Abstract
Deployed surgical teams work together to perform time-critical damage control resuscitation. However, the team often includes members who have never worked together or in the field. A successful team can rapidly acquire knowledge of their clinical environment and each other. In this paper, we explain how Immediate Action Drills (IADs) for the operating theatre department (OTD) can be used to orient individual clinicians to the field and how collective training in these drills can maximise the safety and efficiency of the surgical team.
Introduction
Damage control resuscitation and initial wound surgery are vital capabilities of deployed health facilities that emerge from the time-critical integration of multiple clinical teams, from reception in the emergency department to post-operative critical care. In the contemporary Australian Defence Force (ADF), these clinical teams comprise both full-time and part-time clinicians who are often drawn from several different units and may or may not have previous experience working together or in the field.
Capability can be defined as ‘the power to achieve a desired operational effect in a nominated environment within a specified time, and to sustain that effect for a designated period’.1 From this, to achieve the capability of damage control resuscitation, deployed health facilities must be able to draw upon a pool of clinicians who have achieved individual operational clinical readiness.2 These individuals must then be oriented to the deployed environment and rapidly acquire the ability to synchronise their clinical behaviours within a team likely to contain several unfamiliar faces. Further, the team must have robust processes to induct new members during sustained operations. In many ways, this makes a clinical department such as a deployed operating theatre very different from other high-performing military teams, which draw upon individuals who have completed standardised initial and advanced training and are likely to have substantial experience working together prior to deployment.
We have previously proposed a framework for facilitating individual operational clinical readiness, recognising that reliance upon unstructured civilian clinical experience cannot guarantee competent and confident proceduralists to perform battlefield surgery and resuscitation.2,3 In this paper, we outline our approach to promoting collective clinical readiness at the level of field hospital departments, supported by a Field Orientation Manual (Figure 1). Our proposal is consistent with the Australian Army’s training doctrine, which emphasises that commanders must place constant emphasis on tailored training of individuals and teams to generate optimal collective effectiveness.
Goals
Our goals in establishing a field orientation process were to:
- Ensure all clinicians can operate safely in the field environment.
- Ensure that team members know their roles and the location of key equipment and consumables in time-critical clinical scenarios.
- Allow for timely identification of deficiencies and equipment errors before declaring full operational capability (FOC) of a newly deployed operating theatre department (OTD).
- Provide a framework for the preservation of corporate knowledge or ‘lessons learned’ that does not rely upon continuity of staffing.
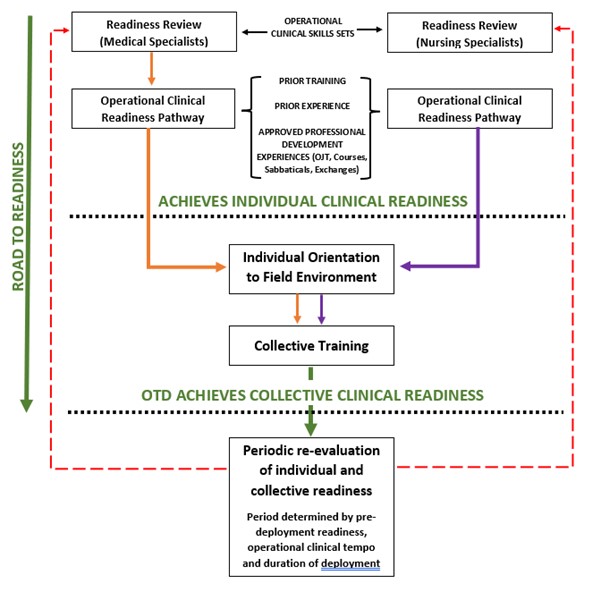
Figure 1: Pathways to individual and collective clinical readiness
Approach
Compared with other military training, exercises involving the deployed health facility have traditionally incorporated individual, small team and whole-of-hospital simulation. However, attending multiple major exercises, we noted that the content of small team or departmental drills is often left to the discretion of the department OIC or the individual specialists within the OTD. These individuals may or may not have previous experience with deployed health care and may not be aware of the range of ‘high acuity low occurrence’ (HALO) events that benefit from rehearsal prior to declaring FOC.
We noted that training serials based on HALO events often resulted in individual team members identifying gaps in their knowledge of OTD processes, as well as allowing for rectification issues such as non-functioning equipment or misplaced consumables. The most prominent example of this was training to manage malignant hyperthermia (MH).5 An MH response is characterised by well-defined individual roles and responsibilities, supported by task cards and team checklists. We see this type of team training as advantageous because it can be ‘walked through’ by a team with no previous knowledge of each other or the physical care environment, and in doing so, it allows them to acquire knowledge of both.
Drawing from these lessons, we identified several other clinical scenarios that demand an immediate, coordinated response by the OTD team. These comprise surgical, anaesthetic and logistic crises that feature predefined roles for each team member, which sometimes deviate from their responsibilities during routine operations. These were:
- fire in OTD
- power outage during surgery
- death in the OTD
- rapid theatre turnover
- major trauma
- red blanket (bypass of the resuscitation bay)
- anaphylaxis
- malignant hyperthermia.
Solution
We determined that the best way to ensure a consistent, timely response to each of these clinical scenarios was to develop a series of Immediate Action Drills (IADs) for the OTD. Drills are characterised by a predetermined sequence of actions performed in response to a clearly defined trigger; within the scope of the drill, no further instructions are required from the team leader. Drills are consolidated through overlearning and spaced repetition to enhance performance and long-term knowledge retention.4
Importantly, drills may constitute a complete initial response to a clinical crisis, as is the case for MH or power outage drill (Figure 2), or they may bring the team to a state of collective readiness in preparation for further tasking, as is the case for the major trauma drill. Drills are widely used for this purpose in other military contexts. At the individual level, all are familiar with weapons IAs. Likewise, small teams apply the basic drill, counter ambush drill and chemical, biological, radiological and nuclear defence drills, among many others.
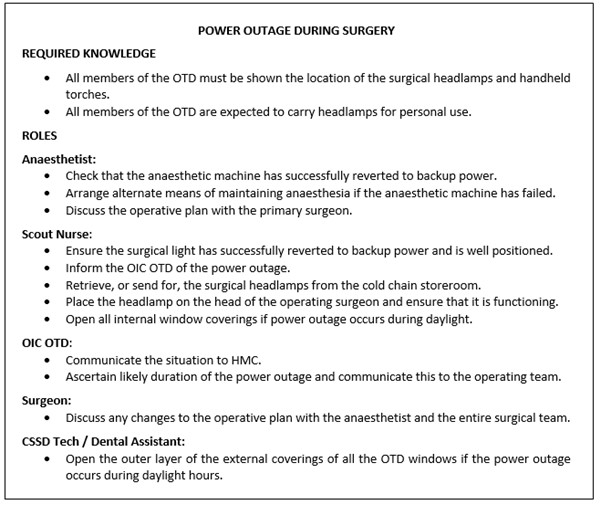
Figure 2: Summary card – power outage during surgery
Team training based on drills offers several advantages over ad hoc clinical scenarios or revision of standard operating procedures (SOPs). First, it allows a new team to swiftly acquire a common language and understand which team member should be expected to undertake each task in time-critical situations. Second, drills provide a ready-made framework for initial training each time the theatre team is constituted, allowing department leadership to focus on devising more complex follow-on training or whole-of-hospital simulation. Third, drills facilitate cognitive offloading of the team leader in a crisis because a single command brings the department to a state of action without the need for detailed instructions. Fourth, drills facilitate tracking of individuals’ orientation to the field. Fifth, drills enable the team to recognise latent factors such as dysfunctional facility layout and equipment deficiencies before receiving the first casualty, consistent with the evidence for in situ hybrid simulation in commissioning new civilian hospitals.6 Finally, drills build team cohesion and facilitate quality assurance through benchmarking of protocol adherence and time to completion.
To facilitate the use of the IADs we developed a Field Orientation Manual for the OIC OTD. This title was chosen to highlight that it should be utilised once a team arrives on location in the field environment and not just as a repository of corporate knowledge but as a tool to orient the team to each other and the environment itself.
The manual contains explanatory material enabling an OIC to implement drill-based team training without prior knowledge of their team or the drills themselves. The OIC can also draw upon a Quick Reference Guide (QRG) that explains key logistic features of the hospital that are needed to execute the various IADs. The QRG outlines the hospital’s pathology and imaging capabilities; composition of standard sets of sutures, anaesthetic drugs and instrument ‘grab bags’; the documentation requirements of the field hospital OTD; and the role of the OTD personnel in the most notable of whole-hospital responses, the mass casualty drill. We believe this ‘walk-through’ guide would enable an entirely new theatre team to achieve collective readiness, consistent work practices and a safe work environment.
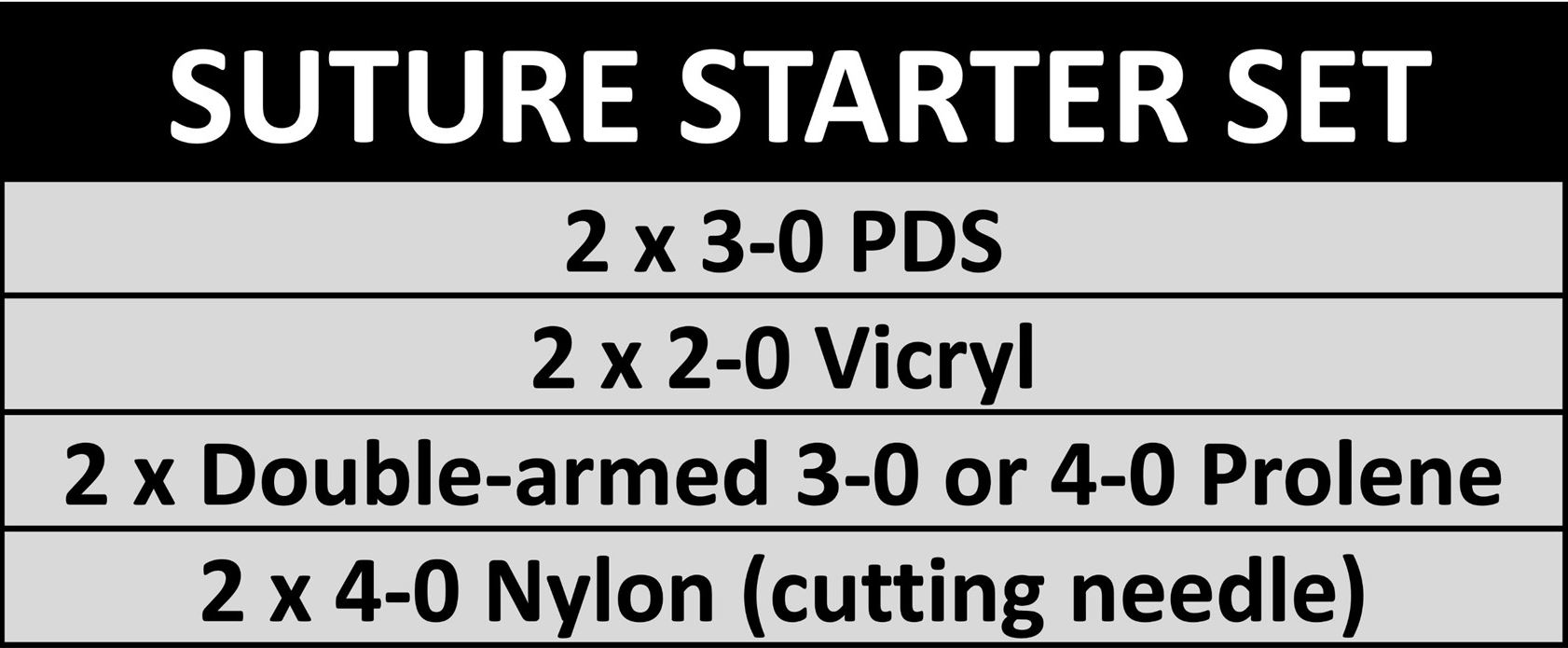
Where deemed useful, we have supported each drill with ‘role cards’ (Figure 3) that outline each role along with other visual aids that can be used for quick reference to check particular equipment, such as the ‘Suture starter set’ (Figure 4) or the ‘Emergency anaesthetic drug set (Figure 5).
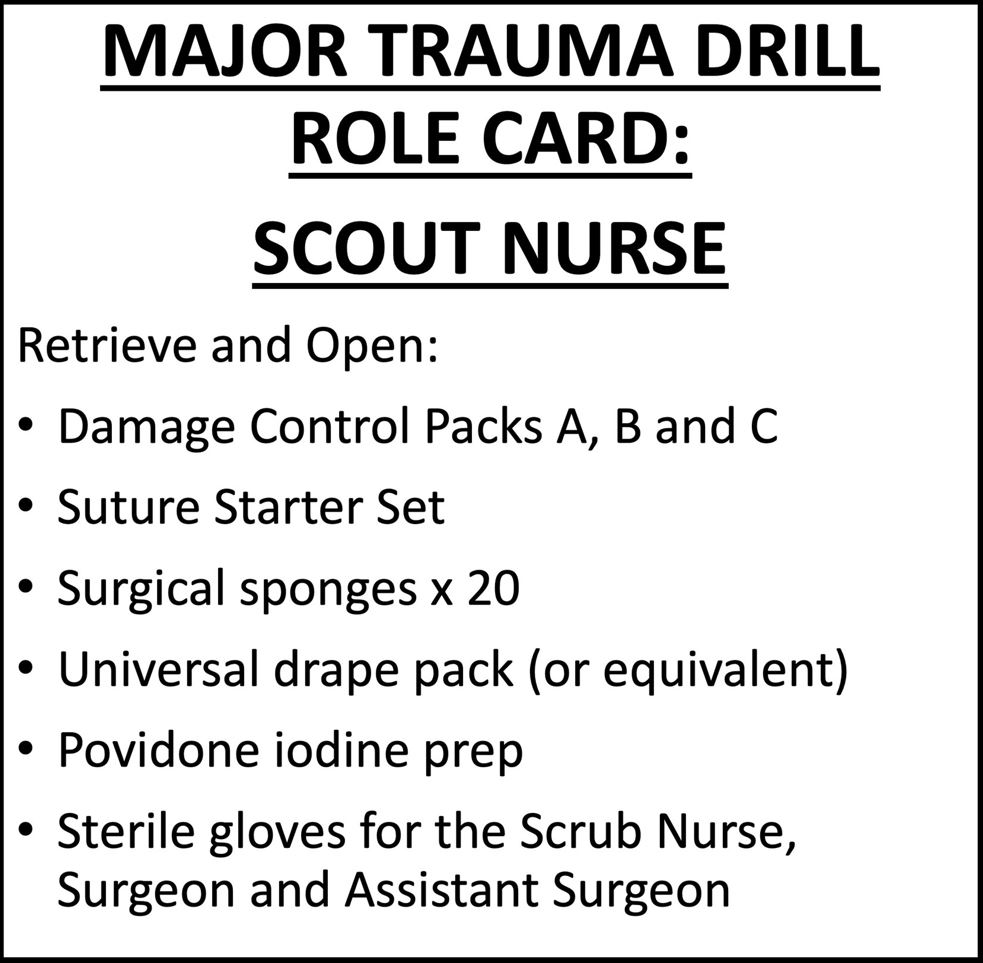
Figure 3: Role card – major trauma drill
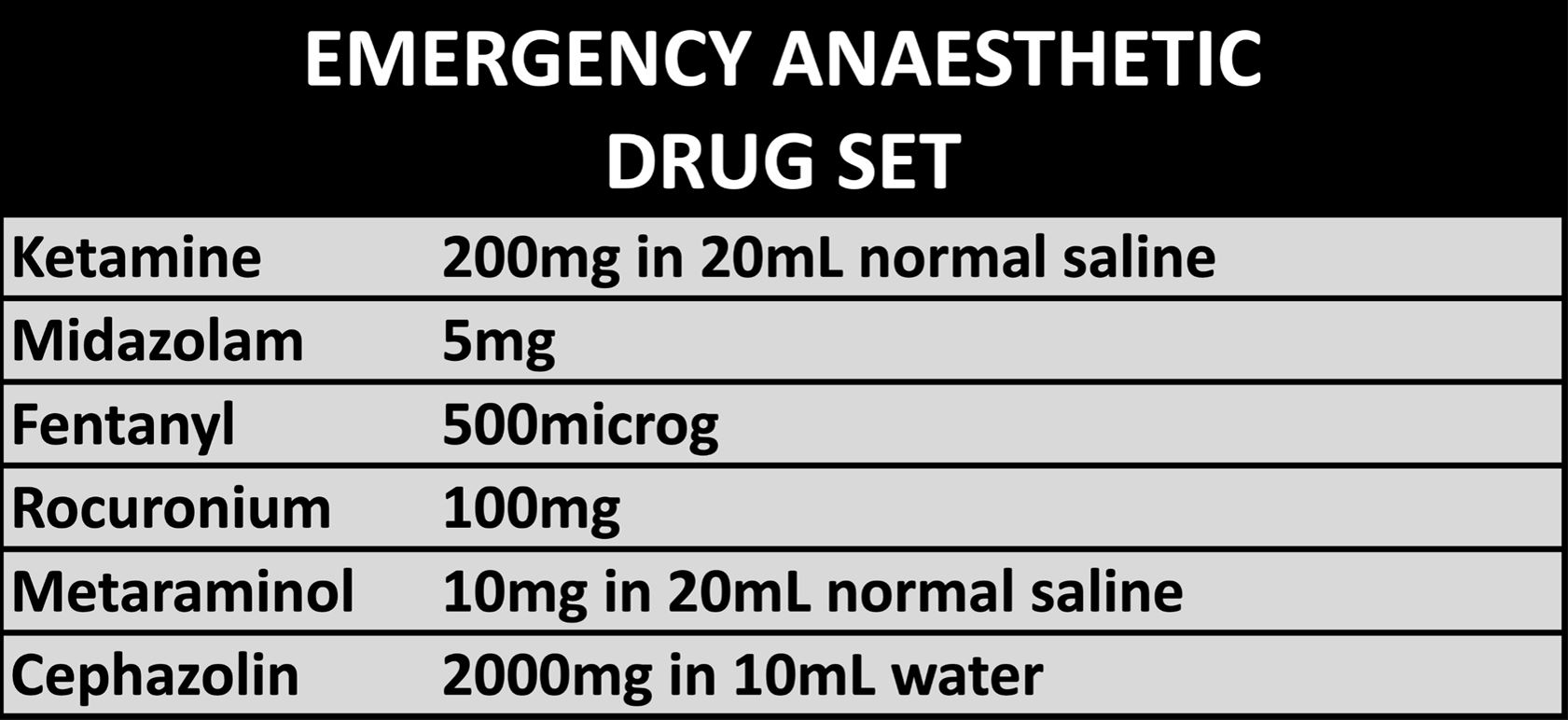
Figure 5 – Emergency anaesthetic drug set
Finally, the overall document also included a compliance tracker, allowing the OIC to mark off each team member as they are oriented to specific equipment and drills of the OTD.
Discussion
In other contexts, it has been said that ‘a good plan, violently executed now, is better than a perfect plan next week’ (Patton). We believe that maxim applies equally to the initial management of high acuity scenarios in the OTD. In the past, we have observed a tendency to ‘reinvent the wheel’ each time an OTD is constituted for deployment or exercise, with each surgeon, anaesthetist or nurse adding or subtracting from the load list and putting their own ‘spin’ on collective practices. While there is much in trauma surgery and resuscitation that cannot be templated, that does not relieve those of us who are professional military trauma specialists from standardising all that we can. A standard tray of instruments and sutures, or routine anaesthetic induction drugs, that can be opened immediately by a scrub nurse or anaesthetic assistant when the major trauma drill is activated is superior to a bespoke list of consumables that can only be readied when the surgeon or anaesthetist returns from the resuscitation bay.
The efficacy of the Field Orientation Manual and its IADs has not been formally evaluated. However, each of the IADs has been piloted at a major exercise, and we have received positive responses from both part- and full-time clinicians of all specialties. We noted IADs enabled team members to ‘work at the top of their scope’; for example, a medic anaesthetic assistant could confidently draw up induction and resuscitation drugs and prime a rapid infuser based on their role outline for major trauma, rather than waiting for a plan from the anaesthetist.
Beyond learning individual responsibilities within a team response, we observed that execution of the IADs orients the team to their physical environment and each other. The fire in the OTD and power outage drills help OTD staff understand the electrical supply to theatre, the location of firefighting equipment and the facility’s layout. The death in the OTD drill introduces the team to broader administrative issues such as casualty tracking and mortuary management in the deployed environment, while demonstrating that time to complete this process affects theatre readiness to receive further casualties. The major trauma and red blanket drills familiarise the team with the surgical equipment, and the anaphylaxis and MH drills are valuable to orient the team to the anaesthetic equipment. Our approach does not obviate the need for more detailed SOPs. These provide an enabling framework for the IADs, as well as guidance on the management of less time-critical situations. Nonetheless, clinical IADs provide a framework for the team to know each other and their environment, enabling recognition of individual and collective capability gaps. We believe a team where all individuals have completed IAD-based orientation training will have a greater capacity to respond to more complex training and care provision demands.
We believe that the utility of clinical IADs should be further evaluated, both within the OTD and other hospital departments. All clinical areas have scenarios that require immediate response with minimal need for variation between instances: for example, resuscitative thoracotomy in the emergency department or unintended extubation in the intensive care unit. This draft proposal has already been replicated in draft form in the OTD of other services. It has been noted as a positive activity in external review processes, such as The Royal Australasian College of Surgeons Trauma Verification.
Conclusion
The OTD Field Orientation Manual is a compendium of IADs targeting a suite of time-critical events in the field hospital operating theatre, supported by decision aids, task cards and visual prompts. The manual can potentially assist team leaders in orienting a new team to the deployed clinical environment and each other. It may help provide continuity of corporate knowledge that otherwise might be lost through the rotation of experienced members, allowing past lessons to be preserved rather than learned repeatedly. It may also give confidence to hospital commanders, who will know that an OTD that has completed individual and collective rehearsal of the IADs is at full operating capability. Our model is consistent with Army’s broader training philosophy, and we advocate further evaluation of clinical IADs in all deployed hospital departments.
Corresponding Author: Adam Mahoney, adam.j.mahoney@gmail.com
Authors: A Mahoney1, K W Bender1
Author Affiliations:
1 Australian Army – 2nd Brigade