard), observing the mind, I am, timeline | |
| Defusion and acceptance (metaphors): ‘Map and terrain’, ‘Passengers on the bus’, ‘Fighting the rip’, ‘Quicksand’, Tug-of-war’, Digging a hole’ | |
| Non-judgemental awareness/being present (mindfulness exercise): noticing thoughts | |
| Committing to valued action (exercise): managing stress Post-its | |
| Homework: identify stress-management strategies that don’t avoid stress | |
| Day 4 | Alcohol and other drugs |
| Alcohol and other drugs psychoeducation | |
| Alcohol as experiential control or avoidance (exercise): costs of using alcohol to avoid | |
| Mindfulness of urges: urge-surfing | |
| Functional analysis and value-guided behavioural choices (exercise): planning functional alternatives | |
| Homework: functional alternatives | |
| Day 5 | Setting the direction |
| Identifying values (metaphor/exercise): ‘65th Birthday’; values compass | |
| Committed action (exercise): perspective- and value-based behavioural actions | |
| Relapse prevention: remembering | |
| Generalising (combined meeting with soldiers and unit commanders): course learnings and leadership support |
Participants learnt various strategies and skills through a combination of short talks, large and small group exercises, individual activities and discussion of film clips. In-class workbook activities and between-session tasks were also used to help apply, extend and consolidate information. The courses were delivered by two facilitators: The first author, a senior clinical psychologist (PhD), facilitated all courses. The co-facilitation was divided between a registered counsellor (B.Couns; third author) and a clinical psychologist (PGDipClinPsych; fourth author), with support from postgraduate clinical psychology students.
Figure 1. Participant flow chart through the ACT intervention.
Data Analysis
To test the hypothesis that participants would experience improvements in alcohol/drug use, aggression, perceived stress, anxiety, locus of control, and emotion management from pre-treatment to post-treatment (1-month and 3-months). We calculated means for each of the measures. For each measure of interest, its pre-intervention level was compared against the 1-month post-course value and against the 3-month follow-up value. Aggregated measures were tested using a paired-samples t-test.
Table 3. Sociodemographic Characteristics for MSP at Pre-treatment, 1-month and 3-month Post-treatment
| Demographic Characteristic | Pre-treatment | 1-month Post-treatment | 3-month Post-treatment |
| N (%) | 292 | 136 | 117 |
| Sex | |||
| Male | 255 (87%) | 114 (83.8%) | 101 (86.3%) |
| Female | 36 (12.3%) | 22 (16.2%) | 16 (13.7%) |
| Unknown | 1 (0.003%) | ||
| Ethnicity/Nationality | |||
| New Zealand European | 47 (16.1%) | 29 (21.3%) | 22 (18.8%) |
| Māori | 116 (39.7%) | 51 (37.5%) | 46 (39.3%) |
| Pacific Islander | 33 (11.3%) | 13 (10%) | 13 (11.1%) |
| European | 74 (25.3%) | 36 (26.4%) | 30 (25.6%) |
| Asian | 7 (2.4%) | 2 (1.5%) | 0 (0%) |
| African | 1 (0.003%) | 1 (0.7%) | 1 (0.9%) |
| Other / Unknown | 14 (4.8%) | 4 (2.9%) | 5 (4.3%) |
| Age (years) | |||
| Under 20 | 22 (7.5%) | 6 (4.4%) | 6 (5.1%) |
| 20-24 | 167 (57.2%) | 77 (56.6%) | 69 (59%) |
| 25-29 | 57 (19.5%) | 26 (19.1%) | 23 (19.7%) |
| 30-34 | 16 (5.5%) | 12 (8.8%) | 8 (6.8%) |
| 35-39 | 11 (3.8%) | 5 (3.7%) | 2 (1.7%) |
| 40 and over | 12 (4.1%) | 8 (5.9%) | 6 (5.1%) |
| Unknown | 7 (2.4%) | 2 (1.5%) | 3 (2.6%) |
Table 4 shows the results of paired-samples t-tests evaluating the impact of the treatment intervention on participants’ scores for each of the measures at pre- and post-treatment (1- and 3-month). Effect sizes were calculated using Cohen’s d. As indicated in Table 4, significant pre- to post-treatment improvements across all measures at 1-month and 3-month follow-ups. Moderate effect sizes are observed for changes in alcohol use, aggression, perceived stress, anxiety and emotion management. A particularly large effect was detected for the verbal subscale of the Buss-Perry Aggression Questionnaire (BPAQ-SQ)(24).
While the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST)(23) drug use and desire to use drugs items were administered to participants at both pre- and post-treatment, the only substances with sufficient responses to allow analysis, for either use or desire, was cannabis. Tobacco was not a primary concern of referrals to this intervention so was excluded as a variable from the analysis. At 1-month post-treatment 8 participants reported lower cannabis use/urges, while 3 increased their use/urges and 3 reported no change (not including consistent non-smokers) (Wilcoxon Z= -1.29, p= 0.10). At 3-months post-treatment 5 participants reported lower cannabis use/urges, 4 increased their use/urges and 0 reported no change (Wilcoxon Z= -1.48, p= 0.07). Although these changes in cannabis use are not significant, the changes are in the expected direction. A high frequency of no change for drug use/desire was largely due to a lack of use/desire at pre-treatment, which was maintained through to post-treatment. Consequently, the distribution of changes in drug use does not meet the requirements of normality and should therefore be interpreted with caution.
Table 4. Mean () Differences in Dependent Variables for those completing Pre-treatment and Post-treatment Assessment with Standard Errors of the Mean (SEM), and Effect Sizes (Cohen d)
| Pre-treatment | 1-month Post-treatment | Pre-treatment | 3-month Post-treatment | |||||
| Dependent Variable | (SEM) | (SEM) | t (df) | d | (SEM) | (SEM) | t (df) | d |
| Alcohol Use | 6.64 (0.27) | 5.03 (0.26) | 6.90 (115)** | 0.64 | 3.41 (0.38) | 2.90 (0.32) | 6.18 (98)** | 0.62 |
| Aggression Total Score | 2.04 (0.07) | 1.76 (0.06) | 4.53 (118)** | 0.42 | 2.28 (0.09) | 1.95 (0.07) | 3.66 (107)** | 0.35 |
| Physical§ | 2.22 (0.09) | 1.89 (0.08) | 4.59 (127)** | 0.41 | 2.41 (0.10) | 2.02 (0.08) | 4.00 (112)** | 0.38 |
| Verbal§ | 2.11 (0.08) | 1.40 (0.05) | 11.02 (128)** | 0.97 | 2.30 (0.10) | 1.53 (0.07) | 8.78 (110)** | 0.83 |
| Anger§ | 1.87 (0.09) | 1.55 (0.07) | 3.88 (129) ** | 0.34 | 2.15 (0.11) | 1.83 (0.08) | 2.73 (113) ** | 0.26 |
| Hostility§ | 2.02 (0.09) | 1.72 (0.06) | 3.76 (126)** | 0.33 | 2.23 (0.09) | 1.95 (0.08) | 2.67 (112)** | 0.25 |
| Perceived Stress | 17.48 (0.61) | 13.48 (0.55) | 6.61 (117)** | 0.61 | 18.12 (0.70) | 15.16 (0.60) | 3.62 (106)** | 0.35 |
| Anxiety | 5.81 (0.46) | 3.68 (0.37) | 4.97 (129)** | 0.44 | 6.65 (0.55) | 4.37 (0.44) | 4.46 (110)** | 0.42 |
| Locus of Control Chance§ |
7.52 (0.20) |
7.07 (0.20) |
2.36 (135)* |
0.20 |
7.97 (0.22) |
7.28 (0.23) |
2.72 (115) ** |
0.25 |
| Powerful Others§ | 7.81 (0.26) | 6.89 (0.21) | 3.62 (135)** | 0.31 | 8.32 (0.28) | 7.47 (0.26) | 2.84 (115)** | 0.26 |
| Emotion Management Total | 100.12 (1.20) | 106.71 (1.26) | 5.87 (126)** | 0.52 | 98.33 (1.27) | 103.61 (1.28) | 4.10 (110)** | 0.39 |
| Attention§ | 41.61 (0.66) | 45.76 (0.65) | 7.17 (128)** | 0.63 | 41.29 (0.70) | 44.89 (0.66) | 5.54 (112)** | 0.52 |
| Clarity§ | 37.40 (0.57) | 38.83 (0.60) | 2.66 (129)* | 0.23 | 36.29 (0.61) | 37.43 (0.58) | 2.00 (110)* | 0.19 |
Note. Analysis-by-analysis case exclusion resulted in n ranging from 53 to 78. § = an abbreviation of ‘subscale’. * p < 0.05 ** p < 0.01. Two pre-treatment columns are provided as numbers differed between comparison samples (pre-intervention and 1-month vs 3-month samples)
Discussion
Support was found for the hypothesised pre- to post-intervention reductions in participant levels of alcohol consumption, aggression, perceived stress, anxiety, powerful other loci of control and emotion management. One of the greatest effects concerned the alcohol consumption reduction with significant, moderate-sized reduction observed at both 1-month and 3-month post-intervention. This reduction could be attributed to the development and use of a combination of ACT mindfulness and acceptance skills and values-guided committed behavioural action. Participants were shown how to crystallise values that were personally meaningful and to commit to behaviours which were congruent with these values (e.g. take up different leisure activities), an outcome of which may have been reduced alcohol consumption.
Another potential explanation for reductions in alcohol consumption relates to the context in which MSP received treatment. Many of the MSP attended the NZAWC as a result of disciplinary issues, and so may have reduced their drinking to avoid further disciplinary action and/or were ordered to abstain from alcohol. In addition to this, the AOD-related psycho-education may have sensitised some participants to the adverse health effects of alcohol consumption, which may have contributed to a reduction in drinking. In this regard, it is unclear the extent to which reductions in alcohol consumption can be attributed to the NZAWC protocols, the context within which the treatment was undertaken, or some combination of these.
Significant, moderate reductions in total aggression and the four subscales (verbal and physical aggression, anger and hostility) were also found. The observed decrease in aggression scores demonstrates desired change in accordance with ACT’s model of psychological flexibility and indicates a possible decrease in the use of experiential avoidance. For example, by learning to observe their internal experience from a self-as-context viewpoint, participants potentially increased their present moment awareness of impulses to behave in aggressive ways (that have previously functioned to externally discharge the unpleasant emotional experience). With this increased awareness, it follows that there was increased opportunity to consciously accept the presence of the impulse and, therefore, greater scope for the defusion of psychological events (e.g. anger-related thoughts and impulses to act on these). This in turn could enable participants to exercise increased control of their overt behaviour so that behaviour congruent with their valued directions was more possible (e.g. inhibition of aggression was more possible; therefore, it was less likely to detract from commitment to values-directed behaviours). Eifert et al. (2006) refer to this quality of values-guided behavioural flexibility, resulting from increases in psychological flexibility, as ‘response-ability’, and assert that it increases the likelihood of goal attainment(29).
Moderate reductions in levels of perceived stress and anxiety were also found. These reductions may be due to participants having learnt to make room for experiences of stress and anxiety by observing and allowing them to come and go as harmless psychological events without attempting to control them (in accord with the ACT-based open acceptance of one’s immediate experience), which in turn may have increased their capacity to commit to values-directed behaviours. Thus, the accumulation of stressors is decreased given there is less experiential avoidance and more committed action, and, therefore, decreases in levels of perceived stress and anxiety are reinforced. This aligns with previous research supporting ACT’s efficacy for the treatment of stress and anxiety(18, 30, 31) and its efficacy in the form of brief intervention(18).
Hypothesised reductions in participant drug use and desire to use drugs were not supported. Results indicated that, in addition to alcohol, cannabis (excluding tobacco) was the most commonly used drug by the participants and that no significant decrease in either the use or desire to use cannabis was found between pre- and post-treatment. A possible explanation for the lack of reduction in both the use and desire to use cannabis may relate to the small number of reported users, as most participants were primarily referred to treatment for alcohol-related disciplinary concerns. A large number of participants reported no drug use or desire to use at pre-treatment, thereby increasing the likelihood of no change from pre- to post-treatment.
Results showed support for the hypothesised increase in emotion management skills. There was a moderately strong effect found for the improvement in overall emotion management and in ability to attend to moods and emotions and discriminate clearly among feelings. These results may relate to a continued increase in awareness of emotions (more generally) in line with taught/learnt ACT acceptance strategies.
Non-significant differences between 1-month and 3-month results across the other variables suggest the positive outcomes hold over time, indicating no evidence of relapse, but little of continued improvement either. It may be that participant changes do not extend beyond 1-month; further post-intervention follow up over a longer period could help clarify the pattern of longer-term change. Some form of refresher/reminder of relevant course material (e.g. in-person follow-up sessions, emails, texts, phone applications) could also be introduced post-intervention to help MSP continue to build on gains from the course.
Several limitations were identified, mostly related to the early developmental stages of the NZAWC. Firstly, given the small sample size, statistical power was limited; future analyses with a larger sample of MSP, and more follow-up data, would enable pre- and post-treatment comparisons with greater power. Secondly, the current study was not a randomised controlled trial (RCT), nor did it have a control group; therefore, the findings should be interpreted with caution. Future investigations into the course’s treatment efficacy would benefit from employing a RCT; or, at the least, a wait-list control group should be introduced to the study, requiring earlier referrals of MSP to treatment to enable the organisation of such an addition. Thirdly, frequency and intensity measures are useful for identifying patterns of drinking behaviours over time. However, as Dufour (1999) pointed out, these forms of self-report screens are less reliable for those with irregular drinking patterns as it relies upon respondents calculating an average drinking pattern. Instead, Dufour suggested the use of graduated frequency measures or drinking diaries to enhance the accuracy of data collection(32). The expense and degree of labour to administer these forms of measurement meant they were not considered for this study but are important considerations in the future.
Participant selection was beyond the control of the researchers, as MSP were referred to the course in accordance with military protocol. Therefore, extraneous variables such as concurrent pharmacological intervention and the medical histories of MSP were unknown. Additionally, logistical complications associated with this population (e.g. deployment, frequent field exercises) hindered follow-up data collection, as did attrition due to the protocol of ‘due diligence’ (i.e. some MSP who attended the course were inevitably going to be discharged regardless of the outcome of their treatment and were sent to attend as part of a duty of care). Relatedly, the detected effects of the NZAWC may partly reflect a favourable client-related bias as the remaining MSP (i.e. those completing follow up) constitute those referred for less problematic treatment concerns than MSP referred out of due diligence. In addition, although there were effects of noteworthy magnitude, it is unclear which specific treatment processes caused them. The design of a RCT and inclusion of ACT process measures (e.g. the Acceptance and Action Questionnaire(33)) should help to elucidate what these active treatment processes might be and to interpret findings from treatment effects with greater theoretical consistency. Future research could also include an extended follow-up assessment period to assess the longevity of observed treatment effects.
The current study represents an important step in addressing the paucity of research surrounding the specific treatment needs of MSP suffering from AOD and mental health difficulties. While the findings regarding the NZAWC efficacy are preliminary, they are promising. Levels of alcohol consumption and distressing emotions reduced over the course of treatment, with indications that treatment may have imparted valuable emotion detection and management strategies for MSP. Based on the initial evidence, further exploration of the NZAWC treatment efficacy is warranted, as is a more general investigation of ACT’s clinical utility with military populations.






