Introduction
With a growing frequency of extreme weather events, associated natural disasters1 and military conflicts, there is an increasing incidence of fractures requiring emergency treatment in the context of ‘damage control’ using simple methods such as an external fixator. As Martinez-Rondanelli et al. point out in their 2021 manuscript on damage control in orthopaedics and traumatology,2 polytrauma stands as a significant contributor to mortality among individuals under 40 years of age, with 55 per cent of these cases involving fractures of the long bones or pelvis. In 31 per cent of the patients, orthopaedic damage control procedures were conducted during the initial surgery.
Although information on the treatment of the consequences of injuries is available from the international community, as in the webinars provided by the AO (Arbeitsgemeinschaft für Osteosynthesefragen) in the context of the war in Ukraine,3 implementation is limited in disaster situations by the scarce medical infrastructure and quantity of materials available, as recently reported by Médecins Sans Frontières.4
If these fractures cannot be treated, they cause not only fatal consequences but also long-lasting disability. Due to the severity of these injuries, the limbs often have to be amputated, even though they could be saved under normal circumstances.5 In many countries, the loss of a limb leads to disability, combined with loss of income and other severe consequences for the individual and their family.6
The external fixator is the method of choice in emergencies when fractures cannot be treated using a cast due to soft tissue damage or gross instability. Further, as Dunn et al. pointed out in their 2022 article on damage control,7 the use of initial external fixation, in contrast to definitive internal fixation, aims to reduce the occurrence of post-operative systemic inflammatory response syndrome, multiorgan dysfunction, overall surgical complications, acute respiratory distress syndrome, surgical blood loss and reduces the duration of the procedure, which in return reduces the chance of perioperative complications.8
Commercially available external fixator systems used in these cases have several flaws in disaster situations: they are only available in limited quantities, are heavy and expensive, and require special tools and training.
Attempts have been made to develop 3D-printed clamps,9 tool-less10 and low-cost systems11 with no success combining all features in one clamp.
The project aimed to develop a fixator that bypasses the limitations of being costly, requiring training and the need for special tools. The developed clamp’s performance should be tested compared to a commercially available external fixator.
Materials and methods
The study was carried out within the framework of a translational project by the University Hospital of Hamburg UKE, the BG Klinikum Hamburg and the Bundeswehr Krankenhaus Hamburg (military hospital). As no patients or patient data were involved, the study did not have to be registered in the clinical trial registry. It nevertheless strictly followed a predefined study protocol. No funding was received for the project.
According to current plans, the fixator is aimed to be a disposable external fixator used for temporary care and applied under emergency conditions in natural disasters and military conflicts under limited logistical conditions. Objectives of the system are:
– low-cost manufacturing
– short-term, demand-optimised, decentralised production
– intuitive handling with minimal tools and little training required
– compatibility with existing systems
– rod-to-pin and rod-to-rod fixation with the same clamp
Fixator-System A – Wingman external fixator
The newly developed fixator system can be seen in Figure 1(A) and has been called ‘Wingman’ due to its ergonomic handle shape that is reminiscent of wings that unfold and was developed in association with the company Bluewater Medical (BLUEWATER MEDICAL GMBH, Faulmannweg 5, 24148 Kiel, Germany). The reason for the shape was to increase torque for tightening. A snap-in-retention was built in to avoid unintended unlocking (Figure 1(B)). One coupling could adapt a Ø5 mm shaft pin (Figure 1(A)) and up to two 11 mm rods (Figure 1(B)). The application of the coupling was entirely tool-less. In Figure 2 more detail on undeployed wings (Figure 2(A)) and deployed wings (Figure 2(B)).
Fixator System B – AO external fixator
The AO (Arbeitsgemeinschaft für Osteosynthesefragen) Fixator system by Depuy Synthes (Synthes Holding AG, Solothurn, Switzerland) with the tradename ‘Large and medium External Fixator’ (Figure 1(C)) was used as the commercially available model for comparison. It had a modular clamp to rod-to-pin system with a clip-on self-holding mechanism made from titanium constructed for 5mm pins and 11 mm rods. An 11 mm combination wrench was used for tightening the clamp. This setup has been used in studies before.12
Pins, rods and bone model
Each fixator setup was constructed of four self-drilling half pins (Ø5 mm, 150 x 50 mm), model Apex by Stryker (Stryker GmbH, Selzach, Switzerland), which were driven into a synthetic bone (left femur with distal canal opening, Synbone, Switzerland. Length: 460 mm. Condylar width: 85 mm. Neck angle: 120°. Anteversion: 18°. Head diameter: 49 mm. Canal diameter: 10 mm) with a standard Cordless screwdriver (Model GSR 12V-15 PROFESSIONAL by Robert Bosch Power Tools GmbH, Leinfelden Echterdingen, Germany).
Figure 1 Comparison of both systems set up

Figure 2 Deployed and undeployed clamps

Subjects applying the systems
The system was applied by surgeons who were divided into three groups, each with eight subjects of varying surgical experience, resulting in a total of 24 surgeons:
- Group 1
Surgeons working in trauma surgery with 0–3 years of professional experience were described as residents with the lowest experience level. - Group 2
Surgeons with more than 3 years of experience in trauma surgery but without successful examination in ‘Special Trauma Surgery’ are described as fellows having a medium level of experience. - Group 3
Experienced surgeons in trauma surgery with the designation described as attendings.
Procedure for the application of the systems
One run with each fixator model was carried out per surgeon in a cross-over design according to ABBA scheme (Surgeon 1: fixator A followed by fixator B. Surgeon 2: fixator B followed by fixator A) to reduce bias due to a learning effect. The fixation was carried out in orientation on the standard principles of ASTM F1541.13 The surgeons were free to place their pins, sparing the area where the condyles were placed in a footing and the osteotomy zone. The time measurement was carried out from the placement of the pins in the bone to the completed placement of the connecting rods of the fixator and fully tightened clamps.
Once the fixator was in place, an oscillating saw was used to simulate an unstable transverse femoral shaft fracture according to AO 32A3(b), followed by mechanical testing.
Mechanical testing
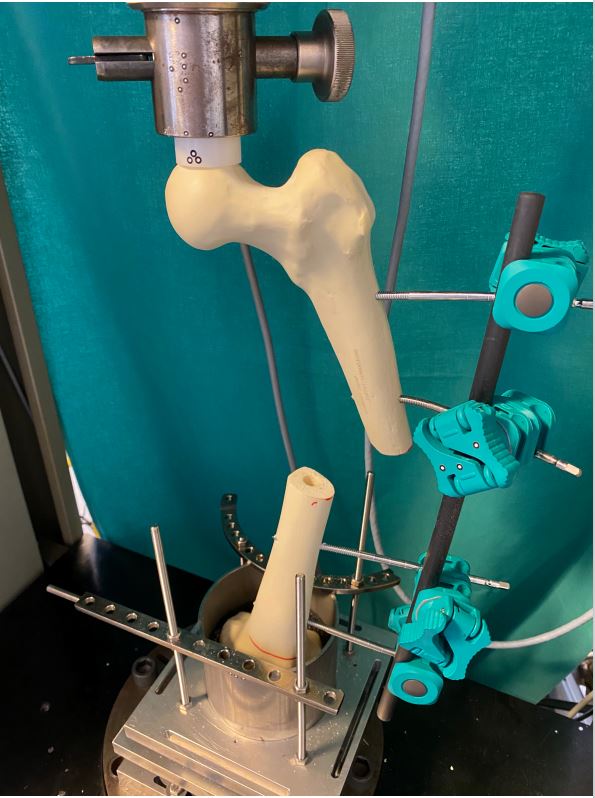
A simple quasi-static mechanical test was used to measure the stability of the individual surgeons’ setup. The static test was performed based on annex 7 of the ASTM F1541 [7], which describes a test method for the complete skeletal fixator-bone construct. Compared to the testing standard of external fixators, a test scenario was used to investigate the individual setup of the surgeons, as the focus was on the time needed to apply the system rather than implant it in a standardised fashion. The distance between the rod and point of force application was set to 155 mm while the individual pin placements were kept in place. The tests were performed with a Zwick Roell 1455 RetroLine (Zwick Roell AG, Ulm, Germany), which can be seen in the test setup in Figure 3. The setup was based on a biomechanical degree of freedom analysis of the human femur. The femoral head was able to rotate freely. The femoral condyle was mounted allowing no torsion but leaving 30 mm into anterior-posterior and lateral-medial direction. A maximum load of 150 Newtons was selected, corresponding to the approximate force due to the leg’s weight (18.5% of body weight14 for an average of 77 kg15).
For each test, two similar measurements were performed. The first measurement was performed to diminish the system’s slack due to the installation of the test. The second measurement was used as a basis for the comparison of both systems. The recording of the measurement started at 5 N. The table speed was set as 1 mm/s. After 150 N were reached, the load was reduced until 5 N were reached, and the recording stopped. The deformation was measured in mm. In Figure 3, both systems can be seen under load and without load.
The resulting failure rate was compared for fixator systems A and B. Failure was defined as the inability to withstand 150 N due to movements between connected parts and deformation. An example of a failed construct can be seen in Figure 4.
Figure 3 Comparison of Fixators under load
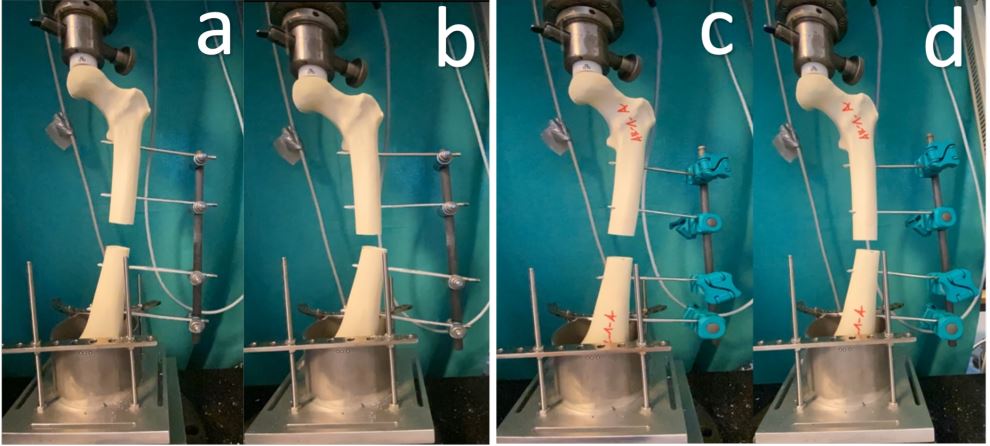
Figure 4 Clamp failure
Statistical methods
A direct comparison between groups was carried out regarding the fixator system first applied using a Chi-Square test. The overall time needed to apply the fixator system and the deformation during material testing were tested using a Wilcox Rank-Sum test. SAS statistical software was used for calculating the results.16
Results
In total, 24 surgeons divided into three groups of eight, with varying surgical experience (resident, fellow, attending), applied each external fixator system to one synthetic left femur, making up a total of 48 constructs that were tested.
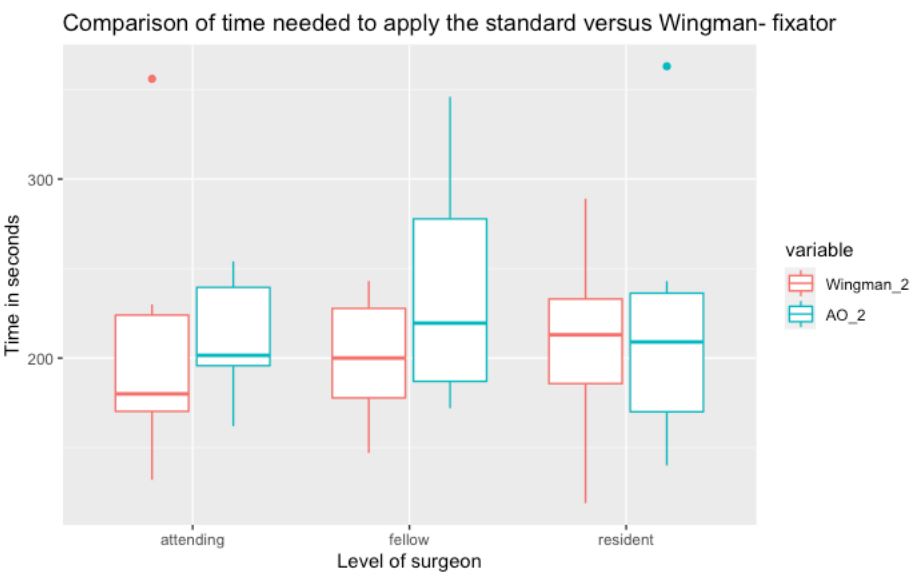
First, we measured the overall time needed for each surgeon to apply each system and compared the results. It showed no significant difference (p=0.06) in a Wilcox Rank-Sum test. When looking at it as a race with the system applied first as the winner and the system applied second as the looser, 16 out of 24 surgeons had the Wingman fixator applied before the AO system, making it significantly faster in comparison to the AO fixator (p=0.02) in a Chi-Square test.
A comparison of the time needed to apply both systems can be seen in Figure 5. A tendency of the Wingman fixator to be faster can be retraced graphically by comparing a steady reduction of median time needed to apply the system in comparison to the AO fixator.
One sample failed in each group of 24 setups, not reaching 150N of axial load during biomechanical testing. When deformation was compared, the Wilcox Rank-Sum test showed no statistically significant difference between both groups (p=0.33).
Discussion
Tool-less external fixators are currently not state-of-the-art in military and disaster applications. However, the developed system has some unique advantages due to the manual locking clamp mechanism.10 Especially in combat situations, in which time and weight optimisation is an asset, lightweight and quickly adaptable systems are preferable if they achieve equivalent results. Therefore, the study’s primary aim was to compare the performance of the novel tool-less system to the commercially available and established AO external fixator. The novel system showed equal failure rates when tested for stability while showing no inferiority when the time needed to set up either system was compared, in line with the Wingman’s goal to provide an intuitive handling while being safe to set up by novel users.
Numerous studies have explored possibilities to bypass the inherent obstacles of commercially available external fixators. For example, Landaeta et al. recently tested a 3D-printed clamp for external fixation following the ASTM standard F1541 showing that its biomechanical properties were comparable with other currently available external fixators.9 Similar to this study, a unilateral fixator with one rod was used.
Goh et al. took a similar approach to our setup, testing an AO external fixator to a novel low-cost fixator, not finding a statistically significant difference in stiffness.17
A tool-less external fixator named ‘Dolphix Temporary Fixation System’ was biomechanically evaluated in comparison to the Hoffmann III System by Stryker by Carpanen et al.10 The tool-less system exhibited 54 per cent of the strength of the Hoffmann system. In contrast to the Wingman clamp, the system needs one clamp for a pin-to-rod fixation and one for a rod-to-rod fixation, whereas the Wingman clamp can be used for both purposes. On top, the Dolphix system was not intended to be 3D printed.
Kouamé et al. tested a low-cost conventional external fixator compared to the Hoffmann III model by Stryker and found no inferiority of the low-cost system.11
An experimental setup comparing the time needed to apply different external fixator models could not be found. Kienast et al. compared the ‘plate to bone fit of manually bent reconstruction plates with two industrial pre-bent clavicle midshaft plates’ also using three differently experienced surgeons.19 Significant differences between the groups regarding the time needed for bending the plate could not be identified.
The Wingman clamp showed no inferiority to the AO system when it came to the time needed to apply it with equal failure rates. This proves its intention of needing no prior training when applied by any surgeon, no matter which system they had trained on.
While testing the application of both external fixator models, the participants noted that one advantage of the system is that a reposition of a fracture could be held while the fixator clamp could be single-handedly fastened. In clinical practice, holding reposition is usually done by one surgeon while the other surgeon fastens the clamps using special tools. In precarious situations during warfare, as currently reported by the WHO in the Ukraine,20 a system saving technical and personal resources can be beneficial.
A potential subject for further studies would be testing a modular external fixator system setup recommended by the AO21 using the Wingman external fixator clamp compared to a conventional external fixator clamp to see how it performs in more complex setups.
Limitations
In this study, a monotube system was applied and tested. Biomechanically, a double tube system has superior stability.22 As applicability was the focus of this study, only one tube was used.
As the surgeons knew which system they were using, a performance bias cannot be excluded due to preconceived notions or preferences for one system.
Despite a current global mismatch between the availability of 3D printing and demand for it in developing countries or regions of a humanitarian crisis, market potential is seen by Corsini et al. regarding supply chains, making the approach of the Wingman external fixator prospectively sustainable.23
Summary, conclusion and outlook
In this study, three groups of eight surgeons with different degrees of experience tested the performance of the novel tool-less external ‘Wingman’ fixator clamp in comparison, designed to be used during warfare and humanitarian crises, to a commercially available and established AO external fixator system. The novel system proved to be significantly faster to set up, not significantly less time consuming, with identical failure rates, pointing towards a superiority of the Wingman external fixator system.
The low amount of metal could allow MRI compatibility compared to conventional fixators, especially when glass fibre rods rather than metal tubes are used, yet this has to be evaluated and is subject to further projects.
Of all the objectives set initially, the cost factor could yet not be finally determined. The cost depends on the production scale and its possibility of decentralised production by 3D printing on demand wherever the external fixator is needed and will be subject to future projects.
Despite the intention to be used in a setting of limited medical infrastructure, the Wingman external fixator has the potential to be used in civilian circumstances due to MRI compatibility and overall good handling and performance. Its clinical implementation is the next step, possibly also in civilian use.
Corresponding Author: Jasper Frese, jasper.frese@yahoo.de
Authors: J Frese2, T Barth2, M Münch2, J Keller3, M Johann4, C Lutz5, AP Schulz2
Author Affiliations:
1 BG Klinikum Hamburg – Department of Traumaand Orthopaedic Surgery
2 BG Klinikum Hamburg – Centre for Clinical Research Hamburg
3 UKE – Department of Trauma and Orthopaedic Surgery Hamburg
4 Bundeswehrkrankenhaus Hamburg
5 Bluewater Medica


