Abstract
The 2000-2005 quinquennium saw a marked drop in the number of Australian Defence Force (ADF) personnel suffering from malaria following the deployment of an Australian Army Malaria Institute (AMI) outbreak investigation team to Timor Leste and improved compliance with various prevention measures. The field evaluation of novel drug regimens using currently registered and new drugs also contributed to the reduced number of malaria cases overseas and after return to Australia. The main purpose of some of these studies was to determine the tolerability and effectiveness of more user friendly drug regimens, such as shorter courses of primaquine and 3-day courses of tafenoquine for post-exposure prophylaxis against vivax malaria. Clinical/ field studies were also conducted with atovaquone/proguanil (Malarone®), loading doses of mefloquine, and a new artemisinin drug – artemisone. All of these investigations yielded positive results. Another landmark study – the first Phase III study in which weekly tafenoquine was taken for six months by non-immune individuals – showed that Australian soldiers could be protected against both falciparum and vivax malaria while in Timor Leste without having to take a post-exposure primaquine eradication course upon return to Australia.
In addition to documenting increasing drug resistance of malaria parasites in various parts of the Asia/Pacific region, molecular markers and changes associated with parasite resistance to antimalarial drugs were identified. An in vitro field test for assessing the drug susceptibility of Plasmodium vivax was also developed and, for the first time, successful transfection of P. vivax genes to continuously cultured P. falciparum enabled antifolate drugs to be screened in vitro for their activity against P. vivax. Furthermore, various laboratory/epidemiological studies and mathematical models were developed to investigate factors involved in the evolution and spread of drug resistance, such as mutation patterns, antigenic variation, loss of fitness, and inappropriate treatment.
In ongoing efforts to improve protection against mosquito bites, the effectiveness of various repellents/ insecticides applied to skin, clothing and tents were evaluated in military training areas in Queensland and the Northern Territory. Mosquito control measures, including the use of newly-developed tools, were instrumental in controlling the outbreak of both malaria and dengue fever in Timor Leste. Furthermore, investigations in Australia, Vietnam and China indicated the potential value of novel molecular-based and other tests for identifying and controlling the spread of mosquitoes transmitting malaria, dengue and Japanese encephalitis. In view of the ADF’s increasing exposure to arboviral diseases, further clinical studies were conducted to assess the tolerability and immunogenicity of dengue and Japanese encephalitis vaccines and prelicensure studies were started to determine the effectiveness of new vaccines.
Background
In 1943, an impressive medical and scientific group was assembled by Brigadier Neil H. Fairley in response to the devastating effects of malaria being experienced by allied soldiers deployed to the South Pacific. In just three years (1943-1946), the ‘high priority’ Land Headquarters Malaria Research Unit, based at Cairns in North Queensland, obtained considerable new information about the activity of drugs such as proguanil (Paludrine®) against different stages of the human malaria parasite and was able to protect soldiers remarkably well against malaria infections.1
By the mid-1960s, there were renewed concerns regarding the ability of antimalarial drugs to provide adequate protection against malaria. In 1965, Professor Robert H. Black, Army Consultant in Tropical Medicine and a previous investigator at the Cairns Unit, proposed that the Army should conduct malaria studies to address the growing drug resistance problem in Southeast Asia.2 As a result, a small research unit comprising two scientists and a few technicians was established at the University of Sydney in 1966. Although additional positions were established later, research activities were hampered by frequent staff changes and cramped facilities.
The relocation of the unit to more spacious pre- fabricated quarters behind 2nd Military Hospital at Ingleburn, Sydney in 1974 led to a gradual improvement in the scope and significance of research activities at the Army Malaria Research Unit (AMRU), receiving a special boost when the number of unit staff positions was increased from 13 to 24 in 1982.3 Commencing in the mid-1980s the pace of research activities gathered momentum and greater emphasis was placed on practical problems facing Australian Defence Force (ADF) personnel deployed to malarious areas.4,5
The unit continued to operate out of Sydney until late 1996 when it was relocated to a new purpose built laboratory complex at Gallipoli Barracks, Enoggera, Brisbane and known as the Australian Army Malaria Institute (AMI).6 The establishment of the Institute enabled the ADF to play a key global role in the fight against malaria and other vector- borne diseases (VBDs). Enhanced collaboration with Australian and overseas institutions empowered AMI to make evermore significant contributions to the more effective control of VBDs. This was further facilitated by increased funding from non-Defence Health Service sources.
Commencing in 1997, AMI deployed outbreak management teams to Bougainville, and later to Timor Leste (formerly known as East Timor), in response to scores of soldiers developing malaria while on deployment to these areas.6 Without daily doxycycline prophylaxis, there is ample evidence that up to one thousand soldiers would have been incapacitated by malaria, most of them infected with potentially fatal falciparum malaria.6 Apart from causing personal distress, this would have compromised operational capability, placed severe strain on the health services and may even have jeopardised the successful outcome of the peace- keeping missions. Despite the prescribed 14-day post-exposure primaquine course, several hundred soldiers experienced their first attack of vivax malaria after returning to Australia. Furthermore, about one-fifth of them proceeded to have one to four relapses for up to a year after their initial attack. This course of events was a rather sobering reminder that malaria continued to be a serious threat to the well being and fitness of military personnel deployed to malarious areas. In addition to highlighting the importance of adhering to prescribed antimalarial measures, it emphasised the need for more effective and user friendly tools to counter the ever increasing problem of drug resistance.
AMI had earlier on pioneered the use of doxycycline for mass chemoprophylaxis and demonstrated its effectiveness during ADF deployments overseas.5 More recently it had shown that daily atovaquone/ proguanil (Malarone®) could be used as an alternative to doxycycline if required.6 Studies by AMI had also demonstrated that tafenoquine, a long-acting 8-aminoquinoline drug, might ultimately play a very useful role in malaria prophylaxis and possibly replace primaquine for prevention of vivax malaria.6 Although higher doses appeared to be more effective,6 the very short elimination half-life of primaquine and its toxicity (e.g. gastro-intestional disturbances) would always remain a problem. With the growing threat of drug resistance, significant progress was made in the non-clinical assessment of various potential antimalarial drugs, including the artemisinins, Mannich bases, and third generation antifolate compounds.
The establishment of a molecular parasitology laboratory broadened the scope of investigations in malaria diagnosis and drug resistance.6 Early results using DNA technology identified molecular markers for atovaquone resistance. These procedures also complemented various investigations with already established in vitro and in vivo procedures and enhanced AMI’s fundamental commitment to improve malaria diagnosis and to monitor the evolution and spread of drug resistance.
In the continuing quest for improved personal protection against mosquito bites, field studies included the evaluation of two novel topical mosquito repellents and a self-erecting, low profile bednet.6 The extensive survey of anopheline mosquitoes in 10 provinces of PNG, started in 1992, was completed in 2000.6 Detailed analysis of collected specimens, using DNA-based technology and monoclonal antibodies, revealed many hereto unknown facts of significant benefit to malaria control activities. One of these was groundbreaking information on the vectorial capacity of various genotypes and taxons of Anopheles farauti.
AMI became involved with other mosquito-borne diseases following its relocation to Brisbane.6 After identifying Ross River virus in mosquitoes at the Shoalwater Bay Training Area in Queensland during 1998, further observations highlighted the importance of collecting serum specimens for IgG and IgM analysis during both acute and convalescent phases of the illness. In 1999/2000, AMI identified 160 cases of dengue (mostly serotype 3) among ADF personnel in Timor Leste and virus containment was successfully managed, when nine of them were medically evacuated to Townsville. In response to the shortage and cost of Japanese encephalitis (JE) vaccine (Biken) in Australia, a series of studies was undertaken which revealed that low dose intradermal injections (one-fifth of the dose of the usual regimen) were able to provide good protection, thereby extending the life of the vaccine stockpile.
By 2000, AMI had evolved from its humble beginnings in the mid-1960s to become a world centre of excellence for malaria research.
Mission, Organisation and Staff
AMI continued its mission to ensure that ADF personnel were able to have the best possible protection against malaria and other VBDs. This mission had become more important than ever with the increased deployment of military personnel to areas overseas with a high prevalence of VBDs. Recent deployments to Bougainville, Papua New Guinea, and Timor Leste had demonstrated the importance of adequate protection against these diseases for optimum performance under adverse conditions.
During the 2000-2005 quinquennium, Professor Karl Rieckmann continued to lead AMI’s activities. In late 2002, Lieutenant Colonel Michael Edstein retired from full-time military service, and his position as Deputy Director and Commanding Officer was filled by Lieutenant Colonel Robert Cooper. Both scientists were long-standing members of AMRU/ AMI and they continued to remain actively involved in various laboratory and field activities throughout this quinquennium.
Effective control of malaria parasites, arboviruses, and their mosquito vectors relied heavily on an improved understanding of the biology and epidemiology of these organisms. For example, the ever-changing susceptibility of malaria parasites to drugs could be tackled more effectively by a better insight into the mechanisms of drug resistance and by developing better surveillance techniques. In addition to devising novel regimens and approaches to improving the effectiveness of currently available agents, AMI was actively involved in the development and/or evaluation of new antimalarial drugs, vaccines and personal protection measures. Although these investigations were generally tailored to meet the requirements of the military sector, many of them were of benefit for controlling malaria and other VBDs in civilian populations.
Objectives at AMI were primarily achieved through the activities of its five departments: Drug Resistance and Diagnostics (DRD), Drug Evaluation (DE), Clinical Studies and Surveillance (CSS), Vector Surveillance and Control (VSC), and Arbovirology (AV). Each department head had either a military or civilian appointment within the Australian Defence Organisation. Some department heads also had adjunct academic appointments with the Faculty of Health Sciences of the UnIversity of Queensland. Departmental activities were supported by an Administrative/Logistics section, a Quality Assurance section, and various committees, such as Biosafety and Animal Ethics. All human studies were reviewed by the Australian Defence Human Research Ethics Committee.
Drug Resistance and Diagnostics (DRD). Dr Qin Cheng was the Head of the department. Members of her staff included Dr Nanhua Chen, Captain Alyson Auliff, Captain Bruce Russell (up to 2002), Lieutenant Joanne Baker, and Lieutenant (Army Reserve) Michael Korsinczky.
Key functions of the department were (1) to monitor drug susceptibility of malaria parasites in the field; (2) to better understand how and why parasites develop drug resistance; (3) to determine host, parasite and environmental factors that might enhance or hinder the development and spread of drug resistance; and (4) to improve the reliability and performance of malaria diagnosis.
Responding to a call for applications by the National Institutes of Health, USA, a research proposal by Dr Qin Cheng and Prof Allan Saul (QIMR) entitled “Evolution of drug resistance in Plasmodium falciparum” was submitted and subsequently funded for three years commencing in March 2000. The project aimed to develop computer models, based on laboratory experiments and mathematical modelling, which would mimic both the growth of malaria parasites in people and the transmission of parasites within communities. The models would then be used to investigate factors underlying the development and spread of drug resistance, thereby helping to design better strategies for extending the life of existing antimalarial drugs and for protecting future drugs. Following the departure of Prof Saul a few months after initiation of the project, Dr Cheng became the Principal Investigator, assisted by Dr Michelle Gatton (mathematical modeller), Dr Beth Fowler (molecular geneticist), and Mrs Jenny Peters (molecular biologist). At the end of this first NIH grant funding period, a competitive renewal application entitled “Antigenic variation and drug resistance in falciparum” was prepared and submitted to NIH by Dr Qin Cheng (Principal Investigator) and Drs Michelle Gatton, Nanhua Chen and Dennis Kyle (Co-Investigators). Based on results obtained during the first grant, NIH provided support for a further three years (2004-2007). Dr Darren Krause joned the research efforts in 2004.
Drug Evaluation (DE). Dr Michael Edstein was the Head of the department. Members of his staff included Dr Barbara Kotecka, Dr Marina Chavchich (from 2003), Sergeant Kerryn Rowcliffe, Mr Thomas Travers, Mr Wayne Lyons, and Sergeant Hamish Barbour (from 2003). Veterinarians at the Institute’s animal facility were: Major Ivor Harris, Captain (Army Reserve) Clair Nussey (until 2001), Captain (Army Reserve) Narelle Peach (until 2003), Captain (Army Reserve) Joanne Beckett (from 2002), and Captain (Army Reserve) Amanda Perry (from 2004). Animal technicians included Mr Zbigniew Kotecki and Mrs Julie Staley (until 2003).
Key functions of the department were (1) to optimise drug regimens for malaria prophylaxis and treatment by pharmacokinetic and pharmacodynamic studies; (2) to support new antimalarial drug discovery progams; (3) to assess the antimalaria activity of promising candidate drugs using various parasitological tools and animal models; and (4) to manage the animal facility.
Dr Edstein was intimately involved with the establishment of the Vietnam Australia Defence Malaria Project (VADMP) and assumed primary responsibility for operational administration of the Australian component of the project. He also played a leading role in contributing to the successful outcome of many of the clinical and field studies in Vietnam and in organising the exchange visits by Vietnamese and Australian personnel.
Clinical Studies and Surveillance (CSS). Lieutenant Colonel Peter Nasveld continued to be closely involved in operations of several departments of the Institute, having been posted as Senior Medical Officer of the Third Brigade to the forward area of operations in Timor Leste at the beginning of this period. Major Scott Kitchener (1999-2002) carried on Lieutenant Colonel Nasveld’s work as department head from late 1999 before being replaced by Lieutenant Commander Sonya Bennett (2002- 2004). Following his departure and appointment as Lieutenant Colonel (Army Reserve), he became involved with the development of chimeric arborviral vaccines at Acambis Research (ACR) and provided a link for their subsequent clinical evaluation by AMI. Valuable support was also provided by Major (Army Reserve) Nathan Elmes (from 2003), Captain (Army Reserve) Anne Jensen (from 2001), and Captain (Army Reserve) Tracy Carthew (from 2002). Other members included Warrant Officer John Staley (until 2003), Warrant Officer Derek Davis (from 2004) and Sergeant (Army Reserve) Christine Atkins (from 2004).
Key functions of the department were (1) to conduct clinical evaluations of antimalarial drugs and vaccines against VBDs; (2) to protect ADF personnel against VBDs by monitoring their occurrence and prevalence; (3) to provide clinical advice on VBDs to ADF personnel; and (4) to maintain the ADF Central Malaria Register.
Vector Surveillance and Control (VSC). Major Stephen Frances replaced Major Robert Cooper as Head of the department in 2002 following Major Cooper’s promotion to Commanding Officer. In addition to both of these long-serving entomologists, other members of the department included Miss Cassie Jansen (until 2004), Lieutenant Robert Marlow (from 2004), Sergeant Stephen Mcleod-Robertson, Corporal Brooke Wilson (2001-2002), Corporal Raethea Huggins (2002-2005).
Key functions of the department were (1) to conduct risk assessment of exposure to VBDs by mosquito surveys; (2) to provide field commanders with the best possible assessment of risk from VBDs and optimum vector protection measures; (3) to identify potential mosquito vectors of VBDs by using molecular-based technology; (4) to determine environmental factors affecting the distribution patterns of anopheline mosquitoes; (5) to evaluate personal protection measures against VBDs used by ADF personnel under field conditions, especially topical mosquito repellents, impregnated military clothing and bednets; and (6) to evaluate the use of pyrethroid insecticides in military fabrics for protection against nuisance and vector mosquitoes.
Arbovirology (AV). Major Stephen Frances was Head of the department until 2002 when he relinquished the position to direct VSC activities. His position was assumed by Major (Army Reserve)/Professor John Aaskov, an experienced virologist at QUT, who had joined AMI in 2000. Members of his staff included Captain Mark Reid, Lieutenant Michael Reid (until 2003), Cadet Lisa Baade, Sergeant Kerry Somerscales (2002-2003), Corporal Natalie Lehmann (2003), and Corporal Andrew Baron (from 2004) and Corporal John Ross (until 2003) and Corporal Cameron Redman (from 2003) in Logistics.
Key functions of the section were (1) to provide personnel management, training and security support; (2) to manage internal and external financial affairs; (3) to prepare staff for courses, overseas visits and overseas deployments; (4) to manage the day- to-day administration of overseas visitors engaged in research activities at AMI; and (5) to order and account for equipment and supplies required by the departments and coordinate the maintenance and repair of equipment. During this period, the section maintained a considerable operational tempo of personnel movement and support for extended periods in several overseas operations.
Quality Management Section. Mr Ken Lilley was the Head of the section and was assisted by Major (Army Reserve) Robin Gregory.
Key functions of the section were (1) to ensure that laboratory equipment and procedures were maintained at the highest standard to produce data with the greatest accuracy and validity; (2) to implement and maintain accreditation and certification with national and international authorities such as National Association of Testing Authorities/Royal College of Pathologists of Australasia. (NATA/RCPA) and ISO 9001:2000; to conform to the relevant requirements of the Office of the Gene Technology Regulator (OGTR), the Australian Quarantine and Inspection Service (AQIS), and the animal use requirements of the Commmonwealth Scientific and Industrial Research Organisation (CSIRO) and Queensland Department of Primary Industries (DPI); and (3) to promote a culture of continuous improvement in the pursuit of excellence.
Walter Reed Army Institute of Research (WRAIR) Laboratory
The WRAIR laboratory was established at AMI in 2001 with the arrival of Lieutenant Colonel Dennis Kyle from WRAIR. He was part of the Engineer and Scientist Exchange Program (ESEP) between the Australia Defence Organisation and the United States Department of Defence. Just before his departure in 2004, Major Michael O’Neil replaced him for a further 3-year assignment by WRAIR to AMI. They were assisted in their investigations by Dr Marina Chavchich (from 2003), Mrs Jennifer Peters (from 2004) and Ms Karryn Grestey (from 2005).
Key functions of the laboratory were (1) to support the discovery of new antimalarial drugs; (2) to study drug resistance; and (3) to develop tools for controlling drug-resistant malaria more effectively. Most of their Key functions of the department were to improve the capacity of the ADF to detect, diagnose and prevent diseases caused by mosquito-borne viruses. During this period, Captain Reid helped accredit AMI with the Office of the Gene Technology Regulator and manage the Physical Containment Level 3 arbovirus laboratory.
Administrative/Logistic Section. Major Ivor Harris was the Head of the section except during his absence in Antarctica during 2003 when his duties were performed by Major Robin Gregory. Other members included Major (Army Reserve) Chrisopher McCormack (from 2003), Sergeant (Army Reserve) John Humphries, Corporal Anna Davis (until 2002) and Mr Kevin Anderson (from 2002) in Administration and Corporal John Ross (until 2003) and Corporal Cameron Redman (from 2003) in Logistics.
Key functions of the section were (1) to provide personnel management, training and security support; (2) to manage internal and external financial affairs; (3) to prepare staff for courses, overseas visits and overseas deployments; (4) to manage the day- to-day administration of overseas visitors engaged in research activities at AMI; and (5) to order and account for equipment and supplies required by the departments and coordinate the maintenance and repair of equipment. During this period, the section maintained a considerable operational tempo of personnel movement and support for extended periods in several overseas operations.
Quality Management Section. Mr Ken Lilley was the Head of the section and was assisted by Major (Army Reserve) Robin Gregory.
Key functions of the section were (1) to ensure that laboratory equipment and procedures were maintained at the highest standard to produce data with the greatest accuracy and validity; (2) to implement and maintain accreditation and certification with national and international authorities such as National Association of Testing Authorities/Royal College of Pathologists of Australasia. (NATA/RCPA) and ISO 9001:2000; to conform to the relevant requirements of the Office of the Gene Technology Regulator (OGTR), the Australian Quarantine and Inspection Service (AQIS), and the animal use requirements of the Commmonwealth Scientific and Industrial Research Organisation (CSIRO) and Queensland Department of Primary Industries (DPI); and (3) to promote a culture of continuous improvement in the pursuit of excellence.
Walter Reed Army Institute of Research (WRAIR) Laboratory

Figure 1: Visit to AMI by US Army Surgeon General, July 2002. (L to R): Dr Q. Cheng, Lieutenant Colonel R.D. Cooper, Lieutenant Colonel M.D. Edstein, Commander S. Bennett, Professor K. H. Rieckmann, Lieutenant General
J. B. Peake, Lieutenant Colonel D. E. Kyle, Lieutenant Colonel S. Boos, Captain M. G. Reid, Major S. P. Frances, Colonel P. Alexander.
The WRAIR laboratory was established at AMI in 2001 with the arrival of Lieutenant Colonel Dennis Kyle from WRAIR. He was part of the Engineer and Scientist Exchange Program (ESEP) between the Australia Defence Organisation and the United States Department of Defence. Just before his departure in 2004, Major Michael O’Neil replaced him for a further 3-year assignment by WRAIR to AMI. They were assisted in their investigations by Dr Marina Chavchich (from 2003), Mrs Jennifer Peters (from 2004) and Ms Karryn Grestey (from 2005).
Key functions of the laboratory were (1) to support the discovery of new antimalarial drugs; (2) to study drug resistance; and (3) to develop tools for controlling drug-resistant malaria more effectively. Most of their activities were closely integrated with work being carried out by the DRD and DE departments.
Collaboration and engagement with
military and civilian organisations
Apart from close collaboration with medical research establishments within the US Army, as evidenced by the establishment of the WRAIR Laboratory at AMI, collaboration and engagement with various military and civilian organisations, both in Australia and overseas,5,6 was maintained and expanded during this quinquennium. This was of paramount importance in achieving AMI’s objectives to improve the control of malaria and other VBDs.
Vietnam Australia Defence Malaria Project (VADMP)
Following several years of consultation, a vitally important relationship was established between the ADF and the Vietnam People’s Army (VPA) with the signing of a Memorandum of Understanding (MOU) in Hanoi in March 2000.6 This marked the start of the Vietnam Australia Defence Malaria Project (VADMP) which not only served to enhance malaria control activities within the defence forces of Vietnam and Australia but also contributed to developing overall closer defence cooperation between both countries.6 This long-term collaborative project between AMI and the VPA Military Medicine Department (MMD) had a strong and comprehensive focus on training, technological transfer, capacity building, developing effective antimalarial drug regimens and characterising malaria transmission.
The principal collaborating institutions in Vietnam were the Military Institute of Hygiene and Epidemiology (MIHE) and the Central Military Hospital 108 in Hanoi, and the Military Preventative Medical Centre and Military Hospital 175 in Ho Chi Minh City. During this quinquennium six Vietnamese officers spent 2 to 6 months at AMI. Among them was Colonel Vu Quoc Binh, Deputy Director of MIHE, and later to become the Director of MMD and the Surgeon-General of VPA, and Lieutenant Colonel Le Nogc Anh, Secretary of the Project Management Unit of VADMP in Vietnam. On 12 August 2002, the VADMP Laboratories were officially opened at MIHE, the ceremonies being attended by the Australian Ambassador to Vietnam and other dignitaries. Following the establishment of the Laboratories, successful laboratory and field studies were conducted, with some results being presented at the 14th and 15th Asia Pacific Military Medicine Conferences held in Brisbane (2004) and Hanoi (2005), respectively.
World Health Organization (WHO) Collaborating Centre for Malaria

Figure 2: Inauguration of Vietnam Australia Defence Malaria Project laboratories, Hanoi, August 2002.
Professor Rieckmann continued to serve as Director of the WHO Collaborating Centre for Malaria and, at the end of the quinquennium, completed his 32-year service as Member of the WHO Expert Advisory Panel on Malaria. Between 9-11 December, AMI hosted the “13th South-West Pacific Malaria Meeting – Roll Back Malaria in the Pacific”. This meeting brought together nine national representatives from Governments in the region, eleven Who staff members, five temporary advisers, and six observers from national and international funding organisations to discuss many different aspects of malaria control in the region. AMI was also visited by several WHO staff during 2000-2005, including several visits by Dr David Bell and Dr Jeffrey Hii.
Throughout this period, many AMI staff members continued to contribute to, and benefit from, participation in WHO activities. Dr Qin Cheng served as Temporary Adviser at WHO Workshops/ Consultations in Shanghai and Manila, and was the recipient of two WHO grants relating to rapid diagnostic tests (RDTs) for malaria. She was also a collaborating partner on a WHO funded project to eliminate malaria from the Hainan Province in China. Ms Joanne Baker participated in WHO- sponsored field and laboratory evaluations of RDTs in the Philippines. Dr Robert Cooper, in collaboration with Professor Gao Qi (JIPD) and Dr Nigel Beebe (UTS), received a WHO grant to study the potential malaria vectors of the Hyrcanus group of mosquitoes in central and southern China. Mr Ken Lilley acted as Rapporteur at a WHO Multiregional Workshop on “Quality Assurance of Malaria Light Microscopy” held in Malaysia, in addition to conducting WHO- sponsored malaria microscopy courses in the Philippines, Cambodia, Indonesia and the Solomon Islands. The purpose of these courses was to assesss the proficiency of provincial microscopists, to identify qualified personnel as national trainers, and to review draft quality assurance (QA) programs and procedures for malaria microscopy and RDTs at country peripheral levels.
Wide network of partnerships
Interaction with other experts at national and international meetings continued to enhance AMIs ability to achieve its objectives. For example, following the outbreak of vivax malaria in ADF personnel returning to Australia, AMI co-sponsored the first- ever international conference on vivax malaria research organised by the US-based Multilateral Initiative on Malaria (MIM). This 2002 conference in Bangkok provided AMI staff with the opportunity to interact with others who were also concerned with the prevention of vivax malaria after leaving endemic areas. The second international conference – “Vivax Malaria Research: 2005 and beyond” was held in Washington DC, USA, with Dr Cheng being a member of the organising committee.
All departments were involved in continuing and expanding their collaboration with other institutions. These institutions included:
- AFRIMS – Armed Forces Research Institute of Medical Sciences, Bangkok,
- AP – Aventis Pasteur, France
- ACR – Acambis Research, UK
- BAY – Bayer AG, Germany
- CDC – Center for Disease Control, USA
- GMI – Gorgas Memorial Institute of Health Studies, Panama
- JPC – Jacobus Pharmaceutical Company, USA
- JIPD – Jiangsu Institute of Parasitic Diseases,China
- MAH – Mahidol University, Thailand
- MERLIN – Medical Emergency Relief International, UK
- MMV – Medicines for Malaria Venture, Switzerland
- MSHR – Menzies School of Health Research, Australia
- NAMRU-2 – ) US Naval Medical Research Unit 2, Indonesia
- NIH – Laboratory of Parasitic Diseases, National Institutes of Health, USA
- NIHRD – National Institute of Health Research and Development, Indonesia
- QH – Queensland State Health, Tropical Public Health Program, Australia
- QIMR – Queensland Institute of Medical Research, Australia
- QUT – Queensland University of Technology
- PNGIMR – Papua New Guinea Institute of Medical Research, PNG
- RITM – Research Institute of Tropical Medicine, Philippines
- SMRU – Shoklo Malaria Research Unit, Thailand
- UQ – University of Queensland, Department of Parasitology, Australia
- UTS – University of Technology Sydney, Australia
- VBDCU – Vanuatu Malaria and Other Vector Borne Diseases Control Unit, Vanuatu
- VADMP – Vietnam Australia Defence Malaria Project, Vietnam
- WEHI – Walter and Eliza Hall Institute, Australia
- WHO – World Health Organization, Switzerland
- WHO/WPRO – World Health Organization, Western Pacific Regional Office, Philippines
- WRAIR – Walter Reed Army Institute of Research, Experimental Therapeutics Division, USA
- WRL – Wellcome Research Laboratories, Thailand
Activities
Many of the objectives at AMI were achieved by joint efforts between two or more departments. Because of this, outcomes and achievements of each department are not presented under department headings. Rather, they are presented according to key objectives pursued by AMI during this quinquennium.
1. MALARIA PREVALENCE AND SURVEILLANCE
Regular six-monthly updates on the malaria situation in the ADF were issued during this quinquennium.7-9 They were based primarily on the analysis of data provided by health personnel to the ADF Central Malaria Register maintained at AMI.10 Malaria notifications in the ADF declined from almost 400 cases in 2000 to 75 in 2001, and then to fewer than 20 per year over the next four years.11 As described previously,6 most of the malaria cases in 2000 were observed in soldiers who experienced their first acute attack of malaria in Australia because doxycycline had effectively suppressed their vivax infections while they were on peacekeeping duties in Timor Leste. However, because more than 60 soldiers developed malaria (two-thirds of them falciparum malaria) soon after arrival in the forward area of operations,12 an AMI disease outbreak investigation and management team was deployed to Timor Leste at the beginning of 2000.13
Major risk factors were poor compliance with doxycycline prophylaxis, involvement in night operations, lack of preventive medicine support and higher risk locations selected by platoons. Following initial field assessments, the malaria outbreak was brought under control by instituting various epidemiological surveillance and operational activities (in collaboration with preventive medicine personnel) and fostering improved compliance with personal protection and chemoprophylactic measures.13-15 In addition, new tools were assessed for improved prevention and control of malaria (see below). The marked reduction in the number of malaria cases was achieved despite a significant level of malaria transmission in the local villages.16 Apart from being infected with P. falciparum and P. vivax, a few villagers were infected with P. malariae, possibly the first report of the presence of this Plasmodial species on the island of Timor Leste.17
2. PROPHYLAXIS AND TREATMENT OF BLOOD STAGE MALARIA PARASITES
AMI continued its investigations to identify better tools for countering the threat posed by drug-resistant malaria. More than a decade ago AMI had pioneered the daily use of doxycycline for military contingents deployed to malarious areas. This tetracycline antibiotic continued to be effective against the blood stages of drug-resistant parasites and was the first- line drug for protecting ADF personnel against malaria while they were overseas. Atovaquone/proguanil (Malarone®), a drug combination which had been investigated intensively at AMI for many years, had recently been approved for daily use by soldiers who were unable to take doxycycline. However, under certain field conditions, better drug compliance might be achieved by using ADF’s second-line drug, mefloquine, which had to be taken only once a week. Although mefloquine was being used widely overseas as a first-line drug for malaria prophylaxis, further information regarding mefloquine’s tolerability, safety and pharmacokinetics seemed desirable.
Most drugs used for prophylaxis were also being used to treat drug-resistant malaria infections. But, increasingly, they were being used in combination with artemisinin drugs, a group of semi-synthetic compounds derived from Artemisia annua. Apart from an extremely rapid clinical response to treatment, artemisinin-based combination therapy (ACT) was far more effective than mono-drug therapy in curing falciparum infections and reduced the likelihood of the emergence of drug-resistant parasites. During the previous decade, AMI had developed in vitro tests and bioassays to assist in the pharmacokinetic evaluation of various artemisinin and antifolate compounds.5,6 Investigations were now broadened to determine the pharmacokinetics of atovaquone/ proguanil, mefloquine and other compounds used in ACTs. Furthermore, studies were carried out to assess the effects that pregnancy, gender or food might have on the absorption and/or disposition of these drugs, because they might ultimately affect their bioavailability and effectiveness. In view of the increasing role of artemisinin drugs in the treatment of drug-resistant malaria, further studies were carried out with artemisone, a potent new drug with little or no neuro- or cyto-toxicity.
Atovaquone/proguanil (Malarone®) pharmacokinetics during pregnancy
Atovaquone/proguanil/artesunate was a well tolerated and highly effective ACT that was being investigated for the treatment of falciparum malaria. Earlier studies in collaboration with WRL had shown that the pharmacokinetics of individual components of this ACT were not altered when given in combination with one another.6 As few antimalarial drugs could be recommended during pregnancy, the SMRU on the western border of Thailand approached AMI in 2001 to assess the pharmacokinetics of the proguanil and atovaquone components of this ACT during pregnancy. This was especially important in view of the well known heightened vulnerability of pregnant women to malaria infections, higher risk of developing severe malaria, and the fact that no information was available on the extent to which the extensive physiological changes during pregnancy might affect the pharmacokinetics of this drug combination.
The first study, carried out in healthy Karen women during the second and third trimesters of pregnancy, showed that plasma concentrations of cycloguanil, the active triazine metabolite of proguanil, were reduced by approximately 50% when proguanil was administered alone.18 This suggested that late pregnancy was associated with reduced biotransformation of proguanil. Although pregnancy did not affect the rate of proguanil absorption, it did increase plasma clearance and apparent volume of distribution of the drug, suggesting that pregnant women might need to receive a higher dose of proguanil. In the second study, serial plasma concentrations of atovaquone, proguanil and cycloguanil were measured in 24 malaria infected pregnant Karen women after completing a 3-day treatment regimen consisting of atovaquone (20 mg/ kg/day), proguanil (8 mg/kg/day) and artesunate (4 mg/kg/day).19 This ACT was well tolerated with no adverse effects in the pregnant women, birth outcomes, and other clinical and laboratory parameters. Compared with previously reported blood maximum drug concentrations (Cmax) and area under the drug concentration versus time curve (AUC) values of atovaquone, proguanil and cycloguanil in healthy women from the same population group, pregnancy caused a 50% reduction in the Cmax and AUC values, suggesting that the dose of atovaquone- proguanil might need to be increased for malaria treatment during pregnancy.
Prolonged persistence of atovaquone after administration of atovaquone/proguanil (Malarone®)
Further information on the pharmacokinetics of atovaquone was obtained by determining plasma atovaquone concentrations collected from three Caucasian volunteers after they had been treated for three days with atovaquone/proguanil during malaria investigations at QIMR.20 The average elimination half-life of atovaquone in the volunteers was much longer than expected at 5.9 days by high performance liquid chromatographic (HPLC) analysis and 4.9 days by bioassay, and atovaquone was still present 35 days after treatment. These half-lives were about twice as long as those obtained previously in African and Asian patients treated with atovaquone. Since proguanil has a half-life of less than one day, proguanil would not be present to potentiate the antimalarial activity of atovaquone for about a month after treatment. Although the prolonged persistence of atovaquone would be of little consequence when used by short-term travellers, it could lead to the rapid selection of atovaquone-resistant parasites if used widely by residents living in endemic areas.
Effectiveness, tolerability and pharmacokinetics of mefloquine for malaria prophylaxis in Timor Leste

Figure 3: Captain B. Russell and Major S. Kitchener taking off from Komoro airfield in Timor Leste to carry out field investigations.
Poor compliance by some soldiers with daily doxycycline prophylaxis led to an appraisal of the wider use of mefloquine for ADF personnel because it had to be taken only once a week.21,22 Although mefloquine prophylaxis had been well tolerated by British, Dutch, Indonesian, Italian and US soldiers during two to five month deployments to malarious areas, parasite resistance to mefloquine had been encountered in Cambodia and Indonesia. Furthermore, there were isolated reports of severe neuropsychiatric side-effects associated with the use of mefloquine. Following a field study in Timor Leste during which no severe adverse events were observed in the 162 Australian soldiers receiving mefloquine for six months,23 a large field study was undertaken in Timor Leste to determine whether a loading dose of mefloquine would (1) help to identify individuals who might not tolerate the drug, and (2) allow “steady-state” blood mefloquine concentrations to be reached right at the start rather than several weeks after commencing weekly medication.
In two successive contingents, 1,155 male soldiers received a loading dose of one 250 mg tablet of mefloquine every other day on three occasions, followed by one tablet a week for six months.24 Seventy-five soldiers (6.5%) experienced adverse responses to the drug and completed their deployments on doxycycline prophylaxis. The three soldiers who experienced serious adverse events of a neuropsychiatric nature, all revealed prior episodes of either depression, hallucinations or epilepsy. All soldiers were protected against malaria while in Timor Leste and 94% of them indicated that they would use mefloquine again. Clinical assessment after the loading dose was found to be both positively and negatively predictive of side effects associated with mefloquine, simplifying its use for malaria chemoprophylaxis. Pharmacokinetic studies also provided much useful information relating to the use of this drug under operational conditions.25 After determining plasma mefloquine concentrations by HPLC at various times during prophylaxis, the pharmacokinetics of mefloquine could best be described as a two-compartment model: low plasma clearance (CL/F, 2.1 L/h) and a high central volume of distribution (V1/F, 528 L), with an elimination half-life of 14.0 days. Body weight had a positive influence on central volume but was insufficient to warrant adjustments to the drug regimen.
Clinical studies in Vietnam on the influence of food on mefloquine and piperaquine pharmacokinetics
Food had been reported to increase the bioavailability of mefloquine in healthy Caucasian volunteers, but it was unclear whether this was also the case in malaria patients. As part of a VADMP project, the pharmacokinetics of mefloquine was determined in Vietnamese malaria patients treated with mefloquine in the fasting and fed state.26 Blood mefloquine concentrations were compared in two cohorts of six malaria patients treated with mefloquine (15 mg/kg) and artesunate (8 mg/kg) and given either a low-fat (approximately 3 g fat) or high-fat (approximately
30 g fat) meal. The results showed no statistical differences (P<0.05) in the Cmax and AUC of mefloquine between these two groups of patients. These findings suggested that a high-fatty meal does not increase the bioavailability of mefloquine in malaria patients and should therefore not affect their response to treatment. This was not the case for piperaquine, another drug being considered as a partner with dihydroartemisinin for ACT in Vietnam and other countries of Southeast Asia. When 26 healthy Vietnamese soldiers were administered 0.5 or 1.0 g of piperaquine, the bioavailability of the drug was increased by 41% after eating a moderately fatty meal (about 17 g of fat).27
Artemisone – a new artemisinin compound for clinical evaluation
Artemisinin derivatives had by now been acknowledged to be the most rapidly acting drugs for the treatment of falciparum infections. However, infections were not being cured by 3-day courses of treatment due to the short pharmacological elimination half-lives of the artemisinins. Since patient compliance with longer courses of treatment was poor, especially in malarious areas with limited health facilities, various slower-acting but longer-lasting drugs (see above) were being investigated for use as partner drugs for ACT. Recently artemisone, a new semi-synthetic drug, had been developed which was relatively cheap to synthesise, and, unlike some other artemisinins, displayed negligible neuro- and cytotoxicity. Early ex vivo investigations with artemisone at AMI had also indicated that the degree and duration of its activity against multidrug-resistant P. falciparum was significantly greater than that of artesunate following drug administration to non-infected Saimiri sciureus monkeys.6
This was followed up by further studies at AMI with Aotus monkeys infected with the chloroquine- resistant FVO strain of P. falciparum. Since many patients were not cured of their malaria infections because they failed to complete 3-day courses of treatment, might just a single dose of artemisone, combined with subcurative single doses of mefloquine, be sufficient to cure infected Aotus monkeys? In a pilot study, three monkeys cleared parasites within one day and two monkeys receiving only 10 mg/kg artemisone and 5 mg/kg mefloquine were cured.28 This was far below the curative mefloquine dose of 20 mg/kg for Aotus monkeys. The remaining monkey that received 2.5 mg/kg mefloquine had a recrudescence of parasitaemia 24 days after treatment. The findings suggested that this ACT might eventually prove useful in areas with low malaria transmission but, because of mefloquine’s very long persistence in the body, the likelihood of developing resistance to mefloquine would be increased in areas with high levels of malaria transmission.
Additional investigations were carried out in collaboration with GMI in Panama, using a larger group (23 Aotus monkeys) than was available at AMI.29 Artemisone was administered in combination with two other partner drugs – amodiaquine and clindamycin. Although amodiaquine is a 4-aminoquinoline drug, parasites were often less resistant to this inexpensive drug than to chloroquine.30 Clindamycin, an antibiotic, was another drug which had been used in combination with artemisone for treating malaria patients. Whereas monkeys failed to be cured after one day of treatment with amodiaquine (20 mg/kg) and artemisone (30 mg/kg), they were cured after three days treatment with amodiaquine (20 mg/kg/day) and artemisone (10 mg/kg/day). A 3-day course of clindamycin (100 mg/kg/day) and artemisone (30 mg/kg/day) was also effective in curing falciparum infections.
In view of the encouraging results obtained in studies with non-human primates, Phase I human safety and tolerability studies with artemisone were initiated in healthy German volunteers.31 With the support of MMV and BAY, AMI assisted by assessing the pharmacokinetic properties and ex vivo pharmacodynamic antimalarial activity of artemisone and its metabolites. Artemisone was well tolerated, with no serious adverse events and no clinically relevant changes in laboratory and vital parameters, during and following administration of single or multiple ascending doses (10-80 mg range) of artemisone to 56 healthy volunteers. The pharmacokinetics of artemisone demonstrated dose linearity, with a Cmax of 140 ng/mL, an elimination half-life of 2.8 hours, a high oral clearance of 284 L/h, and a large apparent volume of distribution of 14.5 L/kg following a single 80-mg dose. Plasma samples taken after multiple dosing showed marked ex vivo pharmacodynamic antimalarial activities against two multidrug-resistant P. falciparum lines and confirmed the presence of active metabolites. Compared to other artemisinin derivatives, such as artesunate and dihydroartemisinin, artemisone’s longer elimination half-life (2.8 hours versus 1.0 hour for dihydroartemisinin) appeared to favour this artemisinin as a candidate ACT drug for treatment of falciparum malaria. As a result of these findings, further clinical studies with artemisone were planned, including Phase II efficacy studies in Thailand.
3. PROPHYLAXIS AND TREATMENT OF LIVER HYPNOZOITES OF VIVAX MALARIA
The outbreak of vivax malaria among several hundred soldiers after returning to Australia during 2000 re-emphasised the need for improved measures to prevent exposure to infected mosquitoes. But it also highlighted the urgent need for antimalarial drug regimens that would reduce the risk of this happening in the future. The fact that most of these soldiers experienced their first attack of malaria more than a month after leaving an endemic area indicated that inadequate drug suppression of blood stage parasites was not the problem. Rather, the outbreak of vivax malaria was due to the activation of dormant hypnozoites in the liver at different time intervals up to a year or more after leaving Timor Leste.
Since it was unclear what determined the number and timing of relapses, AMI attempted to investigate to what extent molecular diversity of parasites might influence the relapse patterns experienced by soldiers after their return to Australia.32 Although high molecular diversity was observed, primary infections and relapses were produced by the activation of a single hypnozoite clone in 99% of cases. Even in patients with more than two genetically different hypnozoites, 71% of them still experienced clonal relapses. The activation of a single hypnozoite genotype, when multiple genotypes were present in the liver, suggested that hypnozoites were activated according to a genetically determined biological clock and not triggerrd by non-specific environmental or host factors. The findings also suggested that multiple liver hypnozoite genotypes were associated with multiple replases. Therefore, any measures to reduce exposure to mosquitoes would reduce not only the number of malaria infections but also the number of relapses.
While providing assistance with the diagnosis and management of these infections in Timor Leste, it became obvious that, in attempting to deal with the situation, soldiers were receiving a variety of different treatment regimens.33,34 Although regimens with higher primaquine doses were more effective in preventing P. vivax relapses,6 the lengthy duration of medication did not encourage drug compliance. More user friendly drug regimens would undoubtedly be more effective in eradicating the dormant hypnozoites remaining in the liver after leaving an endemic area. With this in mind, clinical studies were initiated to evaluate the efficacy and safety of shorter courses of primaquine and tafenoquine taken either during or after deployment overseas.
Shorter primaquine prophylactic and treatment regimens
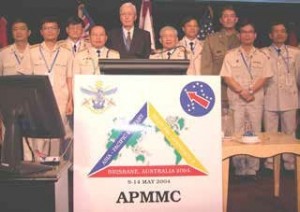
Figure 4: Key contributors to the Vietnam Australia Defence Malaria Project attending the 14th Asia Pacific Military Medicine Conference, Brisbane, May 2004. Front row (L to R): Senior Colonel Nguyen Xuan Thanh, Lieutenant General Cuong Tien Chu, Professor Karl Rieckmann, Professor Bui Dai, Lieutenant Colonel Michael Edstein, Senior Colonel Vu Quoc Binh.
The very large number of vivax infections observed in soldiers after their return to Australia from Timor Leste6 emphasised the urgent need for better post- exposure drug regimens to eradicate the residual dormant hypnozoites of P. vivax malaria. Earlier studies in ADF personnel returning from Timor Leste had indicated that primaquine 30 mg (15 mg twice a day) was more effective than 22.5 mg daily for 14 days in curing these infections.6 As the lengthy 14-day regimens were contributing to poor compliance, a pilot volunteer study was initiated to assess the tolerability of higher dose, shorter courses of primaquine.35 Australian soldiers tolerated primaquine 22.5 mg twice a day for 10 days and 30 mg twice a day for seven days just as well as 15 mg twice a day for 14 days. The findings indicated that additional studies were desirable to further define the tolerability, safety and effectiveness of shorter, high dose courses of primaquine.
Poor compliance was also a problem in patients who were being treated with 14-day courses of chloroquine/primaquine after developing malaria. This drug regimen had the additional handicap that chloroquine-resistant P. vivax, first identified at AMI,4 was being reported from many areas of Asia, Oceania and South America. By contrast, P. vivax malaria continued to be susceptible to the artemisinins. Might a shorter treatment course of artesunate (200 mg twice a day for two days) followed by primaquine (22.5 mg base twice a day for seven days) be the answer?
Under the auspices of VADMP, this drug regimen was administered to 28 adult patients infected with P. vivax in Vietnam.36 All patients responded quickly to treatment with mean parasite and fever clearance times of 14.2 hours and 18.6 hours, respectively. The high daily dose of primaquine was generally well tolerated, and only one patient (3.6%) had a recurrence of parasitaemia during the 28 day follow-up period. As most patients infected with Southeast Asian strains of P. vivax have their first relapse within 28 days after treatment with a rapidly eliminated blood schizonticide, such as quinine or artesunate, the failure to do so by 96% of the patients suggested that this drug regimen was active against both blood and liver stages of vivax malaria. These findings indicated the need for further studies to confirm that rapidly acting and short artesunate- primaquine regimens are able to provide better patient compliance and treatment outcomes than standard chloroquine-primaquine regimens.
Influence of gender and food on primaquine pharmacokinetics
Although primaquine had been used for 50 years for the radical cure of P. vivax dormant (hypnozoite) stages, little information was available on the effect of gender and food on the disposition of primaquine. Earlier studies appeared to indicate that female ADF personnel had a higher prevalence of gastro-intestinal (GI) disturbances than their male counterparts during post-exposure prophylaxis with primaquine.37 This could have been due to higher blood primaquine concentrations in females than in males. Under the auspices of VADMP, a randomised, two-phase cross-over study was conducted in which 10 healthy male and 10 healthy female Vietnamese soldiers were administered a single oral dose of 30 mg primaquine in the fasting and fed states.38 The pharmacokinetics of primaquine was comparable in both groups, with geometric mean ratios of Cmax = 0.89 and AUC = 0.80, although males had a slightly higher plasma clearance than females. When primaquine was taken in conjunction with a fatty meal, the geometric mean Cmax of primaquine increased by 26% and the AUC by 14%. When the same dose of primaquine was given to nine healthy male and nine female ADF personnel, no significant differences in the pharmacokinetics of primaquine between the genders were observed.39 These findings suggested that, based on single dose assessment of primaquine, there was no need to modify primaquine doses for women. However, the greater bioavailability of primaquine when consumed with a fatty meal might lead to improved antimalarial effectiveness irrespective of gender.
Tafenoquine for the prevention and cure of vivax malaria
Ground breaking investigations at AMI had shown that tafenoquine might be more effective than primaquine in the prevention and cure of vivax malaria.5,6 This new, long-acting synthetic analogue of primaquine might not only improve patient compliance with post-exposure prophylaxis and treatment regimens, but might provide protection against vivax and falciparum malaria if taken on a weekly basis. Because of the potential importance of this 8-aminoquinoline drug in reducing the malaria burden in ADF personnel, considerable time and effort was devoted to carrying out further clinical studies with this drug in Australian soldiers contributing to peacekeeping duties. In addition to pharmacokinetic studies involving male and female ADF personnel, several hundred soldiers deployed to Timor Leste participated in the first Phase III trial to determine the safety, tolerability and effectiveness of tafenoquine for malaria prophylaxis.
Tafenoquine post-exposure prophylaxis at end of deployment to malarious area
A previous short report had already described preliminary findings from a study in which 173 Australian soldiers had received a 3-day course of tafenoquine as post-exposure prophylaxis at the end of their peacekeeping duties in Bougainville, PNG.6,37 Since GI disturbances are a well known feature associated with the use of 8-aminoquinolines, 87 volunteers (76 males; 11 females) received a single tafenoquine dose (400 mg once a day) and 86 voluneers (73 males; 13 females) received a split tafenoquine dose (200 mg twice a day) to determine whether the split dose would lower the incidence of side-effects. Although GI disturbances were generally mild, self-limiting and not significantly different between the two groups, the frequency of nausea and abdominal distress in both groups was more than two-fold higher in females than in males. Furthermore, plasma tafenoquine concentrations were significantly higher in females than in males (mean values: 737 ± 118 ng/mL vs. 581 ± 113 ng/mL) with similar body weight.40 Whilst little difference was observed in the way both sexes tolerated single and split doses, the findings did suggest that there might be an association between tafenoquine concentrations and GI disturbances and that adjustments might have to be made in the dose of tafenoquine administered to women.
Tafenoquine treatment of Plasmodium vivax malaria
Relapses of vivax malaria were common among ADF personnel after their return to Australia, despite post- exposure prophylaxis and/or treatment with 14-day courses of primaquine. Following the successful treatment of two patients with 3-day courses of tafenoquine,41 a further 27 patients were treated with tafenoquine after their vivax infections had failed to be cured by chloroquine and primaquine.42 After a standard course of chloroquine (1,500 mg base over three days), they received a loading dose of tafenoquine (200 mg/day for three days) followed by 200 mg a week for eight weeks. Only one of the patients experienced a relapse during the next six months. Although further optimum dose-finding studies are indicated, these findings suggested that intermittent weekly dosing with tafenoquine over several weeks might prove more effective than daily dosing over a shorter period of time. The advantages of such a tafenoquine regimen might be similar to those observed following weekly doses of primaquine administered over a period of eight weeks.43
Tafenoquine prophylaxis during deployment to malarious areas
By 2000, doxycycline, Malarone® and mefloquine were being used to protect ADF personnel against malaria during their deployments overseas, but they all had shortcomings, including their inability to prevent relapses and to radically cure P. vivax infections. Although post-exposure prophylaxis with tafenoquine might prove to be more effective than using primaquine, could such prophylaxis be dispensed with altogether by taking tafenoquine throughout the time spent overseas? During a previous collaborative field study in Thailand, the administration of tafenoquine (400 mg) at monthly intervals for five months had been shown to be highly effective in preventing vivax and falciparum infections.6 Based on various considerations, including tafenoquine analysis of Thai blood samples at AMI, it was decided to conduct the first Phase III trial on the safety, tolerability and effectiveness of tafenoquine in Australian soldiers, with reduced doses of the drug being administered at shorter time intervals. So in October 2000, a randomised double-blinded study was started which involved the participation of 654 soldiers during the entire period of their peacekeeping deployment to Timor Leste. 44,45
During the six month period, 492 soldiers received a loading dose of 200 mg tafenoquine daily for three days followed by a weekly dose of 200 mg tafenoquine. A comparator group of 162 soldiers received a weekly dose of 250 mg mefloquine. As the soldiers had acquired no prior immunity to malaria, ethical considerations obviously precluded incorporation of a concurrent no-drug placebo group. After their return to Australia, the mefloquine recipients were administered primaquine (15 mg twice a day) for 14 days whereas the tafenoquine recipients were given a placebo. While they were in Timor Leste, none of the 654 volunteers developed malaria, but four tafenoquine recipients (0.9%) and one mefloquine recipient (0.7%) had acute attacks of P. vivax malaria within 16 to 20 weeks after returning home. This was in marked contrast to the 168 malaria cases observed in the 1,351 soldiers of two battalions that were deployed to the same area during the previous wet season between October 1999 and February 2000.6 Although the exposure of soldiers to malaria could not be estimated directly without a placebo control, malaria transmission continued to occur in several villages in close proximity to where the soldiers were located.16
Drug-related adverse events were generally mild or moderate in severity and comparable in the two groups. The most common drug related events were GI disturbances, with eight (<2%) of the tafenoquine recipients reporting that the drug did not allow them to complete their daily duties. Only three soldiers in the tafenoquine group discontinued prophylaxis because of possible drug related adverse events (none in the mefloquine group). Mild vortex keratopathy, detected in 93% of a subset of 74 volunteers, was not associated with any visual disturbances and had fully resolved within one year after stopping medication.45
The population pharmacokinetics of tafenoquine was determined in 476 male and 14 female participants in this study by analysing plasma tafenoquine concentrations in blood samples collected after the last loading dose and then at weeks 4, 8, and 16.46 Analysis of specimens revealed that tafenoquine had a relatively low plasma clearance (CL/F) of 4.5 L/h, a high apparent volume of distribution (V/F) of 1,896 L, suggesting that the drug was widely distributed to body tissues and organs. As expected, the elimination half-life of tafenoquine was long at 12.7 days. Pharmacokinetic data from the four soldiers who developed vivax malaria after returning to Australia were similar to those who remained free of malaria. Neither could any links be established between pharmacokinetic parameters and the prevalence or severity of GI disturbances or other adverse events, suggesting that plasma tafenoquine concentrations were not the primary predictor of tafenoquine tolerability. These findings indicated that (1) the derived population one-compartment pharmacokinetic model for tafenoquine satisfactorily described the disposition and variability of tafenoquine in ADF personnel, and (2) the pharmacokinetic properties of the drug were well suited for long-term weekly malaria prophylaxis during military deployments.
This study involving ADF personnel was the first and only Phase III study to show that weekly tafenoquine taken for six months was an effective prophylactic drug against both P. falciparum and P. vivax malaria in non-immune individuals.
4. MALARIA DIAGNOSIS
Rapid diagnostic tests (RDTs)
Early diagnosis and treatment are critical to prevent severe complications and death from malaria, particularly in individuals with little or no prior exposure to malaria. Although definitive diagnosis of malaria can only be established by microscopic examination of blood films, the availability of a non-microscopic test would be a distinct advantage during the deployment of ADF personnel to remote malarious areas where reliable malaria microscopy might not be available.
In the mid-1990s, AMI had participated in the field evaluation of the ICT Malaria Pf test card which was the first immunochromatographic test card to detect a specific antigen (PfHRP2) produced in patients infected with falciparum malaria.5 By 2004, about 25 branded malaria rapid diagnostic tests (RDTs) were commercially available; some of them detected P. falciparum only, while others detected P. falciparum plus one or more other plasmodial species. However, the performance of these products (sensitivity, specificity, heat durability, ease of use, etc) were reported to vary greatly between different products and between the same products used in different settings.
In view of the variability observed in the performance of these tests, WHO/WPRO organised an informal consultation on laboratory methods for the quality assurance of malaria RDTs. Following this meeting, to which Dr Qin Cheng had been invited, DRD became a key laboratory in the WHO malaria RDT Quality Assurance network, making significant contributions (described below) to the development of positive controls and the testing of various products and lots. As a WHO Collaborating Centre for Malaria, AMI also collaborated with QIMR in examining several important parasite and host factors that could affect the performance of RDTs.
Since many RDTs were based on the detection of P. falciparum histidine rich protein 2 (PfHRP2), might variability in RDT results be related to genetic diversity of PfHRP2 antigen? After amplifying and sequencing the pfhrp2 gene from 75 P. falciparum lines and isolates originating from 19 countries, extensive diversity in this antigen was observed both within and between countries. When a subset of parasite isolates was tested in two popular brands of RDTs, a correlation was observed between detection sensitivity and antigen structure. The results demonstrated for the first time that the variability of PfHRP2 could affect the detection sensitivity at parasite densities ≤250/µL blood.47 Significant differences were also observed between the reactivity of four PfHRP2 specific mononclonal antibodies to parasite PfHRP2 from a single isolate and also when one of the antibodies was tested against different isolates. When the target epitopes of these antibodies were determined they were found to vary in frequency in different isolates.48 These findings appeared to indicate that variability in PfHRP2 antigen might have an effect on the sensitivity of PfHRP2-detecting RDTs. However, further investigations including isolates from Africa and South America suggested that RDTs were not greatly affected by the diversity of PfHRP2 at parasite densities exceeding 200 parasites/µL blood.49
Some of the RDTs were based on the detection of aldolase, a key enzyme in the glycolysis pathway of malaria parasites. Since RDTs targeting aldolase were showing highly variable sensitivities, the genetic diversity of parasite isolates originating from geographically different areas were determined by sequencing the coding genes.50 The results showed that aldolases were highly conserved, indicating that antigenic diversity was not a cause of variable RDT sensitivity. However, in general, aldolase- detecting RDTs were less sensitive than their HRP2 counterparts.
In their excellent article in ADF Health, Baker et al.51 reviewed the results of investigations carried out with RDTs at AMI and elsewhere, and pointed out their advantages and limitations. Although RDTs offered distinct advantages for early diagnosis and treatment, especially when expert malaria microscopy was not available, ADF medical personnel needed to be aware that a patient might still have malaria despite a negative RDT result. This would be more likely during the early stages of a malaria infection when parasite densities were still at a low level. For this reason, competent malaria microcopy remained the preferred method of arriving at a definitive species diagnosis of malaria. Patients with persisting symptoms of malaria should have repeated RDTs within 24 hours of the initial test, and microscopy should be performed if at all possible.
Polymerase chain reaction (PCR) test
Earlier efforts to employ sensitive and specific PCR- based methods for malaria detection6 were followed up by the establishment of nested PCR and a multiplex PCR to detect or verify Plasmodial species in ADF personnel suspected of having malaria but in whom negative or discrepant results were obtained by microscopy or RDT. This could now be performed using whole blood samples, plasma samples, dried blood on filter papers and blood smears. In combination with results obtained with microscopy or RDT, it ensured that accurate malaria information was entered into the ADF Central Malaria Register.
5. ASSESSMENT OF DRUG RESISTANCE
Malaria control activities in the Asia-Pacific region continued to be frustrated by the changing susceptibility of parasites to standard antimalarial drugs. This also affected ADF operational and peacekeeping activities. Many countries were using chloroquine (CQ) and sulfadoxine-pyrimethamine (SP) for first- and second-line treatments of uncomplicated malaria. CQ continued to be used because it was readily available and relieved symptoms in patients who were infected with vivax malaria or had become partially immune to falciparum malaria. When too many falciparum infections failed to be cured, SP was usually introduced for malaria treatment. Whereas both components of SP act synergistically against P. falciparum, this is not the case for P. vivax because of its innate resistance to the sulfadoxine component. In the presence of low to moderate degrees of pyrimethamine resistance, this meant that, unlike its activity against P. falciparum, SP was often ineffective against P. vivax malaria.52 Since P. falciparum could not be distinguished from P. vivax in many malarious areas due to unavailable or unreliable malaria microscopy, CQ was often co-administered with SP to increase the patient’s likelihood of responding adequately to treatment irrespective of the infecting Plasmodial species. The response to treatment was of course far less satisfactory in areas with CQ-resistant vivax malaria.
Susceptibility of Plasmodium falciparum to sulfadoxine/ pyrimethamine (SP) in Timor Leste
When ADF personnel were deployed on peacekeeping duties to Timor Leste in 1999 the efficacy of CQ and SP for the treatment of uncomplicated P. falciparum malaria was unknown. AMI was approached by the non-government organisation, MERLIN, to assist in determining the efficacy of the antimalarial drugs by genotyping for drug resistance and measuring blood drug concentrations. Earlier investigations at AMI had already shown the value of molecular markers for monitoring the resistance of P. falciparum to CQ and atovaquone.6 Collaborative investigations with WEHI and PNGIMR had also indicated that the 76T allele of the pfcrt gene was strongly associated with chloroquine resistance.53 After documenting a high level of CQ resistance in 48 patients,6 a further 40 individuals infected with falciparum malaria were treated with SP following the collection of their blood to determine whether genetic mutations could be detected in the dihydrofolate reductase (DHFR) of their parasites. Although 90% of these partially- immune patients were cured, 80% of them were infected with parasites which carried double genetic mutations (S108N/C59R) in SP’s target molecule (Pfdhfr).54 This suggested that the useful life of SP might be limited and that alternative drugs were required to treat patients with lower levels of acquired immunity to malaria.
Susceptibility of Plasmodium falciparum and Plasmodium vivax to chloroquine (CQ) and sulfadoxine- pyrimethamine (SP) in Indonesia
Malaria epidemics in Central Java had increased concern about the re-emergence of endemic malaria which could threaten the island’s 120 million residents. AMI was approached by NAMRU-2 to collaborate in a 28 day in vivo test of the efficacy of CQ and SP among 167 villagers from Central Java with 33% of 1,389 residents being infected prior to enrollment.55 Drug analysis was done at AMI to ensure that the patients had adequate blood concentrations of CQ and SP after starting treatment. The study revealed CQ and SP to be ineffective therapy for P. falciparum, with therapeutic failure rates of 47% and 22%, respectively, and 18% and 67% in the treatment of P. vivax. These findings suggested that the presence of CQ- and SP-resistant P. falciparum and P. vivax would compromise efforts to control resurgent malaria in Java and that ACTs should be introduced as soon as possible to improve efficacy.
In addition to Central Java there had been a steady rise in the number of reported cases of emerging drug resistance in southern Papua, Indonesia. In collaboration with MSHR, AMI carried out the drug measurements in the assessment of the therapeutic efficacy of CQ monotherapy for P. vivax infections as well as CQ plus SP for P. falciparum infections.56 Of the 143 patients enrolled in the study (40 treated with CQ and 103 treated with CQ+SP), early treatment failures occurred in 15% of patients with P. vivax and 4% of patients with P. falciparum The failure rates by days 28 and 42 were 65% for P. vivax and 48% for P. falciparum, respectively. These findings further confirmed the existence of a high prevalence of drug resistance of P. vivax and P. falciparum to both the first- and second-line treatments in Indonesia.
Prevalence and extent of pyrimethamine resistance in
Plasmodium vivax
The above mentioned study in Timor Leste exemplified the fact that genetic mutations in the dihydrofolate reductase (DHFR) of P. falciparum could also be used to assess drug resistance to pyrimethamine and SP. Furthermore, one to four genetic mutations in DHFR of P. vivax had been shown to confer various degrees of resistance to pyrimethamine and other antifolate drugs. How prevalent might genetic mutations in Pvdhfr be in different areas of the Asia- Pacific region? In collaboration with QIMR, NAMRU 2 and WRAIR, 70 P. vivax isolates from six countries were examined for mutant genes.57 Overall, 74% of P.vivax isolates carried a mutant Pvdhfr, with the prevalence of mutants being lower in isolates from China, Philippines, Timor Leste and Vietnam than in those from PNG and Vanuatu. Furthermore, they only carried single or double mutations whereas isolates from PNG and Vanuatu carried up to quadruple mutations. The data suggested that both the prevalence and degree of resistance of P. vivax to antifolate drugs was higher in the Southwest Pacific countries of PNG and Vanuatu than in their counterparts in Southeast Asia. Because sulfadoxine could not be expected to potentiate the activity of pyrimethamine, these findings indicated the limited value of SP for the treatment of vivax infections.
Efficacy of sulfadoxine-pyrimethamine (SP) combined with artesunate or chloroquine (CQ) against Plasmodium vivax malaria in Papua, Indonesia
Widespread CQ resistance of P. falciparum and P. vivax in Papua, Indonesia, during the late 1990s led to the use of CQ/SP combinations and the evaluation of artesunate/SP. Since artesunate/SP proved highly (96%) effective in curing falciparum infections, NIHRD and MSHR conducted a study to compare the efficacy of this combination with that of CQ/SP in two groups of patients with vivax malaria.58 Not unexpectedly, the treatment failure rate was higher in the CQ/SP group (33%) than in the artesunate/SP group (10%), and would have been higher in patient groups who were not partially immune to malaria. In fact, molecular analysis of parasite samples at AMI revealed that 80% of these patients were infected with parasites carrying one to four genetic mutations in the P. vivax dihydrofolate reductase (pvdhfr) gene and that patients infected with parasites carrying quadruple mutations had a higher risk of treatment failure. Although artesunate/SP was more effective than CQ/SP, it was obvious that an alternative drug, such as piperaquine, might prove to be more useful than SP as a partner for artemisinin-based combination therapy (ACT).
In vitro drug susceptibility of malaria parasites in Vanuatu
In collaboration with VBDCU and NAMRU-2, a preliminary survey was conducted in Malo Island to assess the in vitro susceptibility of malaria parasites to various drugs.59 Using the WHO microtest, six P. falciparum isolates showed a low level of resistance to CQ and pyrimethamine, but were sensitive to mefloquine, cycloguanil, dihydroartemisinin and amodiaquine. The parasites were also 50 to 400 times more active against WR99210, a remarkably active experimental antifolate drug,5,6 than against pyrimethamine. Although patients with falciparum malaria on this island might have a recrudescence of parasitaemia following CQ treatment, the results indicated that they should be cured after SP treatment. No conclusions were possible regarding the drug susceptibility of P.vivax because only two isolates were cultured.
6. NEW INSIGHTS AND TESTS FOR DRUG RESISTANCE
Drug susceptibility test for Plasmodium vivax
In vitro assessment of drug activity against malaria parasites had been an integral part of AMI activities for many years. The WHO in vitro field test (schizont maturation test) had proven to be a simple and reliable means for determining the sensitivity of P. falciparum to antimalarial drugs. However, early attempts to use this test for P. vivax had proven unsuccessful because, unlike P. falciparum, parasite stages other than rings were usually present in the peripheral blood at the start of culture. With recent advances in in vitro culture techniques, further efforts were made at AMI and in Thailand (in collaboration with MAH and AFRIMS), to develop an effective in vitro field test to determine the sensitivity of P. vivax to various drugs.60 Although the processing of freshly-collected parasitised blood samples was more complex than for P. falciparum, it was still considered possible to use this method in a field setting. Chloroquine, sulfadoxine and tafenoquine halted maturation of P. vivax at the late amoeboid or trophozoite stage, whereas dihydroartemisinin did so at the ring stage. As with the P. falciparum test, this field method avoided the use of expensive or dangerous reagents (monoclonal antibodies or radioisotopes) and expensive equipment (beta counters or robotic plate washers and dispensers). The whole 25-37 hour procedure also did not require a biological safety hood. With increasing concern about the emergence of drug-resistant vivax malaria, it was felt that this field in vitro assay could be used for assessing the true drug susceptibility of P. vivax in various areas, without being obscured by various degrees of immunity acquired by malaria patients. Furthermore, in view of the inability to maintain P. vivax in long-term cultures, the test might also play a role in screening new antimalarial drugs for their efficacy against this species.
Polymorphism of pmvdr1 possibly associated with
Plasmodium vivax resistance to chloroquine
Unlike P. falciparum, no genetic markers for CQ resistance had yet been identified for P. vivax. A collaborative effort attempted to shed further light on this by examining the chloroquine susceptibilities (using a modification of the above mentioned in vitro test) and molecular polymorphisms of P. vivax isolates collected in Papua, Indonesia, where high levels of clinical CQ resistance prevailed, and from Thailand where CQ treatment was still generally effective.61 Isolates from Papua were considerably less susceptible to chloroquine than those from Thailand, although in vitro results raised the possibility of a low level of CQ resistance along the western border of Thailand.
Significantly, molecular analysis of the pvmdr1 gene revealed that 96% of Indonesian isolates had the Y976F allele compared to 25% in Thai isolates. It is noteworthy that the 976 mutation was not always associated with high IC50 CQ values, suggesting that other major molecular determinants were likely to be involved. Nevertheless, the predominant presence of the Y976F allele in Papua, known for its widespread clinical resistance to CQ treatment, indicated that pvmdr1 played an important role in modulating the susceptibility of P. vivax to CQ. Since gene amplification of the pfmdr1 gene had already been shown to be a major determinant of multidrug resistance in P. falciparum, this might indicate similar molecular mechanisms for P. vivax resistance to CQ. This study not only emphasised the need to further refine the in vitro test as a means of identifying the presence of chloroquine resistance, but also raised the possibility that the pvmdr1 polymorphism at Y976F might provide a useful tool to monitor the emergence of CQ resistance.
Identification of molecular markers for sulfadoxine resistance in Plasmodium vivax
Although widely used for treating falciparum infections, SP was less effective against P. vivax because its sulfadoxine component was less able to potentiate the activity of pyrimethamine against the parasite.52 To understand the mechanism of this innate resistance to sulfadoxine, studies were undertaken to identify and sequence the P. vivax dihydropteroate synthetase (DHPS) gene, construct a 3D homology model of the DHPS enzyme, and investigate the interactions between sulfadoxine and DHPS.62 As a result, an amino acid residue (V585) unique to the P. vivax DHPS was identified causing a reduction in binding to sulfadoxine. This explained why P. vivax was innately less susceptible to sulfadoxine than P. falciparum. After examining pvdhps in a number of P. vivax isolates collected from different areas, mutations were identified in some isolates which were likely to be responsible for acquired resistance to sulfadoxine. These mutations were subsequently validated as molecular markers for SP resistance in Thailand63 and other areas,57 and have been used worldwide for monitoring SP resistance.
Plasmodium falciparum cultures used to assess the activity of dihydrofolate reductase (DHFR) inhibitors on Plasmodium vivax
As described above, treatment of most malaria patients in endemic areas was based on a clinical diagnosis rather than a parasitological one. In areas where P. falciparum and P. vivax co-existed, this implied that the drug(s) used for treatment of multidrug-resistant falciparum malaria also needed to be effective against vivax malaria. With the increased prevalence of CQ-resistant and SP- resistant P. vivax and the inability to culture P. vivax continuously, P. falciparum from continuous culture was transfected with functional P. falciparum and P. vivax dhfr-ts alleles.64 The development of this P. falciparum expression system allowed for the first direct assessment of the effect of DHFR inhibitors on P.vivax DHFR.
Previous investigations at AMI with one of these DHFR inhibitors, WR99210, had shown this new antifolate drug to be far more effective than conventional antifolates against drug-resistant P.falciparum.5,6 How effective would it be against drug-resistant P. vivax? The results showed that the PvDHFR quadruple mutant conferred greater resistance to WR99210 than the PfDHFR quadruple mutant. This was also the case for cycloguanil and clociguanil, but not for pyrimethamine. Further work, including modeling of both P. vivax and P. falciparum DHFR quadruple mutants suggested that mutations unique to P. vivax DHFR were responsible for differences observed in parasite susceptibility to antifolate drugs. Looking ahead, the development of the P. falciparum expression system appeared to be an important step forward in identifying potential P. vivax drug-resistance markers and in investigating the potency of existing and novel antimalarial drugs against known or putative P. vivax gene targets.
Molecular changes are associated with the development of Plasmodium falciparum resistance to artemisinin derivatives during in vitro cultures
During the previous decade AMI had carried out numerous studies relating to the in vitro and in vivo efficacy, and the pharmacokinetics of existing and novel artemisinin derivatives. In view of the increasing reliance of artemisinin-based combination therapy (ACT) for treating drug-resistant falciparum malaria (see above), there was mounting concern about the possible emergence of parasite resistance to the artemisinins. This prompted WRAIR and AMI to collaborate on investigating the development of artemisinin resistance in vitro.65 Applying discontinuous drug selection pressure, resistance to artemisinin derivatives was established in several clones and lines of P. falciparum. Furthermore, apart from parasites being also cross-resistant to mefloquine and other artemisinin derivatives, they were able to tolerate artemisinin concentrations equivalent to those usually found in plasma samples after treatment of malaria patients.
The development of artemisinin-resistant parasites in vitro provided the opportunity to study various aspects of artemisinin resistance, including the identification of putative molecular markers of resistance to these drugs. Preliminary data suggested that parasites could tolerate increasing concentrations of artemisinin drugs by amplifying the pfmdr1 gene, but they also suggested that this was not the central determinant of artemisinin resistance. Nevertheless, since amplification of pfmdr1 was also associated with mefloquine resistance, attention was drawn to the possibility that this might have practical implications for the use of artesunate- mefloquine as an ACT in areas with high levels of mefloquine resistance. Finally, it was pointed out that the artemisinin-resistant mutants produced during these investigations constituted an important resource in the further search for molecular markers of artemisinin resistance.
7. EVOLUTION OF DRUG RESISTANCE
The aim of these NIH-supported studies was to obtain a better understanding of how malaria parasites developed drug resistance and what host, parasite and environmental factors might enhance or hinder the development and spread of drug resistance.
Origin and dissemination of chloroquine-resistant (CQR)
Plasmodium falciparum in the Philippines
Following identification of the pfcrt gene as CQR marker,6 mutation patterns were suggesting that CQR parasites had arisen independently in four different parts of the world: (1) Southeast Asia, then spreading to Africa; (2) Peru in South America; (3) Colombia, South America; and (4) Papua New Guinea. However, it was not clear how CQR parasites had developed and spread in Asia/Pacific countries other than PNG. During the CQ efficacy study conducted in Timor Leste,6 the pfcrt mutation patterns in P. falciparum parasites indicated that CQR parasites shared a common origin with CQR parasites in PNG, suggesting that CQR in Timor Leste had most likely spread from PNG. Further investigations, carried out in collaboration with RITM, revealed that 90% of parasites sampled in Luzon Province, Philippines, carried two novel mutations in their pfcrt gene which had not been reported elsewhere in the world.66
To better understand the development and dissemination of CQR P. falciparum in the Philippines, a collaborative study was undertaken with QIMR to analyse mutation patterns in pfcrt and microsatellite patterns flanking pfcrt in 82 P. falciparum isolates collected throughout the Philippines between 1989 and 2002.67 While mutation patterns demonstrate CQR status, microsatellite patterns point to the origin of CQR parasites. The results showed that the majority of CQR parasites in Luzon Province (in the North) developed in situ while most CQR parasites in Mindanao and Palawan Provinces (in the South) had originated in PNG. These findings demonstrated that CQ selection pressure could induce parasites with different genetic backgrounds to become resistant to CQ by mutating different positions in the pfcrt gene. Such new information should be helpful in gaining a better insight into the evolutionary process of CQR and in preventing a similar process from occurring following the introduction of newer drugs.
Role of antigenic variation in the evolution of drug resistance
Antigenic variation in malaria parasites is a well known phenomenon hampering not only the development of effective vaccines but also of effective drugs. This is facilitated by a family of antigens, P. falciparum erythrocyte membrane protein 1 (PfEMP1), expressed by P. falciparum on the surface of infected red cells which enables them to adhere to the wall of blood vessels and prevents them from being destroyed by the host spleen. Since each parasite expresses only one of its many member antigens at a time, and regularly switches them around, it is able to evade host immunity. The number and diversity of PfEMP1 antigens in each parasite and in a parasite population are important for the survival of drug resistant parasites and determine the speed at which humans develop immunity against parasites. After examining the repertoires and genetic diversity of genes encoding PfEMP1 in isolates collected from the Solomon Islands, Philippines, PNG and Africa, AMI demonstrated that generally each parasite had genes encoding 40 – 50 members of PfEMP1.68 However, each parasite had quite a distinct set of genes, with only 0-6 genes being shared between any two parasite isolates. These findings suggested that the global repertoire for PfEMP1 was immense and could be potentially selected by the host’s immune response against PfEMP1.
Despite the high diversity of genes encoding PfEMP1 between parasites, five genes were identified that were shared at relatively high frequency among 63 genetically diverse P. falciparum isolates collected from five islands in the Western Pacific region. Upon further examination, three of the five genes were located on chromosome 4 near a mutant pfdhfr while two remaining genes were located on chromosome 7 near a mutant pfcrt. Therefore, the conservationof these genes was a result of their physical linkage to SP and CQ resistance markers and a probable outcome of the widespread use of SP and CQ in the region.69 This provided strong evidence that drug resistance can influence the shape of parasite populations.
To understand how and how quickly parasites switch the expression of PfEMP1, the transcription of genes encoding PfEMP1 was studied in a number of human volunteers, infected with the 3D7 line of P. falciparum, who had participated in a vaccine trial conducted at QIMR in the early 1990s.70 The results demonstrated that the expression of PfEMP1 was reinitiated each time after mosquito inoculation of parasites. Parasites then switched away rapidly from the first expressed PfEMP1 likely to facilitate establishment of infection at a rate of about 18% per generation. Subsequent switching at later phases of infection occurred at much lower rates.71 It appeared likely that a parasite requires a group of 15-20 fast switching genes to establish an infection and a group of at least 20 slow switching genes to maintain the infection for transmission to mosquitoes.72 The results indicated that anything that might be able to interrupt the switching of PfEMP1 would probably interfere with the normal life cycle of the malaria parasite.
Loss of fitness in drug resistant parasites
Following the emergence of drug-resistant parasites, would such parasites suffer a loss of fitness compared to their drug-sensitive siblings? The answer to this question could influence strategies used to delay or even reverse the spread of drug resistance. This was examined by comparing the relative fitness of atovaquone resistant P. falciparum parasites to their atovaquone sensitive parent parasites.73 An equal number of resistant and sensitive parasites were combined with each other and, after 100 days of in vitro culture, the ratio of resistant to sensitive parasites was measured. Without any drug pressure, atovaquone resistant parasites that carried two mutations (M133I and G280D) in their cytochrome b suffered a 5 to 9% loss of fitness compared to their sensitive parents. Further molecular modelling revealed that the loss of fitness was due to the mutation (G280D) weakening the binding of cytochrome b to ubiquinones. These findings supported the concept that drug resistance could be reversed if the old drug was withdrawn and a new drug introduced long before the prevalence of resistance prevalence reached fixation. They also highlighted the importance of continuously monitoring the prevalence of drug resistance so that drug policy can be changed in a timely fashion.
Establishing a P. falciparum in-host dynamics model
In addition to epidemiological and laboratory studies, mathematical models were established to study the evolution of drug resistance. Mathematical modelling is a powerful tool for studying interactions of different factors in complex processes and for predicting the dynamics of changes resulting from interventions that are difficult to study using laboratory or epidemiological tools. The first model was an in-host dynamic model which mimicked the dynamics of P. falciparum infections in naïve hosts.74 The model was constructed using data collected during human malaria studies between the 1930s and 1970s and produced output mimicking the infection dynamics of these infections. To ensure that the model prediction was biologically relevant, several parameters were determined experimentally, including PfEMP1 switching rates (see above), pyrogenic threshold, development of clinical immunity, parasite susceptibility to antimalarial drugs, pharmacodynamics/pharmacokinetics of drugs, and interactions between drugs.
Pyrogenic threshold information was obtained by a retrospective statistical analysis of two existing human infection data sets to determine the relationship of P. falciparum parasite density to the onset of fever in naïve human hosts. The pyrogenic threshold (parasite density triggering a fever) varied significantly between different strains and host ethnicities and became progressively higher as immunity developed following one and more attacks of malaria.75 It was well known that individuals living in malaria endemic areas developed an acquired immunity to malaria, following repeated attacks of malaria, which enabled them to remain asymptomatic while still carrying parasites. In developing the P. falciparum in-host dynamics model, the acquisition of clinical immunity was investigated under different conditions of malaria transmission conditions, levels of parasite diversity, and exposure to treatment.76 The time required to develop clinical immunity increased in areas where parasite diversity was high and decreased in areas where transmission intensity was high. Treatment of symptomatic infections did not prevent the development of immunity, only doubled the time required to develop immunity compared to circumstances where no treatment was available.
The P. falciparum in-host dynamics model was used to investigate the evolutionary steps that were involved in the development of de novo SP resistance. The results indicated that the development of SP resistance evolved in three steps: (a) SP selection of existing mutant parasites, which is driven by the long pharmacological half-life of SP; (b) SP selection of parasites with higher resistance, to which the time of treatment plays a role; and (c) treatment failures due to presence of highly resistant parasites. The model output reaffirmed the importance of correct treatment of confirmed malaria cases in slowing the development of SP resistance.77
8. PERSONAL PROTECTION AGAINST MOSQUITOES
Insect Repellents

Figure 8: Collaborative investigation with mosquito repellents at Cowley Beach Training Area, Queensland, April 2001. (L to R) Major S. P. Frances (AMI), Dr N. Beebe (UTS) Major M. Debboun (WRAIR, USA), Senior Colonel
N.V. Dung (VADMP, Vietnam) preparing to test repellent effectiveness on themselves.
Mosquito repellents are an important first line of defence against vector-borne diseases, such as malaria and dengue,78-80 but the ADF repellent provided to ADF personnel was not being widely used by them. Although previous assessment of the repellent (35% Deet in a gel preparation) by AMI had shown it to be effective in providing a broad spectrum of activity against mosquitoes, soldiers complained that it felt uncomfortable on the skin and melted plastic and some other synthetic materials. During the 2000-2001 deployments to Timor Leste, AMI conducted further field observations on the use of insect repellents by ADF personnel and asked them to complete a questionnaire. In their response, 84% of 955 soldiers indicated that they used repellents, but they were mainly commercial repellents purchased by them.78,81 To ensure that ADF personnel were receiving suitable protection, laboratory and field studies were conducted to assess the effectiveness of commercial formulations available in Australia.82
Picaridin was a new repellent which was starting to be used in commercial preparations. In 2001, a collaborative study between AMI, WRAIR and VADMP was carried out at Cowley Beach Training Area (CBTA) in northern Queensland to compare the effectiveness of picaridin and Deet preparations with one another. In night-time tests, both 20% Picaridin and ADF 35% Deet in a gel provided >95% protection against mosquito bites for 7-9 hours. Similar protection was observed in day-time tests with 20% picaridin and 33% Deet in a polymer cream. However, 10% picaridin provided >95% protection for only 2 hours.83
A further field study was conducted at Mt. Bundey Training area (MBTA) in the Northern Territory in March 2003 which compared the effectiveness of 20% picaridin with 20% Deet and ADF 35% Deet in a gel against Anopheles spp. and Cx. annulirostris.
The protection provided against Anopheles spp. was relatively poor, with 20% picaridin and ADF Deet providing >95% protection for only 1 hour. By contrast, the repellents provided good protection against Cx. annulirostris, with 20% picaridin providing 5 hours protection, and both Deet formulations providing >95% protection for over 7 hours.84 A comparison of commercial formulations against primarily Cx. annulirostris was also undertaken in the same area during 2003. Autan Repel (containing 10% picaridin) provided 2 hours protection, RID (10% Deet) 7 hours protection, and Bushman (80% Deet) 8 hours protection. Commercial repellents containing higher concentrations of Deet provided better protection than picaridin.85
Synthetic pyrethroids as barrier treatment for military fabrics
Previous studies at AMI had established the best methods for using permethrin insecticide in DPCU, bednets and tentage.6 In 2000, after a new active ingredient, bifenthrin, became available in Australia, studies were undertaken to determine the potential use of this insecticide within the ADF. Laboratory studies showed that uniforms treated with bifenthrin and permethrin provided similar protection against Anopheles farauti and Aedes aegypti mosquitoes.86 Chemical assays of ADF shirt fabrics showed that active ingredient was lost after cold water washing, with 78.5 to 85% of the active ingredient lost after three cold water washes. Since bifenthrin did not provide any additional protection, it was decided to continue using permethrin, with bifenthrin potentially available as an alternative insecticide.
In early 2003, a field trial was conducted in MBTA to determine the effectiveness of spraying ADF tents with 0.1% bifenthrin as a means of protecting people inside the tents from being bitten by mosquitoes.87 The treated tents provided an 81% increase in protection from mosquitoes entering the tents, and 90.4% increase in protection from biting Culex annulirostris, an important arbovirus vector. In a subsequent study carried out in the Wide Bay Training Area in Queensland (WBTA) during 2005, the effectiveness of bifenthrin and permethrin in preventing mosquitoes from entering tents were compared with one another.88 The results showed that barrier tent treatment provided increased protection against mosquitoes entering tents for at least four weeks, and that both insecticides provided similar levels of protection.88 During further investigations, low concentrations of bifenthrin and permethrin, applied to tent fabric, were discovered to inhibit egg hatching and larval survival of Aedes aegypti in water accumulating in tent folds and, in addition, inhibit bloodfeeding by host seeking adults. In view of the previous long use of permethrin by the ADF and the findings that it was just as effective as bifenthrin, it was decided to continue using permethrin and to reserve bifenthrin for future use. The additional barrier protection against mosquitoes could have important military and civilian applications, such as might occur when the sheltering of refugees requires the quick erection of tents.
9. VECTOR SURVEILLANCE
Timor Leste
In 1999-2000, ADF forces deployed to Timor Leste on peacekeeping duties suffered from high infection rates of malaria and dengue. The disease outbreak and management team deployed to Timor Leste in 2000 (see above) was involved not only in controlling the malaria situation but also contributed to monitoring the dengue outbreak6 and instituting effective control measures. To guard against further outbreaks during subsequent deployments, surveys were carried out around ADF installations along the Timor Leste western border with Indonesia. The vectors of dengue virus, Aedes aegypti and Aedes albopictus, were found both in the towns that were co-located with defence installations and within the defence installations themselves. The larvae of these container breeding mosquitoes were commonly found in portable water containers used by local residents. Multiple breeding sites were also created following the establishment of defence installations, the most common being water trapped in folds of plastic wraps and tarpaulins, and car and truck tyres. The findings of these surveys were communicated to the deployed preventive medicine personnel who carried out source reduction (physical removal of breeding sites) and larviciding.
Anopheline mosquitoes were surveyed to determine the soldiers’ risk of exposure to malaria. The surveys were carried out in the ADF installations by conducting human landing catches. Using this simple technique the degree of exposure the soldiers had to biting anopheles could be determined, the specimens collected were identified using molecular based techniques and further tested for malaria parasite antigen.
Several species of anophelines were found biting humans: An. barbirostris, An. aconitus, An. annularis, An. maculatus, An. peditaeniatus, An. sundaicus, An. flavirostris and a newly discovered species An. vagus genotype B. The most common species biting humans were An. barbirostris and An. vagus genotype B and specimens of both species were incriminated as vectors at the time of these surveys.90 Larval surveys were also conducted around the ADF installations, primarily to identify anopheline breeding sites for larviciding by preventive medicine personnel. Detection of malaria parasites in mosquitoes is a laboratory based procedure requiring specialised equipment; so the surveys in Timor Leste provided an opportunity to evaluate a novel diagnostic test that could be applied in the field.91
During the deployment to Timor Leste, anti-filarial antibody levels were measured in 907 soldiers to determine whether they had been exposed to mosquitoes infected with filarial parasites, the causative agent of lymphatic filariasis.92 Initial testing using Dirofilaria immitis antigen demonstrated that 49 of them (5.4%) developed antifilarial IgG1 antibodies after deployment, and one out of 944 (0.1%) seroconverted to IgG4 antibodies. When a subsample of 88 D. immitis reactive sera was subjected to a test using Brugia malayi antigen at NIH, 46 had elevated IgG antibodies and five had elevated IgG4 antibodies. A total of 24 soldiers seroconverted to B. malayi IgG, and a single soldier seroconverted to IgG4. The study showed that a relatively low number of Australian soldiers seroconverted to B. malayi, indicating a low but measurable risk of exposure to human filarial parasites. This re-emphasised the importance of soldiers adhering to personal protective measures against mosquito bites during their deployment to tropical areas.
Australia
Ross River virus and Barmah Forest virus
In Australia, ADF personnel were at risk of acquiring mosquito-borne infections not transmitted by anopheline mosquitoes. They were at greater risk of becoming infected by arboviruses, such as Ross River (RR) and Barmah Forest (BF), than civilians because they deployed regularly to areas where the natural animal hosts and vector mosquitoes of these viruses were in abundance. Concentration of soldiers within training areas provided alternative human hosts, thereby facilitating the transmission and spread of these viral infections. During the evaluation of tent barrier treatments with bifenthrin and permethrin in WBTA, 3,497 mosquitoes (primarily Aedes vigilax) were collected between January and March 2005 and processed for the presence of arboviruses. None of the 130 pools of mosquitoes showed any evidence of arboviral infection.88 A subsequent longitudinal surveillance study commenced in 2005 revealed that, out of 348 pools of 9,380 mosquitoes (primarily Ae. vigilax, Ae. multiplex, Ae. kochi and Culex annulirostris), five were positive (two Edge Hill virus, one Stratford Virus, and two unidentified).93
Incursion of dengue virus vectors into Australia
In Australia the primary dengue virus vector Aedes aegypti is only found in far northeastern Queensland, but another less efficient vector – Ae. albopictus – has recently been discovered moving south through Papua New Guinea and into the Torres Strait islands.94 Because both species are container breeders and can lay desiccant resistant eggs they are easily transported from one country to another. Consequently, a continual threat existed that these dengue vectors could be introduced into air and sea ports around Australia. A major problem in monitoring for possible incursions was that larvae of both species, the most common stage encountered by preventive medicine and quarantine services, were very difficult to use for species identification. To meet this problem, AMI, in collaboration with UQ and QSH, developed molecular diagnostic tools for identifying these species and for tracking their movement into and within Australia.95-97
Studies on Culex annulirostris – a potential vector of Japanese encephalitis in Australia
The Japanese encephalitis virus had been moving down Southeast Asia through the Malay Archipelago and into Papua New Guinea and, in 1995, there had been an outbreak in the Torres Strait islands resulting in two deaths. Using sentinnel animals, surveillance activities had indicated that the arbovirus was circulating on Cape York Peninsula in wild pig and bird populations though, as yet, there had only been one human case. Although the Asian vector species for this virus is not present in Australia, vector competency studies had shown that Culex annulirostris could readily transmit the virus. However, this species was sometimes difficult to distinguish from Cx. sitiens and Cx. palpalis using traditional morphological markers. To overcome this handicap, AMI collaborated with UQ and QSH in examining the ribosomal DNA Internal Transcribed Spacer Region I to develop a molecular marker to separate the three species reliably from one another.98 The consistency of the procedure was documented following the examination of specimens collected in Australia, PNG and the Solomon Islands. Further collections of field material in Cape York Peninsula and the Northern Territory were analysed using the CO1 gene of the mitochondrial DNA.99 Analysis of the specimens revealed that there are five independently evolving haplotypes of Cx, annulirostris and three independently evolving haplotypes of Cx. palpalis, and that these populations might differ in their ability to transmit Japanese encephalitis on Cape York Peninsula.100
Vietnam
Malaria vectors and malaria transmission in rural villages in Vietnam (2000-2005)
Under the auspices of VADMP, malaria transmission was studied in rural communities in Vietnam. The aim was to determine what anopheline species were present, which were responsible for malaria transmission, and to learn something of their biology and ecology which might aid in their control and the protection of military forces in the field. A field site was selected at Truong Xuan Commune in Quang Binh Province, 500 km south of Hanoi, where malaria transmission was perennial but where less than 15% of the villagers carried malaria parasites. This was primarily due to the fact that the anophelines in the area were not particularly efficient malaria vectors, preferring to feed on cattle and buffalo.101
There was a perception in Vietnam that most malaria was transmitted in the forest by An. dirus, a notoriously efficient malaria vector, and that people contracted the disease in the forest while hunting, timber cutting, and food gathering. At a second field site in Phuoc Chien Commune there was an opportunity to study this concept of forest malaria. Although villagers in the commune lived in the valley floor where they were not exposed to any malaria vectors, they spent several months of the year cultivating their crops on the surrounding hillsides. Vector surveys conducted around these hillside communities showed that An. dirus was present and that a sufficient number of people spent enough time cultivating these crops to sustain malaria transmission.102 These findings had implications for community malaria control activities because indoor insecticide spraying and treated bed nets were only supplied to village houses situated in the valley floor, whereas little or no emphasis was placed on preventing the acquisition of malaria at hillside garden dwellings.
China
Malaria vectors associated with P. vivax epidemics in China
In 2003, AMI received a WHO grant, in collaboration with Dr Nigel Beebe, UTS and Professor Gao Qi (JIPD), to investigate the possible discovery of a new malaria vector in China. During the late mid- 1990s there was a resurgence of vivax malaria in China involving millions of cases. The vector thought responsible for these epidemics was An. sinensis, but this species is primarily zoophilic, feeding mainly on cattle, and therefore not a very efficient vector. Field studies in Chinese provinces where the malaria outbreaks occurred revealed the presence of another anopheline which appeared morphologically similar to An. sinensis but which readily fed on humans. This mosquito was believed to be a new species and was named An. anthropophagus. The aim of the collaboration was to determine, using molecular tools, if An. anthropophagus was indeed a new species and not An. sinensis. Analysis and sequencing of the ribosomal DNA Internal Transcribed Spacer Region II showed that An. anthropophagus and An. sinensis were in fact different species.103 Following the epidemics in China, the Korean Peninsula experienced severe epidemics of vivax malaria in the early 2000s. As in China, An. sinensis was at first thought to be responsible, but the vector was later found to be a closely related species – An. lesteri. Further studies revealed that An. anthropophagus and An. lesteri were in fact the same species, thus incriminating An. lesteri as the major malaria vector responsible for the malaria epidemics in both China and the Korean Peninsula.
10. VACCINE DEVELOPMENT
Dengue
The dengue outbreak among ADF personnel in Timor Leste provided the impetus for AMI to conduct the first tetravalent dengue vaccine study in Australia involving 10 healthy volunteers admitted to the military hospital at Gallipoli Barracks, Brisbane. The Phase 1b study was designed to evaluate the immunogenicity and safety of two live attenuated vaccine formulations. After one injection, all subjects reported systemic reactions consistent with a mild dengue-like syndrome. Seven volunteers developed dengue 3 viraemia after vaccination and all of the volunteers developed a neutralizing antibody response against serotype 3, with a partial response against other serotypes. The study was terminated early due to formulation issues relating to the dengue 3 vaccine component. Managing viral interference and balancing attenuation to produce acceptable tetravalent immunogenicity with minimal reactogenicity may be a recurring problem for future multivalent live vaccines. This initial study with dengue vaccines led to a long-standing collaboration between AMI, AP and ACR to evaluate chimeric arboviral vaccines using their envelope antigens combined with a core yellow fever vaccine.
Japanese encephalitis
With the spread of Japanese encephalitis (JE) throughout the region and even into mainland Australia, almost half of the ADF budget for vaccination was being spent on protecting its military personnel against this mosquito-borne disease.105 In efforts to extend the lifespan of the Australian stockpile of the discontinued Biken JE vaccine, previous studies at AMI had shown that comparable serological levels of immunity could be attained by administering considerably lower doses of the vaccine intradermally rather than by subcutaneous inoculation.6 Furthermore, cellular immunity continued to provide protection following the decline of antibody levels.106,107 Although this inactivated, mouse brain-derived vaccine induced a good immune response, there was uncertainty about the duration of protection and concern about some infrequent adverse events following immunisation, and production of the Biken JE vaccine was completely discontinued in 2005.
In 2003, a randomised double-blind study involving 202 healthy ADF personnel was initiated to evaluate the safety, immunogenicity and persistence of antibodies after administration of a live, attenuated JE chimeric virus vaccine (JE-CV) – Chimerivax™- JE.108 To assess adverse events related to vaccination, volunteers were randomised to receive the vaccine and placebo subcutaneously 28 days apart in a cross-over design. A subgroup of 98 participants were inoculated with a JE-CV booster six months later to determine whether this would prolong the protective efficacy of the vaccine. Vaccination was well tolerated and the incidence of reactions was comparable to that observed after placebo inoculation. Almost all volunteers (99%) achieved seroprotective antibodies within 28 days of receiving the single dose of JE- CV vaccine and 90% were still seroprotected two years later. The seroprotection rate at this time was even higher (99%) for those JE-CV recipients who received a booster dose at six months. These findings indicated that JE-CV vaccination was safe and that just a single dose provided prolonged immunity against JE infection. Plans were put in place to continue monitoring seroprotection for another three years into the 2005-2010 quinquennium.
In 2004, a further randomised double-blind study involving 108 volunteers was carried out to evaluate the safety and efficacy of concomitant or sequential administration of JE-CV vaccine and yellow fever 17D vaccine (YF-17D).109 The rationale for this study was based on the fact that JE-CV was produced by removing the pre-membrane and envelope coding sequences from the yellow fever virus and replacing them with the corresponding sequences from an attenuated strain of the JE virus. Consequently, both vaccines shared antigenic determinants and non- structural coding sequences which might boost or suppress immune responses if these vaccines were administered at the same time or in either order one after the other. After administering two inoculations,
30 days apart, using various JE-CV, YF-17D and placebo cross-overs, there were no serious adverse events and seroconversion rates were above 90% in all the groups. Neutralising antibodies against the JE and YF vaccines continued to be detected in 82- 100% of volunteers up to the last follow-up blood sample collected six months after immunisation. The results suggested that both vaccines could be given together, either concurrently or 30 days apart, without reducing their protective efficacy.
In order to exclude the possibility that vaccinees might transmit JEV to susceptible mosquitoes, Culex annulirostris, Culex gelidus, and Aedes vigilax were fed on Chimerivax™-JE.110 None of the mosquitoes fed on the vaccine became infected, in contrast to mosqitoes fed on JEV-Nakayama or the yellow fever vaccine virus 17D. The findings indicated that it was unlikely that transmission of JEV could be established in Australia following vaccination with Chimerivax™-JE.
11. TECHNICAL ADVICE AND TRAINING
AMI continued to provide the Office of the Surgeon General with periodic updates regarding malaria and other VBDs, including a review of Policy Directive 215 and subsequent issue of a new version in 2005. In addition to responding to frequent enquiries by medical staff regarding prevention and treatment of VBDs of ADF personnel, AMI was actively involved in providing assistance and training to preventive medicine personnel during field deployments. In 2004 a new annual training course was initiated in “Vector Borne Diseases Surveillance and Control”. This one-week course for preventive medicine technicians was administered by Army Logistic and Training Centre, and conducted by AMI staff.
Following inauguration of the Vietnam Australia Defence Malaria Project, AMI hosted medical officers and scientists from Vietnam and trained them in all aspects of work undertaken at the Institute. Concurrently, AMI staff benefited greatly from experience gained during joint clinical and field studies conducted in Vietnam. Apart from contributing to WHO-sponsored training projects in various locations (see above), AMI staff continued to remain involved in other less structured efforts to promote training and information on VBDs.
Conclusions
The second half of the fourth decade (2000-2005) was characterised by the most wide-ranging and significant activities yet undertaken by AMI. Many of them could not have been carried out without the continued collaboration with other institutions in Australia and overseas. Significant events and achievements included:
- Successful control of malaria and dengue outbreak among Australian peacekeepers in Timor Leste following various epidemiological, chemoprophylactic and mosquito control measures instituted by AMI field
- Demonstration that currently-used regimens of antimalarial drugs, including mefloquine and primaquine, can be modified to provide more effective protection against malaria under field
- Prospect that tafenoquine, a new, long-acting synthetic analogue of primaquine, might not only improve compliance with post-exposure prophylaxis and treatment regimens, but might provide protection against vivax and falciparum malaria while in malarious
- Assessment of the influence of food, gender and pregnancy on the effectiveness, tolerability and/ or pharmacokinetics of various antimalarial
- Demonstration that artemisone, a new artemisinin derivative, is more active in vivo than other artemisinins in curing falciparum
- Detailed evaluation of malaria rapid diagnostic tests (RDTs) and development of in vitro drug susceptibility test for vivax.
- Identification of molecular markers for vivax resistance to chloroquine and sulfadoxine.
- Documentation of worsening resistance of first- and second-line drugs used for malaria treatment in various parts of the Asia/Pacific
- In vitro assessment of drug activity against vivax parasites enabled by successful transfection of P. vivax genes to P. falciparum.
- Artemisinin resistance of falciparum in vitro, produced by applying discontinuous drug selection pressure, is associated with amplification of the pfmdr1 gene.
- Investigation of factors influencing the evolution and spread of drug resistance in malaria
- Evaluation of insecticides applied to skin, clothing and tents to maintain optimum protection against mosquito
- Entomological investigations in northern Australia with vectors of Ross River, Barmah Forest, Dengue and Japanese encephalitis
- Epidemiological investigations with malaria vectors in Vietnam and China.
- Inititation of dengue vaccine
- Prolonged protection against Japanese encephalitis obtained after administration of a single dose of a live, attenuated JE chimeric virus vaccine (JE-CV).
- Consolidation of close collaboration with US and Vietnamese Army investigators following the establishment of a Walter Reed Army Institute of Research laboratory at AMI and inauguration of Vietnam Australia Defence Malaria Project (VADMP) laboratories in Hanoi.
- Redesignation of AMI as a WHO Collaborating Centre for 4 years, with AMI hosting, participating in, or conducting several WHO-sponsored courses, conferences or workshops.
Highlights
2000/2001
- Vietnam Australia Defence Malaria Project (VADMP) established (2000-2005).
- Walter Reed Army Institute of Research laboratory established at AMI following arrival of Lieutenant Colonel Dennis
- Investigations on “Evolution of drug resistance in falciparum” commence under three-year NIH RO1 grant (2000-2003).
- AMI field teams control malaria and dengue outbreak in ADF personnel deployed to Timor
- Shorter and higher dose primaquine regimens evaluated to determine tolerability and effectiveness for post-exposure prophylaxis and radical cure of vivax malaria.
- Weekly tafenoquine prophylaxis during six- month deployments on peace keeping duties in Timor Leste prevents falciparum and vivax malaria both during and following
- Population pharmacokinetics of tafenoquine supports the use of a loading dose of 200 mg daily for 3 days followed by 200 mg weekly for six months for effective malaria protection.
- Mosquito repellents evaluated at Cowley Beach Training Area, Queensland
- WHO in vitro test modified to assessof vivax susceptibility to antimalarial drugs.
- Entomological investigations in Timor Leste identify potential malaria vectors and incriminate a new vector species.
2002
- AMI hosts WHO-sponsored 13th Southwest Pacific Malaria meeting.
- Official opening of VADMP laboratories in Hanoi.
- Large-scale study with mefloquine, including pharmacokinetic evaluation, indicates that 250 mg every other day during the first week followed by the same dose once a week is well tolerated and effective in providing malaria protection for six months.
- Artemisone is more effective than other artemisinin drugs in curing falciparum infections in Aotus monkeys.
- Increased plasma clearance (50%) of atovaquone, proguanil and cycloguanil in pregnant malaria patients suggests that the dose of atovaquone- proguanil might need to be increased for the treatment of malaria during pregnancy.
- P. falciparum parasites process a highly diverse family of PfEMP1 on the surface of red cells and switch rapidly between these antigens to establish an infection.
- Sulfadoxine/pyrimethamine treatment is less effective in patients infected with vivax carrying a quadruple mutant dihydrofolate reductase (DHFR) gene.
- Atovaquone-resistant parasites are less fit than sensitive parasites, suggesting reversal of drug resistance following use of alternative drugs.
- Molecular diagnostic tools are developed to identify larvae of dengue virus vectors and to prevent their importation into Australia.
2003
- Lieutenant Colonel Robert Cooper replaces Lieutenant Colonel Michael Edstein as Commanding Officer.
- Amplification of pfmdr1 gene plays an important role in the development of falciparum resitance to artemisinin drugs.
- Chloroquine resistance in the Philippines is due to mutations of both indigenous and imported parasites from Papua New Guinea.
- Field evaluation of picaridin as a mosquito repellent and of bifenthrin as barrier treatment in military shirts and tents at Mount Bundey Training area, Northern Territory.
- Food containing 30 g fat may enhance primaquine effectiveness by augmenting plasma drug concentrations.
- New molecular diagnostic tools are developed to identify potential Japanese encephalitis vectors in Australia.
- Immunisation with live, attenuated Japanese encephalitis chimeric virus vaccine (JE- CV) is safe and induces seroprotection for at least two years.
2004
- High dose, shorter courses of primaquine are tolerated just as well as longer primaquine courses by glucose-6-phosphate dehydrogenase normal Australian soldiers.
- Seven-day courses of primaquine (22.5 mg twice a day), preceded by two days of artesunate (200 mg twice a day) are well tolerated and effective in Vietnamese patients infected with vivax malaria.
- Pharmacokinetic studies with artemisone during Phase I human safety and toxicity studies support the potential value of this drug for artemisinin combination therapy.
- P. vivax is both innately resistant and can develop resistance to sulfadoxine due to variation and mutation, respectively, of the parasite’s dihydropteroate synthetase (DHPS) enzyme.
- Investigations on “Antigenic variation and drug resistance in falciparum” commence under second three-year NIH RO1 grant (2004-2007).
- P. falciparum in-host dynamics model assists in understanding diverse factors influencing the development of host immunity and the evolution of drug resistance.
- Field evaluation of commercial repellents in Queensland
- Entomological studies identify the malaria vectors in rural communities in north central Vietnam and investigate their biology and behaviour.
- Long-term persistence of neutralising antibodies after sequential administration of JE- CV and yellow fever 17D vaccines suggest that both vaccines can be given together without reducing their protective efficiency.
2005
- Food containing 17 g fat increases plasma piperaquine concentrations in healthy Vietnamese soldiers, which may benefit malaria patients receiving ACT using this drug and dihydroartemisinin.
- Relapses of vivax infections in ADF personnel deployed to Timor Leste result from activation of a single strain of hypnozoite in the liver.
- Highly diverse target antigen HRP2 may cause variable sensitivity of malaria RDT’s, whereas highly conserved aldolase produces more reproducible test results but is less sensitive than HRP2.
- Pvmdr1 is a molecular marker for drug resistant P. vivax, with mutant pvmdr1 predicting chloroquine resistance while multicopy pvmdr1 predicts mefloquine resistance.
- P. falciparum expression system established to assess P. vivax response to dihydrofolate reductase (DHFR) inhibitors.
- Drug resistance exerts a strong force in shaping a parasite population.
- Barrier treatment of tents with bifenthrin is just as effective as permethrin in reducing exposure to mosquitoes in the Wide Bay Training area, Queensland.
- Entomological aspects of forest malaria studied in central Vietnam.





