Abstract
Background: This preliminary study offers the first health-related assessment of United States (US) immigrant veterans, who comprise a population of more than 500 000. It builds upon research showing that a number of variables relate to veterans’ health experiences, including race, ethnicity and socioeconomic status.
Purpose: To assess levels of disability reporting among foreign-born veterans in comparison with other populations.
Materials and Methods: We analysed 2011–2015 data from the United States Census Bureau 5-Percent Public Use Microdata Sample (PUMS) to compare disability reporting among foreign-born veterans, native-born veterans, foreign-born non-veterans and native-born non-veterans.
Results: Middle-aged foreign-born veterans were less likely to report a disability than native-born veterans and native-born non-veterans, but more likely to report than fellow non-veteran immigrants. When hearing disability—which has been shown to disproportionately impact veterans—was examined independently, foreign-born veterans reported at lower rates than native-born veterans, and at higher rates than native-born and non-veterans immigrants. Native-born veterans consistently reported disabilities at the highest rates.
Conclusion: Foreign-born veterans are distinct from both other veterans and other immigrants in respect to their levels of reported disability. These results could inform research and practice in the US, as well as other countries with diverse and/or foreign-born veteran populations.
Keywords: veteran, immigrant, disability, minority health
Conflict of Interest: None declared.
Introduction
In research on the health of United States (US) veterans, an important group has been overlooked — more than 511 000 immigrants. Foreign-born former service members comprise a growing proportion of the veteran population. Between 1995 and 2016, the total number of veterans in the US fell from 26.1 million to 18.8 million while the number of veterans who were immigrants remained relatively stable. Foreign-born veterans constituted two per cent of all veterans in 1995 and three per cent by 20161. In 2016, 16 per cent of immigrant veterans were from Mexico and 13 per cent were from the Philippines. Six per cent hailed from Germany, and another six per cent from Canada. Haiti, India, the United Kingdom, the Dominican Republic, China and Italy were each the birthplaces of between two and three per cent of living veterans. The remaining 42 per cent were from a variety of countries. In comparison with foreign-born non-veterans, foreign-born veterans were relatively advantaged; they were more likely to have completed college, more likely to hold positions in management—as opposed to service occupations—more likely to have public health insurance coverage and less likely to have limited English language proficiency1.
This preliminary study is the first, to our knowledge, to provide a health-related assessment of immigrant veterans. Generally, analyses of data from the US Department of Veterans Affairs (VA) focus on a variety of demographic characteristics of the veteran population, including race and ethnicity, but do not separate out birthplace for consideration2–7. A 2010 VA report, for example, showed that white veterans were more likely to report that their health was ‘excellent’, ‘very good’ or ‘good’ than their Black, Asian, Pacific Islander, American Indian/Alaska Native and Hispanic counterparts were8. However, the report did not define foreign-born veterans within or apart from larger minority subgroups. Our study intends to determine if immigrant veterans, too, have unique health-related experiences.
Our findings could inform research and practice, not only in the US, but also in other countries where health-related information on minority and foreign-born veteran populations is somewhat limited. Veterans Affairs Canada (VAC) recently reported on the demographics of Canadian military families, including characteristics such as gender, place of residence, age and family composition, but noted that additional demographic data, such as language and ethnicity, could ‘inform policies, programs and services’9. Reports from the United Kingdom (UK) and Australia suggest that, while the US has relatively large military and veteran populations10, it is not unique in having diverse ranks. More than five per cent of the UK military population is of non-UK nationality11 and more than two per cent of the Australian Defence Force in 2015 spoke only a language other than English12. Meanwhile, multiple European countries, as well as Canada, are facing challenges recruiting citizens for their armed forces, and commentators suggest that foreign-born populations could serve as willing and able recruits13,14.
In this broader context, our study offers perspective on how foreign-born veterans from one of the largest militaries in the world fared health-wise in comparison with both native-born veterans, and native-born and immigrant non-veterans. In addition to providing the first detailed analysis of immigrant veterans, an understudied subgroup, it underscores a point governments and researchers must bear in mind when it comes to studying and alleviating the health impacts of military service: veterans’ experiences are highly variable. Our finding, that foreign-born former service members are distinct from both the US veteran population and the US immigrant population, in respect to their levels of reported disability, relates to diverse studies on whether former service members are more or less healthy than their non-veteran counterparts, and recent reports from both the Australian Department of Veterans’ Affairs and VAC suggesting that a variety of forces—including demographic factors and membership in particular social groups—shape general and health-related post-service experiences15,16. It underscores the necessity for researchers and clinicians to conceptualise health studies and systems that pay heed to the potential importance of individuals’ social and ethnic backgrounds.
Materials and Methods
The dataset used for this study was the American Community Survey 5-Percent Public Use Microdata Sample (PUMS) covering the years 2011–2015 (US Census Bureau). The PUMS data contain information on five per cent of the non-institutionalised US population. This dataset is the largest nationally representative, publicly available dataset in the US. While other nationally representative datasets exist, such as the Current Population Survey, Panel Study of Income Dynamics or National Health Interview Survey, none is large enough to capture a representative sample of foreign-born veterans, given their limited numbers relative to other population groups.
To retain a focus on individuals eligible to serve in the military, individuals under 17 years of age were dropped from the sample. Individuals in the data were coded as either native-born non-veterans, native-born non-veterans, foreign-born non-veterans or foreign-born veterans. Two measures of disability were used: (1) the reporting of any disability (which included self-care difficulty, hearing difficulty, vision difficulty, independent living difficulty, ambulatory difficulty or cognitive difficulty); and (2) the reporting of a hearing disability, which prior research has shown to disproportionately affect veterans17.
Demographic characteristics of the four groups were computed. Disability rates were calculated for four age groups: ages 17–35, 36–50, 50–64 and over 65, plotted graphically. To determine what demographic factors were associated with reporting of disabilities, odds ratios were obtained from logistic regressions according to nativity and veteran status. Variables included in the model were measures of nativity (foreign-born=1, native-born=0), age, insurance status (has insurance=1, 0 otherwise), gender (female=1, male=0), veteran status (veteran=1, nonveteran=0), race/ethnicity (Black, Hispanic, Other) and education status (less than high school, high school, some college, college and graduate degree).
To determine the impact of being foreign-born on disability status among veterans while controlling for other variables, logit models, including the variables described above, were estimated and marginal effects were computed at sample means. The marginal effects reported give the percentage point impact of the characteristic on the likelihood of reporting disability. Significance on the ‘foreign-born’ variable would indicate a differential likelihood of foreign-born veterans reporting disabilities relative to native-born veterans. To determine whether significant differences in disability reporting between native and foreign-born veterans are due to differences in sample mean characteristics, the Oaxaca-Blinder method was used to decompose differences into that proportion attributable to sample characteristics and the estimated coefficients18.
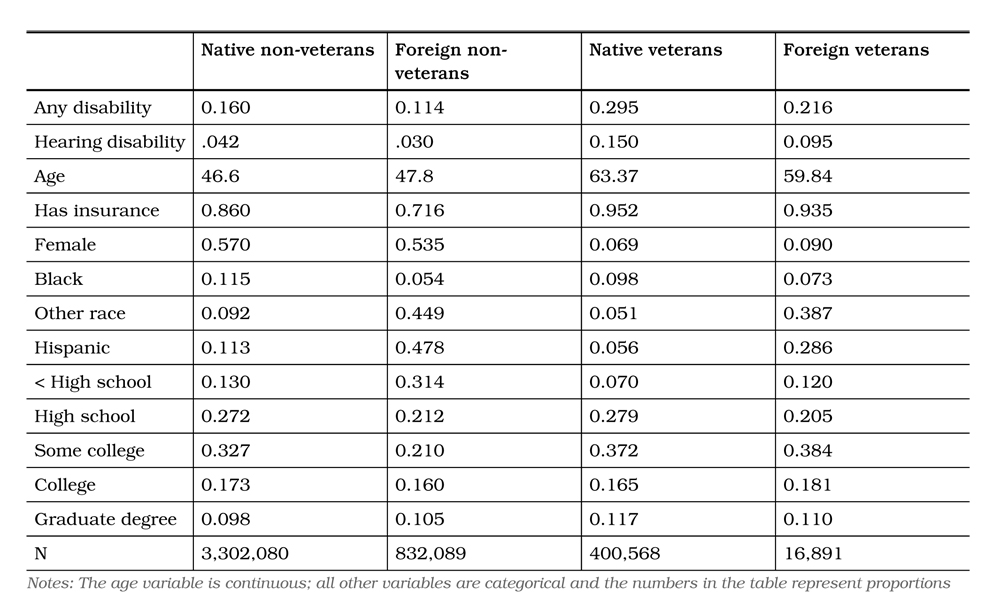
Table 1: Demographic characteristics of native-born veterans, foreign-born veterans, native-born non-veterans, and foreign-born non-veterans, United States, 2011–2015
Results
The data contained a total of 4 551 628 individuals over age 17. Of these, 3 302 080 (72.5%) were native-born non-veterans, 832 089 (18.3%) were foreign-born non-veterans, 400 568 (8.9%) were native-born veterans and 16 891 (0.4%) were foreign-born veterans. The 16 891 foreign-born veterans represented approximately four per cent of the total veteran population. Table 1 reports demographic characteristics. Both native- and foreign-born veterans reported higher rates of disability than their non-veteran counterparts did. They were also older and more likely to be insured. Consistent with prior research1, foreign-born veterans were most likely to have greater than a high school education followed by native veterans, native non-veterans and foreign-born non-veterans.
Figure 1 shows rates of reporting any disability. Overall, native veterans reported the highest rates of disability among the four groups. In middle age (35–65 years old), native non-veterans reported disabilities at the second highest rate, followed by foreign veterans and foreign non-veterans. Reporting of disability increased sharply after age 55. Overall differences across the four groups were smallest for the over age 65 population. While there was a consistent pattern of reporting rates between age 35 and 65, with native veterans reporting the highest rate, native non-veterans the second highest, foreign veterans the third highest, and foreign non-veterans the fourth highest, after age 65, foreign non-veterans reported slightly higher disability rates than foreign-born veterans. In the under age 35 group, native veterans reported disabilities at the highest rate, with foreign veterans reporting at the second highest rate, followed closely by native non-veterans and foreign non-veterans.
Figure 1: Any disability by age nativity and veteran status, United States, 2011–2015
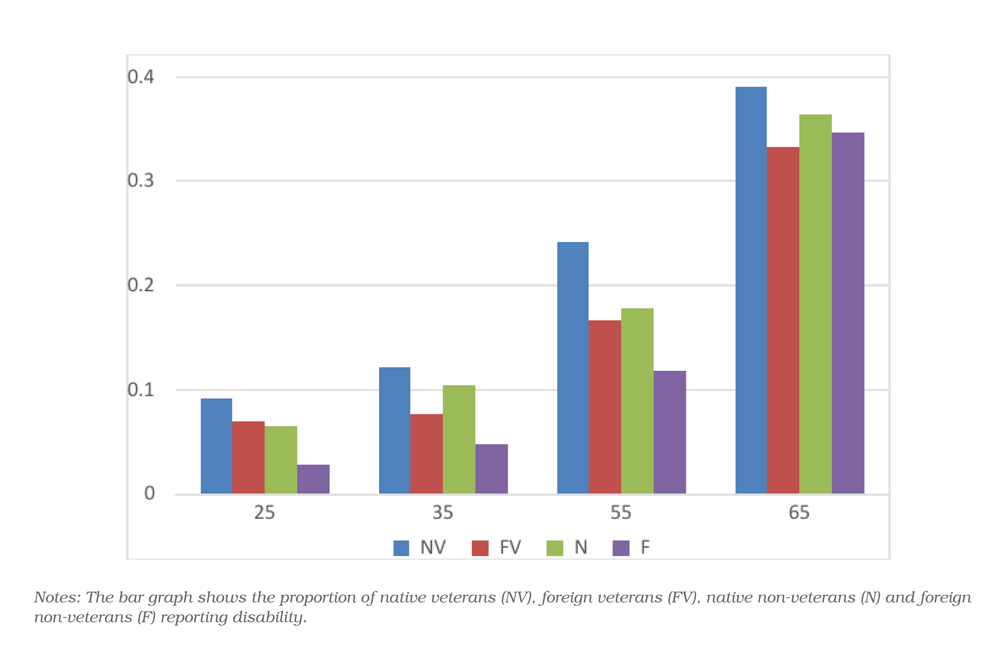
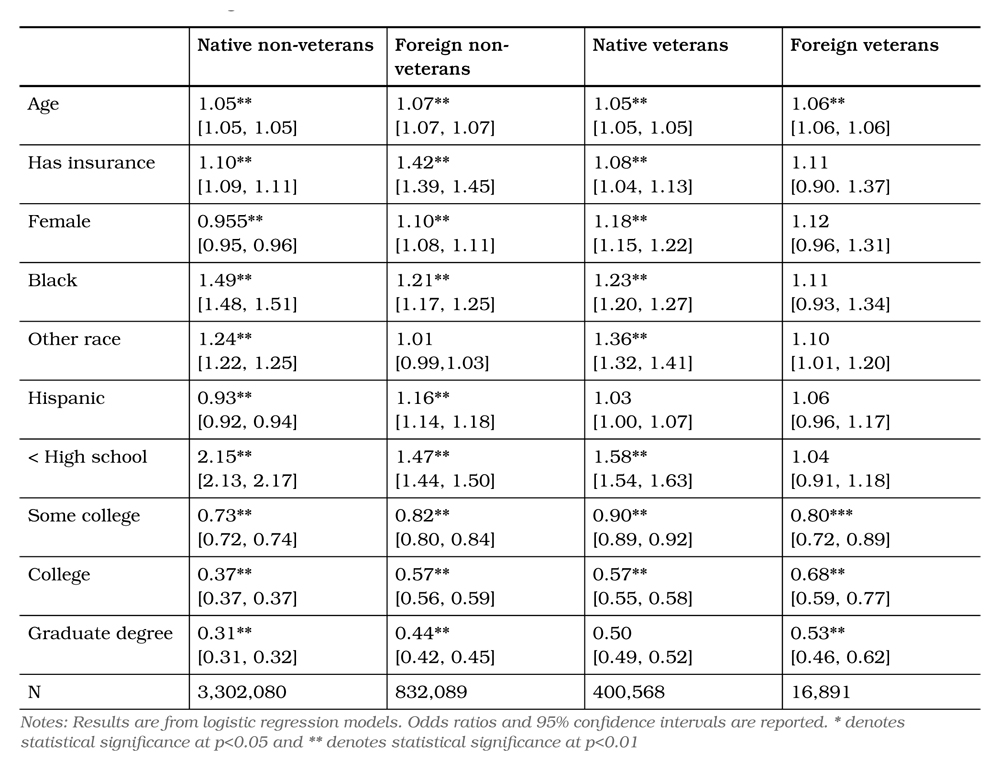
Table 2 reports odds ratios from logistic regressions. For all four groups, age was the strongest predictor of reporting a disability. Insurance status was significant for three of the four groups, with the strongest impact on foreign non-veterans. African Americans were more likely to report disabilities in three of the four groups, while results for the female and Hispanic variables varied in direction, size and significance across the four groups. The education variables had the largest impact on reporting of disability for all groups, with lower rates of education significantly increasing the odds of reporting a disability. The differences exhibited in Figure 1 persist when predicted values at sample means are computed, suggesting the differences are not due to differences in age, race/ethnicity or education level.
Similar results were found when focusing on the reporting of a hearing disability, but differences between the groups were larger and more dependent on veteran status than on nativity (Figure 2). As with the reporting of any disability, the reporting of a hearing disability was highest for native veterans and increased sharply with age for all groups. Foreign-born veterans were the next most likely group to report a hearing disability, unlike the reporting of any disability where native non-veterans were the second most likely to report any disability. While group differences in reporting any disability became smaller after age 65, group differences in the reporting of a hearing disability became larger with age, and rates of reporting of foreign veterans remained higher than foreign non-veterans.
Table 2: Any disability, logistic regression results, native-born veterans, foreign-born veterans, native-born non-veterans, and foreign-born non-veterans, United States, 2011–2015
Odds ratios from logistic regressions are reported in Table 3. As with the reporting of any disability, age and education were the strongest predictors of reporting a hearing disability and showed a similar pattern as the reporting of any disability, with lower levels of education being positively associated with reporting affirmatively. For native non-veterans, having insurance was negatively associated with reporting a hearing disability but was positively associated for foreign non-veterans and native veterans. Unlike the reporting of any disability, being African American was negatively associated with reporting a hearing disability, and the odds ratios for females were less than one and significant for all groups. The differences exhibited in Figure 2 also
persist when predicted values at sample means are computed, again suggesting the differences are not due to differences in age, race/ethnicity or education level.
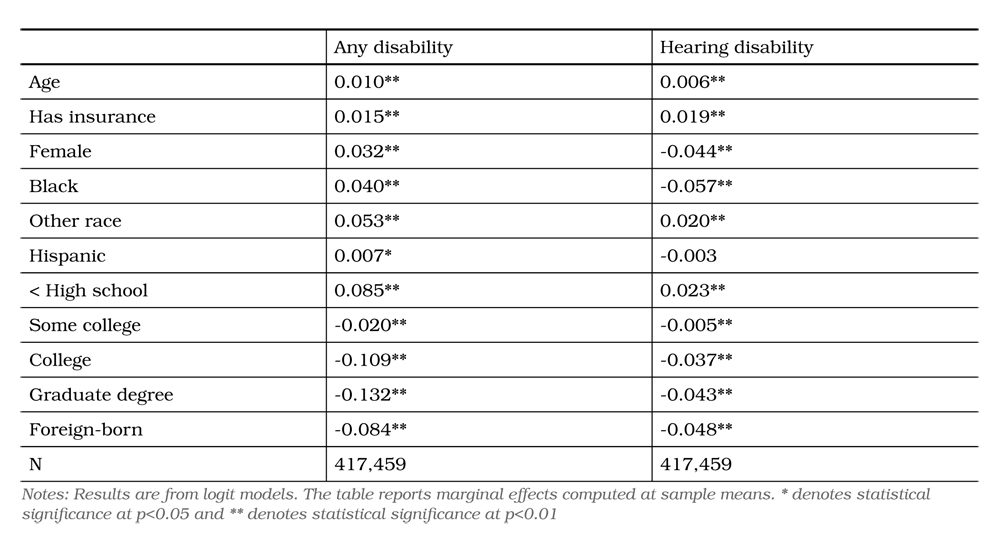
Results from logit models are reported in Table 4 and are consistent with the findings from logistic regression results reported in Tables 2 and 3. For the reporting of any disability, age, insurance status, female, and race/ethnicity were positively associated with reporting disability. Educational attainment and being foreign-born were associated with lower levels of reporting disability. Results suggest that foreign-born veterans were 8.4 per cent less likely to report having a disability than their native-born counterparts were when controlling for other factors. Focusing only on hearing disability found similar results. As in the logistic regression results, results
were similar except for female and race/ethnicity now being associated with a lower likelihood of reporting disability. Results suggest that foreign-born veterans are 4.8 percentage points less likely to report having a hearing disability than their native-born counterparts when controlling for other factors.
Figure 2: Hearing disability by age, nativity and veteran status, United Sates, 2011–2015
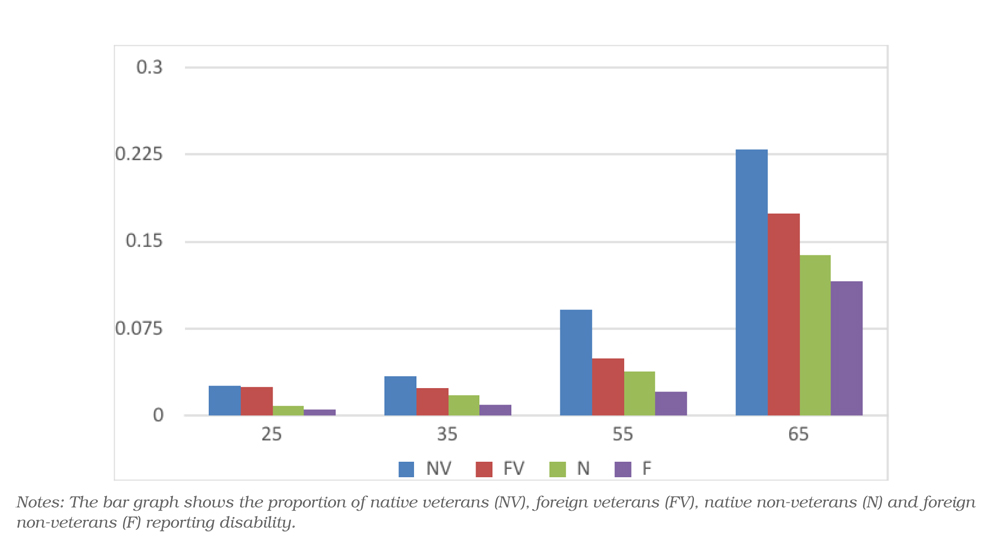
Table 3: Hearing disability, logistic regression results, native-born veterans, foreign-born veterans, native-born non-veterans, and foreign-born non-veterans, United States, 2011–2015
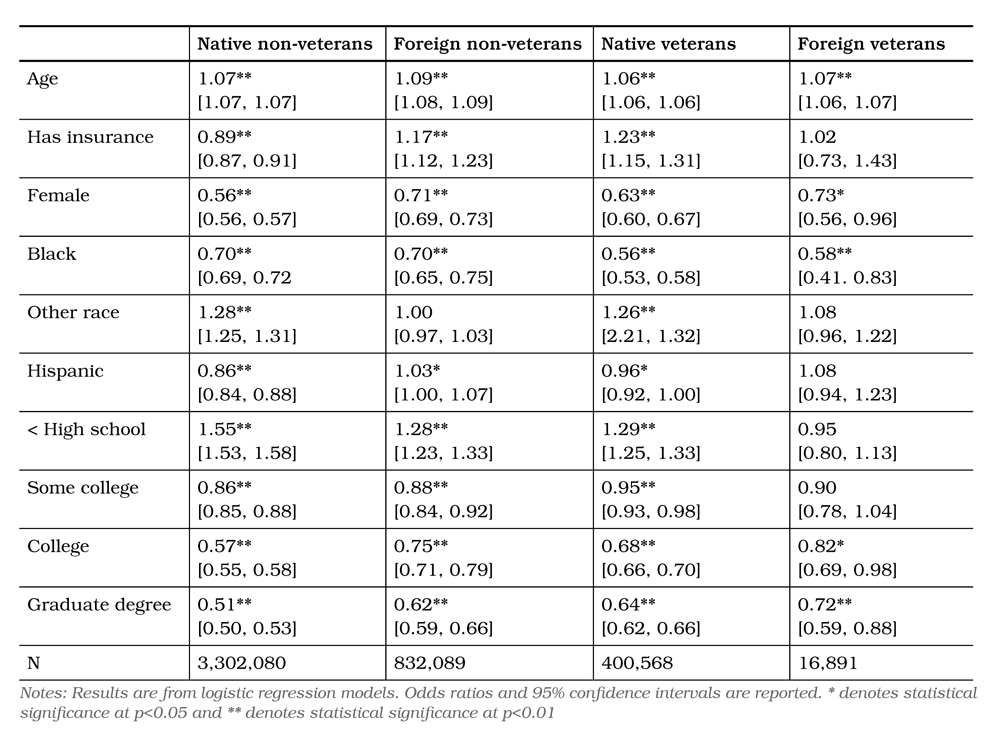
Table 4: Predictors of disability among veterans, United States, 2011–2015
Discussion
A variety of characteristics impacted overall levels of disability reporting. Education level was the strongest predictor. Higher levels of education were associated with a lower likelihood of disability reporting, confirming previous studies that point to education and social class as important determinants of health19,20. Also consistent with other studies, being female or African American was associated with a higher likelihood of reporting a disability other than hearing impairment21. Predictably, the reporting of disability increased with age for all groups. Veteran status increased the likelihood of disability reporting, while foreign-born status was found to decrease the likelihood of disability reporting.
We show that hearing impairment disproportionately impacts both native and immigrant veterans while other disabilities disproportionately impact native veterans, but not immigrant veterans. We separated out hearing impairment as a measure because veterans are 30 per cent more likely to experience severe hearing impairment than non-veterans17. As with the reporting of any disability, the reporting of a hearing disability was highest for native veterans and increased sharply with age for all groups. Foreign-born veterans, across all age groups, were the next most likely group to report a hearing disability, unlike the reporting of any disability where native non-veterans were the second most likely to report any disability after age 35. While group differences in reporting any disability became smaller after age 65, group differences in the reporting of a hearing disability became larger with age, and rates of reporting of foreign-born veterans remained higher than foreign-born non-veterans. These findings suggest that veteran status impacts disability reporting levels among immigrants, but further research would explain why hearing impairment is disproportionately common among both native and immigrant veterans while other disabilities are disproportionately common among native veterans, but not immigrant veterans.
We found that foreign-born veterans reported lower rates of disability than native veterans or native non-veterans in middle age, but not in the over age 65 group. In the elderly population, foreign-born veterans reported disabilities at the lowest rates of any of the four groups. This could be attributed to a greater health status among foreign-born veterans compared to non-veterans in earlier life due to relatively higher socioeconomic status and access to institutional supports, such as the military and veterans’ health systems. The finding correlates with previous research demonstrating that differences in disability rates between veterans and non-veterans decline with age22.
This study highlights a subcategory of the veteran population that, in middle and old age, reports disabilities at lower rates than both the native veteran and the native non-veteran populations do. It contrasts with prior work showing that disability reporting is generally higher among US veterans than non-veterans23. Wilmoth, et. al. reveal that 30.1 per cent of veteran women and 29.8 per cent of veteran men report some limitation or disability, compared with 23.8 per cent of non-veteran women and 21.7 per cent of non-veteran men.24.
Our findings build upon prior work regarding the existence of a healthy soldier effect, in the form of decreased risk of mortality among veterans25, as well as more recent research maintaining that the impact of military service on overall well-being is hardly uniform15,26. Studies on military service in the life course reveal that long-term physical impacts of serving in the military depend on a variety of factors, including prior health, socioeconomic status and conditions of service—for example, whether or not an individual was stationed in a combat zone or served during a war27–30. Previous studies have also shown that minority veterans have distinct experiences receiving diagnoses and accessing health services2,4–7. Our study suggests that immigrants, too, have unique post-service experiences, though further research is needed to determine which factors shape key health outcomes, including individual levels of disability reporting.
In addition to relating to research on the health impact of military service in the life course, our findings build upon studies of immigrant health in various countries. Research on the so-called ‘healthy immigrant effect’ maintains that when individuals first migrate, they report better overall health than native populations in their adopted countries, but that their health advantage decreases over time31,32. Researchers note that a variety of characteristics can influence immigrants’ health status, including birth country, socioeconomic status and access to social and institutional supports33–35. Recent work has indicated the importance of acknowledging ‘selective migration’—that new immigrants have characteristics that are distinct from, and relatively favourable in comparison with, overall native-born populations36,37. One study, for example, maintains that migrants are generally mobile, so they should be compared not to all natives, but instead to native-born ‘movers’38. A 2015 systematic review of immigrant health in at least 10 countries, offers a wide-ranging perspective that goes beyond individual socioeconomic factors; underscoring the idea that the health of immigrants—especially undocumented immigrants—is intertwined with public policies, it suggests that there is a direct link between laws intended to restrict immigration and individuals’ access to health services39. While further research is needed, this previous work suggests that veteran immigrants may be distinct from the larger US foreign-born population in terms of disability reporting, not only due to individual socioeconomic characteristics, but also because they have conditional access to federally sponsored veterans’ benefits.
Our work highlights various additional areas for further research. Immigrant veterans’ educational, vocational and family status, as well as a wider range of predictor variables, available in the PUMS files, should be examined. Subgroups within foreign-born veteran populations could also be analysed according to factors such as country of origin, age, race/ethnicity, gender and education level. The impact of policy-related variables, such as laws governing access to veterans’ health benefits, should be further explored, as should the health care experiences of foreign-born and other minority veterans, especially in public health systems geared towards military and veteran populations. Finally, transnational comparisons of veterans’ disability reporting, which consider demographic and socioeconomic characteristics, are also warranted.
This preliminary study had strengths and limitations. Chretien, et al. recently argued that measuring the long-term health impacts of military service is challenging, and asserted that longitudinal studies are necessary40. Our work focuses on measures included in the PUMS—one of the few data sets that provides a glimpse of health information about this understudied population and allows relevant comparisons with others. However, the health information in the PUMS file is limited; therefore, the analysis was restricted to the reporting of disability rather than more robust measures of health status that may be available in smaller datasets. Smaller datasets, on the other hand, may not yield adequate samples of foreign-born veterans. As such, we capitalised on a large, nationally representative dataset containing almost 17 000 records of foreignborn veterans to provide an in-depth analysis of demographics and disability reporting.
Conclusion
Our conclusion that immigrant veterans’ levels of reported disability are different from both other former service members and other immigrants has important practice, research and policy implications. It signals that health care providers and researchers should consider demographic and social factors when devising studies of, offering care to and designing health systems for former service members. By focusing on a previously invisible subcategory within a veteran population, we verify and call into question aspects of studies regarding the long-term health impacts of military service and immigration. Our findings underscore the notion that there is no universal rule about whether veterans and/or immigrants are healthier or less healthy than their non-veteran or non-immigrant counterparts are. They also demonstrate that the health status of veterans is shaped by a variety of social circumstances including, but not limited to, their experiences as service members.
Corresponding Author: Jessica Adler, jadler@fiu.edu
Authors: J Adler1, T Page1
Author Affiliations: 1 Florida International University



